2/ Shankar, her husband has diagnosed with cirrhosis just a two months ago
At the time, he had swelling of both feet and an evaluation revealed low platelets and features of cirrhosis on imaging
Absolutely no complications of cirrhosis
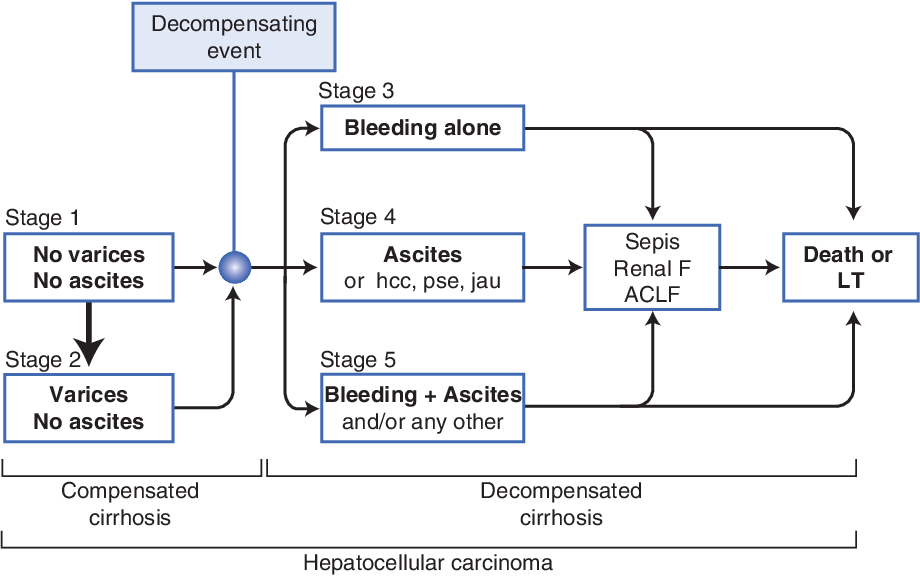
Complications of cirrhosis come in stages
At the time, he had swelling of both feet and an evaluation revealed low platelets and features of cirrhosis on imaging
Absolutely no complications of cirrhosis
Complications of cirrhosis come in stages
4/ In stages beyond these, patients develop features of liver failure - such as jaundice (defined as bilirubin levels > 3mg/dL)
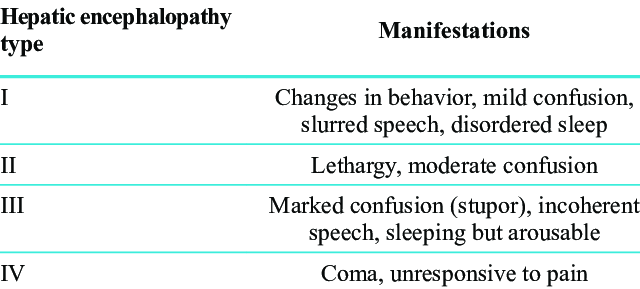
and brain failure (called hepatic encephalopathy or HE)
In natural history of the cirrhosis, HE happens in advanced stages and predicts early death
and brain failure (called hepatic encephalopathy or HE)
In natural history of the cirrhosis, HE happens in advanced stages and predicts early death
7/ reason for precipitation of HE
In the ER, Shankar was being put on the ventilator because he is in a coma and chances of aspiration of saliva into his lungs was very high and lung failure was very high
They were small, loving, close knit family
Father, mother and daughter
In the ER, Shankar was being put on the ventilator because he is in a coma and chances of aspiration of saliva into his lungs was very high and lung failure was very high
They were small, loving, close knit family
Father, mother and daughter
8/ Their daughter was 22 years old, engaged to a gentleman and wedding was planned in three months
After the engagement, her father was diagnosed with cirrhosis and within two months of his diagnosis, he was admitted thrice with HE
And now in a coma, she was worried...
After the engagement, her father was diagnosed with cirrhosis and within two months of his diagnosis, he was admitted thrice with HE
And now in a coma, she was worried...
9/ that she would end up on wedding day, without her beloved Appa
My colleagues take a detailed history - Shankar was a teetotaler, a sweet man who followed doctors orders to the T and worked hard to make ends meet
He was overweight
No drug use apart from what was prescribed
My colleagues take a detailed history - Shankar was a teetotaler, a sweet man who followed doctors orders to the T and worked hard to make ends meet
He was overweight
No drug use apart from what was prescribed
10/ The first time he got sick, it started off with him mistaking the living room for the bathroom and was readying himself to urinate on the living room floor
Disoriented and confused, he was rushed to a nearby hospital where he was diagnosed with HE and treated accordingly
Disoriented and confused, he was rushed to a nearby hospital where he was diagnosed with HE and treated accordingly
11/ The second HE attack came after 3 weeks - this time, he was disoriented while riding his bike and crashed onto a pole very close to his home
No brain injuries, and again, treatment for HE improved his condition and he was taken home
The third time, he went into a coma...
No brain injuries, and again, treatment for HE improved his condition and he was taken home
The third time, he went into a coma...
12/ in front of my eyes
Time was running out and we had to find what was causing his recurrent brain failure
To make things worse, his liver functions were perfect and his cirrhosis was in stage 2 - HE is not expected in this supposedly stable stage
What was causing it?
Time was running out and we had to find what was causing his recurrent brain failure
To make things worse, his liver functions were perfect and his cirrhosis was in stage 2 - HE is not expected in this supposedly stable stage
What was causing it?
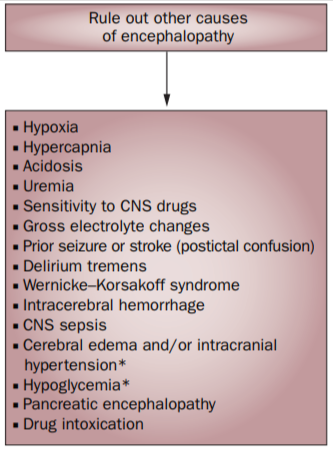
13/ When a patient with stable cirrhosis, presents with recurrent brain failure in the absence of identifiable causes for precipitation of HE it is called "spontaneous HE"
As we wait for the blood reports, we also send Shankar for a CT scan of the abdomen
This would help us...
As we wait for the blood reports, we also send Shankar for a CT scan of the abdomen
This would help us...
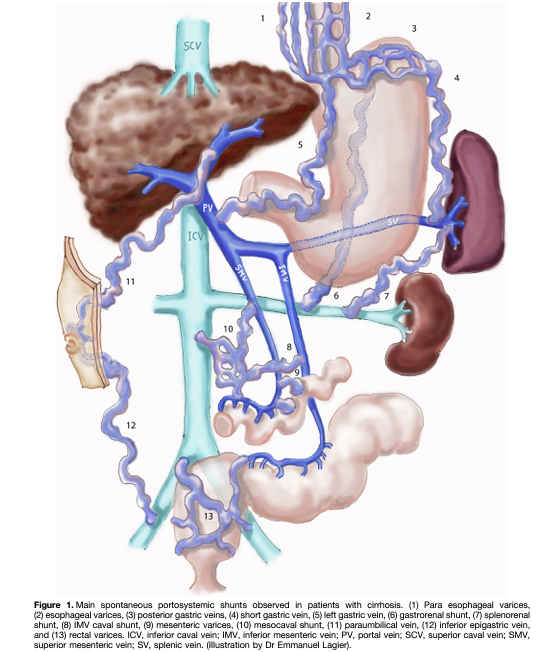
14/ identify an important cause for his supposed recurrent spontaneous HE
This is called as portosystemic shunts
Portosystemic shunts are LARGE blood vessels that form inside the abdomen in cirrhosis, when the liver pressure increases as the liver shrinks
When liver shrinks...
This is called as portosystemic shunts
Portosystemic shunts are LARGE blood vessels that form inside the abdomen in cirrhosis, when the liver pressure increases as the liver shrinks
When liver shrinks...
15/ the pressure inside the liver increases and blood flow into the liver gets difficult
But blood has to flow around
Akin to a block on the highway and how vehicles take the bypass and service roads, for the blood to flow, new large blood vessels form which bypass the liver
But blood has to flow around
Akin to a block on the highway and how vehicles take the bypass and service roads, for the blood to flow, new large blood vessels form which bypass the liver
17/ In Shankar's case, we did not find any shunts and hence, large PSS as a cause for brain failure was ruled out
Meanwhile, the blood reports come
And everything was normal
Except two small things
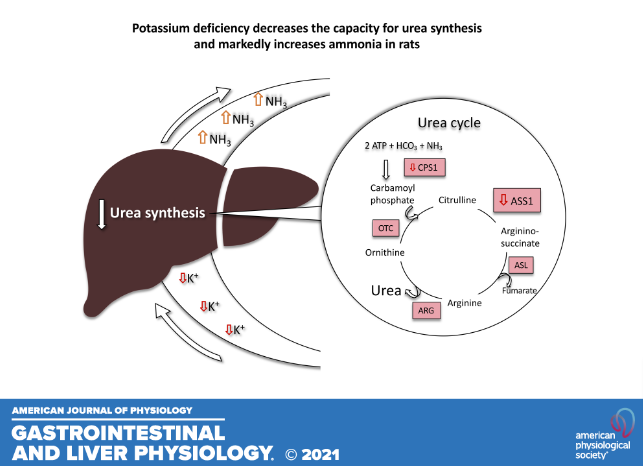
Potassium levels - this was very low in Shankar
Ammonia - was raised
Meanwhile, the blood reports come
And everything was normal
Except two small things
Potassium levels - this was very low in Shankar
Ammonia - was raised
20/ Correct potassium levels and Shankar will be fine
So we start potassium correction for Shankar and tell his wife and daughter that, things are going to be well
But we did not yet, have the reason for Shankar's recurrent brain failure
So we ask the family about reasons...
So we start potassium correction for Shankar and tell his wife and daughter that, things are going to be well
But we did not yet, have the reason for Shankar's recurrent brain failure
So we ask the family about reasons...
21/ doctors who treated Shankar for the first and second attacks of brain failure gave them
'High ammonia', says his wife
'But potassium was also low Amma', says his daughter
I sit up, listen & ask, ' Both times?'
& they nod
'Can I see the discharge summaries'? I ask them
'High ammonia', says his wife
'But potassium was also low Amma', says his daughter
I sit up, listen & ask, ' Both times?'
& they nod
'Can I see the discharge summaries'? I ask them
22/ And we see something intriguing.
Shankar, during all his three attacks of brain failure had low potassium levels
This meant that not only he had recurrent HE, but he also had recurrent hypokalemia every time that gave rise to HE
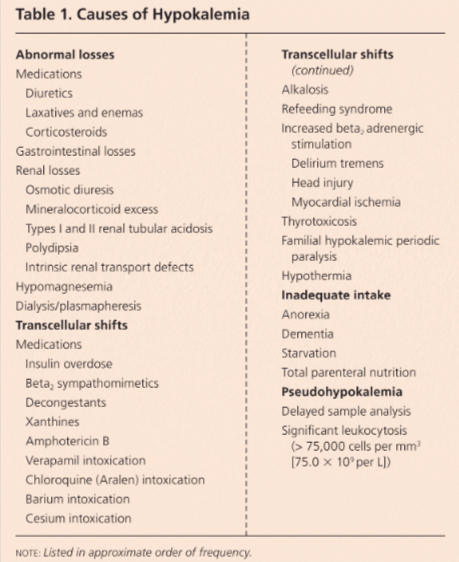
Why was his potassium going low repeatedly?
Shankar, during all his three attacks of brain failure had low potassium levels
This meant that not only he had recurrent HE, but he also had recurrent hypokalemia every time that gave rise to HE
Why was his potassium going low repeatedly?
26/ Following this pattern, we find that in Shankar...
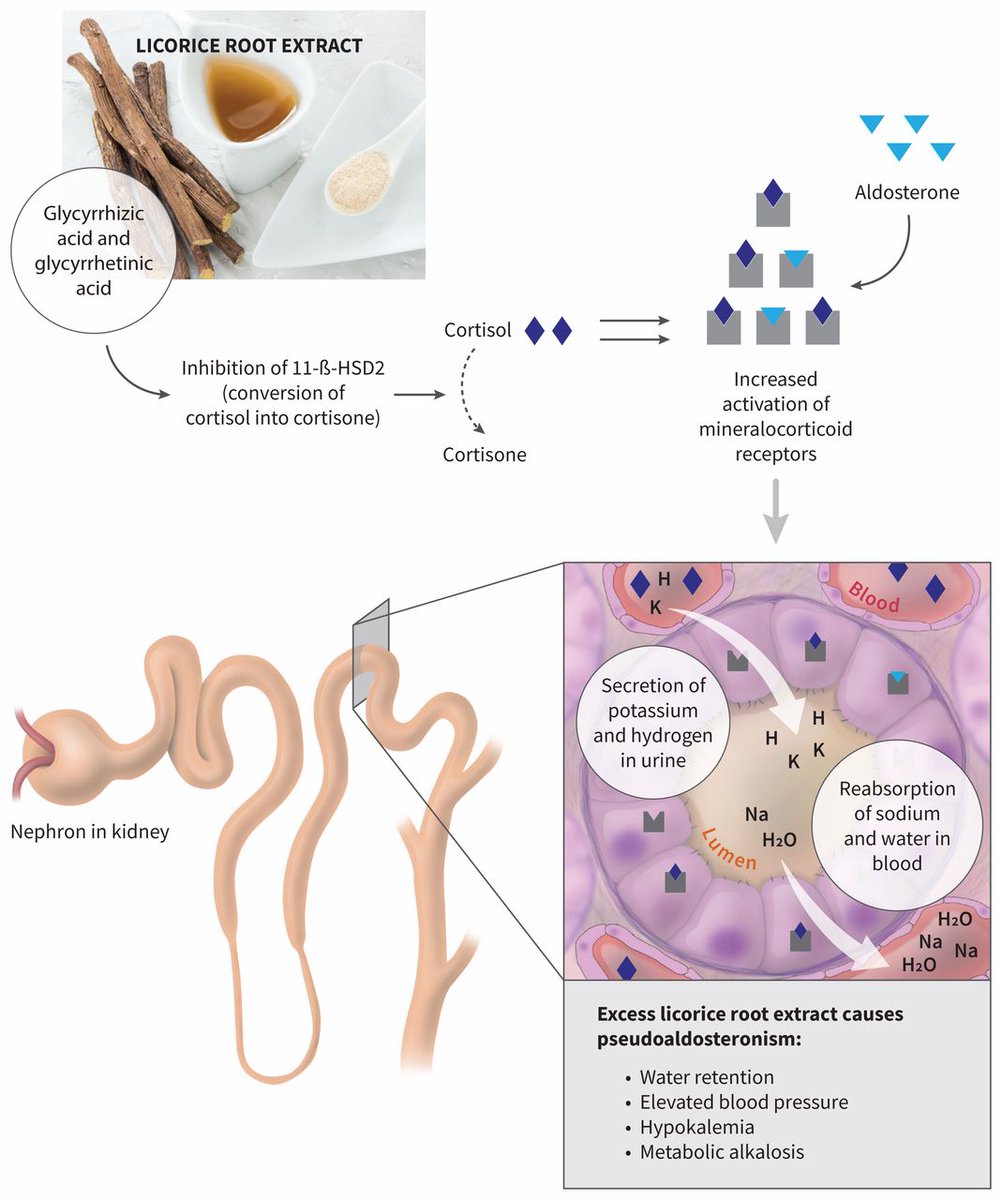
Urine potassium was was high and his blood was alkaline (called metabolic alkalosis)
His admission blood pressures were on the higher side and this was true for every prior admission
And major potassium handling hormone,
Urine potassium was was high and his blood was alkaline (called metabolic alkalosis)
His admission blood pressures were on the higher side and this was true for every prior admission
And major potassium handling hormone,
27/ called aldosterone, secreted by adrenal glands was low
This was strange
Low potassium
High blood pressure
Alkaline blood
All were common at every admission
High aldosterone levels can cause these
But Shankar had low aldosterone levels
This was called..
This was strange
Low potassium
High blood pressure
Alkaline blood
All were common at every admission
High aldosterone levels can cause these
But Shankar had low aldosterone levels
This was called..
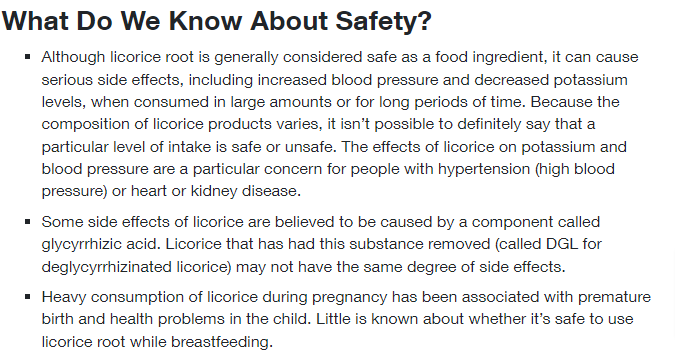
31/ So we get back to the wife and daughter and ask them his dietary habits and they deny excessive use of
Licorice
Any other steroidal drugs
Grapefruits
Now we were truly lost
Without finding the cause of hypokalemia, Shankar was still at risk for brain failure because he..
Licorice
Any other steroidal drugs
Grapefruits
Now we were truly lost
Without finding the cause of hypokalemia, Shankar was still at risk for brain failure because he..
32/ was a cirrhosis patient and the chances of him getting through to attend his daughters wedding seemed very bleak
This depressed us and we did not know how to get through it
One day, while I was in the OPD, the staff comes in and tells me that Shankar's wife wanted to see me
This depressed us and we did not know how to get through it
One day, while I was in the OPD, the staff comes in and tells me that Shankar's wife wanted to see me
33/ I allowed her the time because I knew that we did everything we could to get to the root cause.
Even though Shankar would improve and get discharged from this episode (he was getting better on the ventilator, showing signs of waking up), we were not sure about his future.
Even though Shankar would improve and get discharged from this episode (he was getting better on the ventilator, showing signs of waking up), we were not sure about his future.
34/ The wife walks in and looks at me and I compose myself to apologize to her, because we thought we could do it, but we failed her too.
She speaks. 'Doctor, I thought long about the diet queries you asked me. And even though he did not consume any of those fruits you...
She speaks. 'Doctor, I thought long about the diet queries you asked me. And even though he did not consume any of those fruits you...
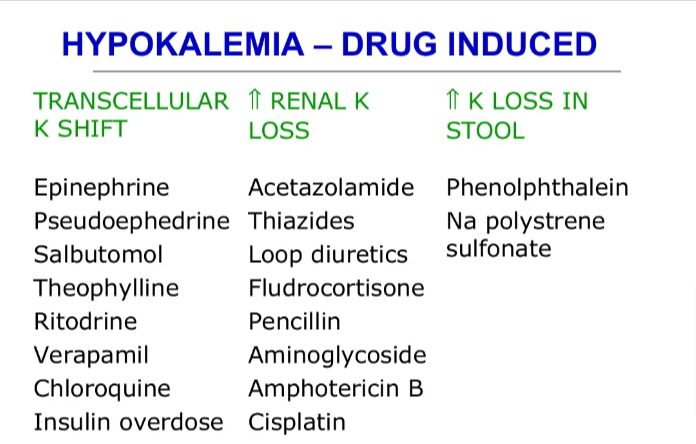
35/ mentioned, he was taking some laxative powder.'
I sit up and ask her the name of the powder
She says she did not know, because he kept it inside the bathroom shelf & she never looked at it.
Cirrhosis patients are usually prescribed lactulose - a safe laxative that helps..
I sit up and ask her the name of the powder
She says she did not know, because he kept it inside the bathroom shelf & she never looked at it.
Cirrhosis patients are usually prescribed lactulose - a safe laxative that helps..
36/ pass soft stools and also reduces ammonia
Lactulose did not suit Shankar - because a common side effect is excessive bloating and hence he went for some other laxative option, the name only he knew
'Only he can tell us and for that he has to be weaned off the ventilator'..
Lactulose did not suit Shankar - because a common side effect is excessive bloating and hence he went for some other laxative option, the name only he knew
'Only he can tell us and for that he has to be weaned off the ventilator'..
38/ more than a week to get to our goal, we finally wean off Shankar from the ventilator
His voice is raspy and he is weak
His swallowing is affected and he is dazed
The critical care nursing team do an intense job on rehabilitating him from speech, swallow and nutritional..
His voice is raspy and he is weak
His swallowing is affected and he is dazed
The critical care nursing team do an intense job on rehabilitating him from speech, swallow and nutritional..
39/ point of view.
And after another week in the ICU, Shankar is finally shifted out to the room
His potassium levels are fine
His blood pressures are fine
His blood is no more alkaline
And that day finally came, when on rounds, I could ask him about the powder he was having.
And after another week in the ICU, Shankar is finally shifted out to the room
His potassium levels are fine
His blood pressures are fine
His blood is no more alkaline
And that day finally came, when on rounds, I could ask him about the powder he was having.
42/ The problem with Kayam Churnam and products that contain Senna laxatives is that they reach a threshold and then they do not work, unless doses are increased
Across 2 months of daily use, Shankar had slowly & steadily increased Kayam use which led to severe potassium loss..
Across 2 months of daily use, Shankar had slowly & steadily increased Kayam use which led to severe potassium loss..
44/ After spending almost three weeks in the hospital, Shankar was finally discharged home
Back home, first thing he did was throw away Kayam Churnam out the window
Shankar teary eyed, watched his daughter dance with her husband on the day of her wedding
He sent me a message..
Back home, first thing he did was throw away Kayam Churnam out the window
Shankar teary eyed, watched his daughter dance with her husband on the day of her wedding
He sent me a message..
Loading suggestions...