2/
Physical examination was notable for:
▶️ BP 175/106
▶️ Flaccid paraparesis
▶️ Areflexia in the lower limbs
Physical examination was notable for:
▶️ BP 175/106
▶️ Flaccid paraparesis
▶️ Areflexia in the lower limbs
3/
Lumbar puncture was performed revealing:
▶️White blood cell count 1
▶️Protein 41
▶️Glucose 88
▶️Negative oligoclonal bands
He was diagnosed with "idiopathic transverse myelitis" and treated with IV methylprednisolone x 5 days and subsequently 5 sessions of plasma exchange.
Lumbar puncture was performed revealing:
▶️White blood cell count 1
▶️Protein 41
▶️Glucose 88
▶️Negative oligoclonal bands
He was diagnosed with "idiopathic transverse myelitis" and treated with IV methylprednisolone x 5 days and subsequently 5 sessions of plasma exchange.
6/
In this case, our patient's symptoms progressed to maximal deficit in just a few hours.
Remember, hyperacute presentations (<12 hours) of severe myelopathy should bring vascular myelopathy etiologies (e.g. spinal cord infarction) to the top of the differential.
In this case, our patient's symptoms progressed to maximal deficit in just a few hours.
Remember, hyperacute presentations (<12 hours) of severe myelopathy should bring vascular myelopathy etiologies (e.g. spinal cord infarction) to the top of the differential.
7/
Spinal cord infarction (SCI) is an extremely underrecognized cause of acute myelopathy, as highlighted by my friend and mentor @nzalewski2 in what I consider this truly seminal piece of literature.
jamanetwork.com
Spinal cord infarction (SCI) is an extremely underrecognized cause of acute myelopathy, as highlighted by my friend and mentor @nzalewski2 in what I consider this truly seminal piece of literature.
jamanetwork.com
8/
While patient's may have typical vascular risk factors (e.g., HTN, HLD, DM2), not all do and SCI can occur at any age.
A large proportion of SCIs are also caused by aortic dissection or fibrocartilaginous embolism.
While patient's may have typical vascular risk factors (e.g., HTN, HLD, DM2), not all do and SCI can occur at any age.
A large proportion of SCIs are also caused by aortic dissection or fibrocartilaginous embolism.
10/
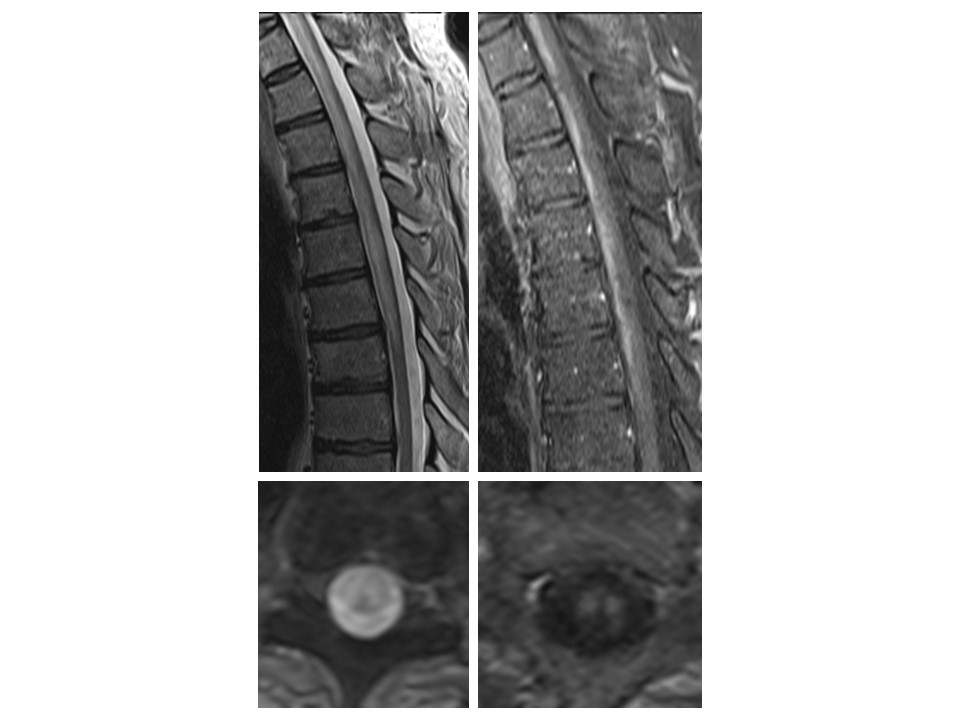
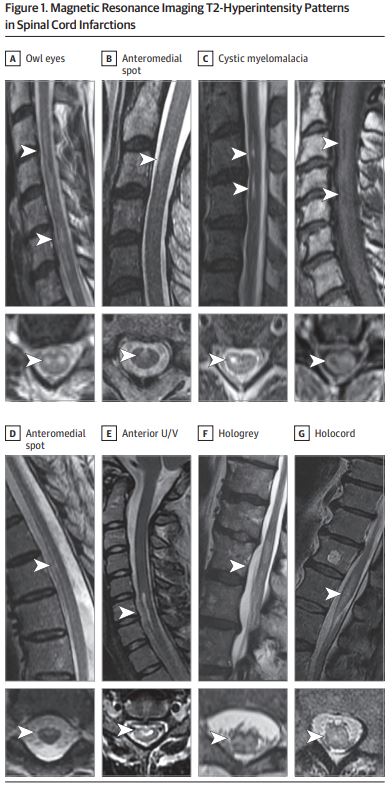
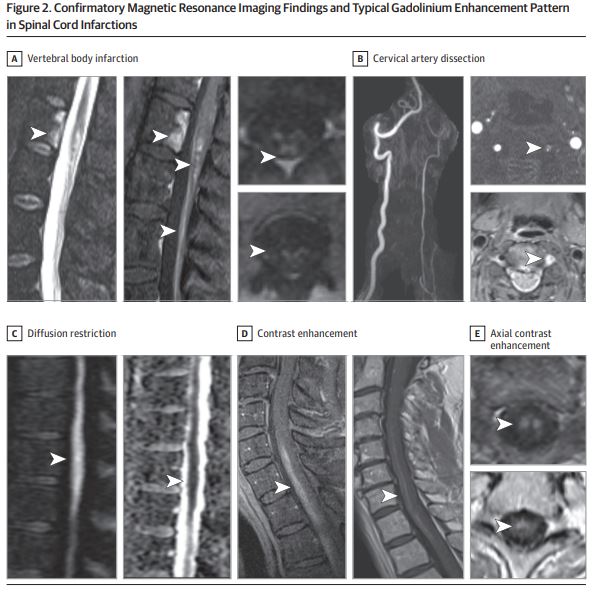
Other common T2-hyperintense patterns are highlighted well in @nzalewski2's paper as shown below.
Other common T2-hyperintense patterns are highlighted well in @nzalewski2's paper as shown below.
12/
In terms of treatment, once acute spinal cord infarction is suspected consider:
▶️IV thrombolytics if within the typical window for acute ischemic stroke
and/or:
▶️Lumbar drain with blood pressure augmentation to increase spinal cord perfusion.
sciencedirect.com
In terms of treatment, once acute spinal cord infarction is suspected consider:
▶️IV thrombolytics if within the typical window for acute ischemic stroke
and/or:
▶️Lumbar drain with blood pressure augmentation to increase spinal cord perfusion.
sciencedirect.com
13/
Afterwards,
Similar to cerebral infarcts, explore potential mechanisms for SCI and optimize/treat vascular risk factors.
Afterwards,
Similar to cerebral infarcts, explore potential mechanisms for SCI and optimize/treat vascular risk factors.
14/
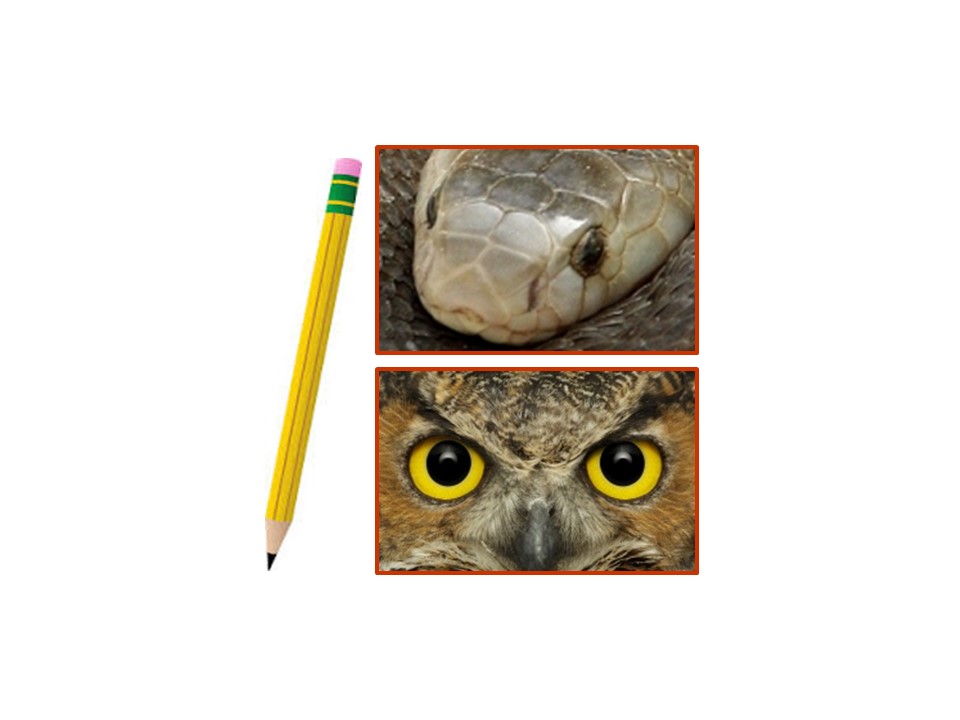
Key takeaways:
▶️Hyperacute myelopathy (<12 hours) ➡️ think SCI
▶️Recognize key imaging findings (pencil, owl eyes)
▶️Treatment is focused on increasing spinal cord perfusion
Key takeaways:
▶️Hyperacute myelopathy (<12 hours) ➡️ think SCI
▶️Recognize key imaging findings (pencil, owl eyes)
▶️Treatment is focused on increasing spinal cord perfusion
Loading suggestions...