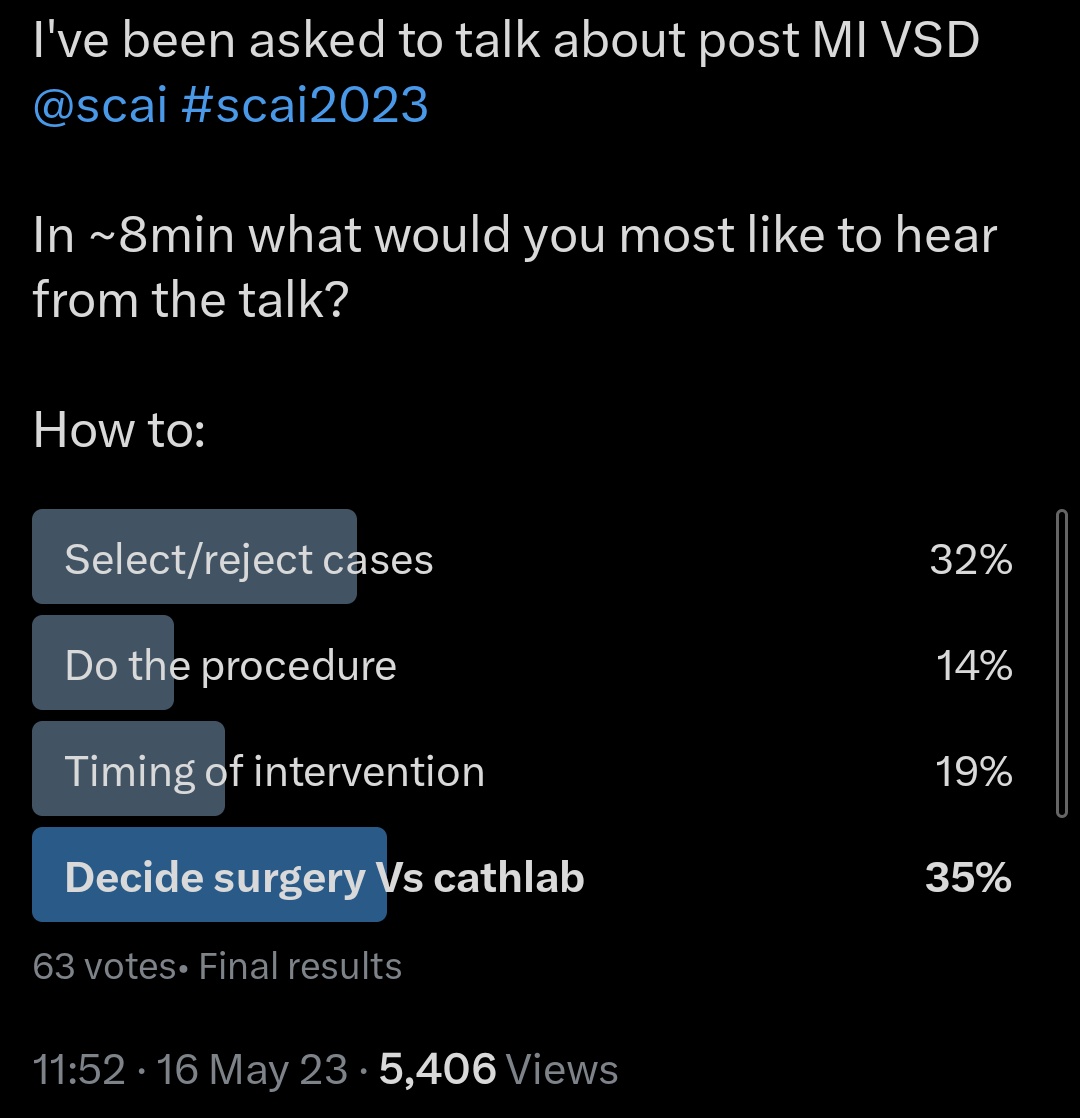
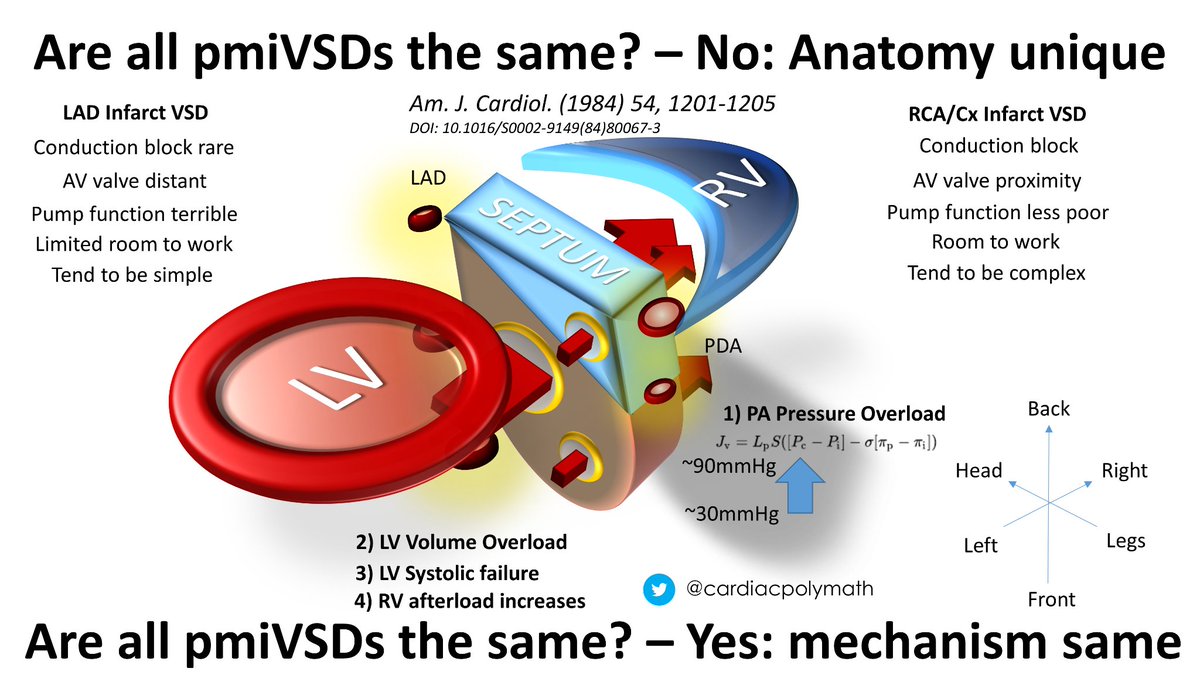
I was asked to talk about post myocardial infarction VSD for #SCAI2023 recently. In 8 mins I was a bit limited, so here's an expanded thread
Apologies that the movie compression makes things a bit jumpy, & if Twitter messes up the movie cropping I will add again at the end
1/
Apologies that the movie compression makes things a bit jumpy, & if Twitter messes up the movie cropping I will add again at the end
1/
What then?
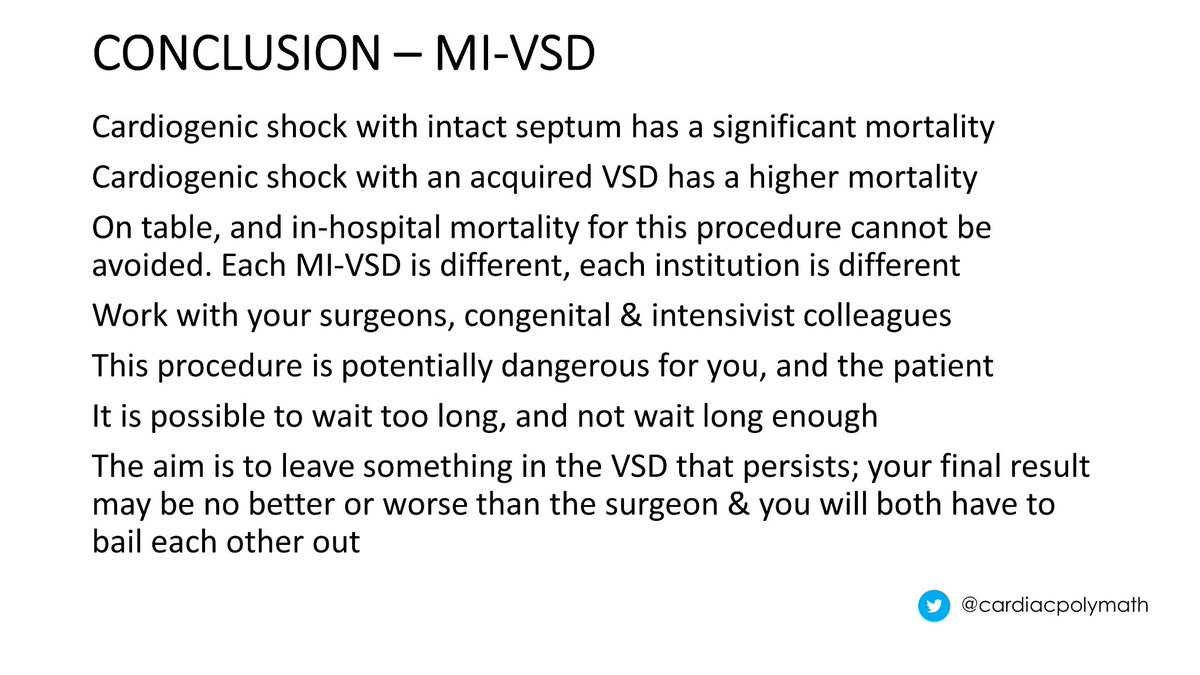
Surgery or a hybrid approach like @AdamGreenbaumMD BASSINET to use devices anchored with sutures through the myocardium agnostic to the VSD tract
I have not seen/heard of many centers offering this, but the article interest continues to grow - so one to watch?
15/
Surgery or a hybrid approach like @AdamGreenbaumMD BASSINET to use devices anchored with sutures through the myocardium agnostic to the VSD tract
I have not seen/heard of many centers offering this, but the article interest continues to grow - so one to watch?
15/
Loading suggestions...