Handout from our Endocrinology episode, "Episode 33: Hypercalcemia" with Dr. OP Hamnvik @ohamnvik is now out!
📝Download it free here: #hypercalcemia" target="_blank" rel="noopener" onclick="event.stopPropagation()">runthelistpodcast.com
🎶Episode: apple.co
check out👇for a #tweetorial on PTH-dependent & PTH-independent causes of hyperCa
📝Download it free here: #hypercalcemia" target="_blank" rel="noopener" onclick="event.stopPropagation()">runthelistpodcast.com
🎶Episode: apple.co
check out👇for a #tweetorial on PTH-dependent & PTH-independent causes of hyperCa
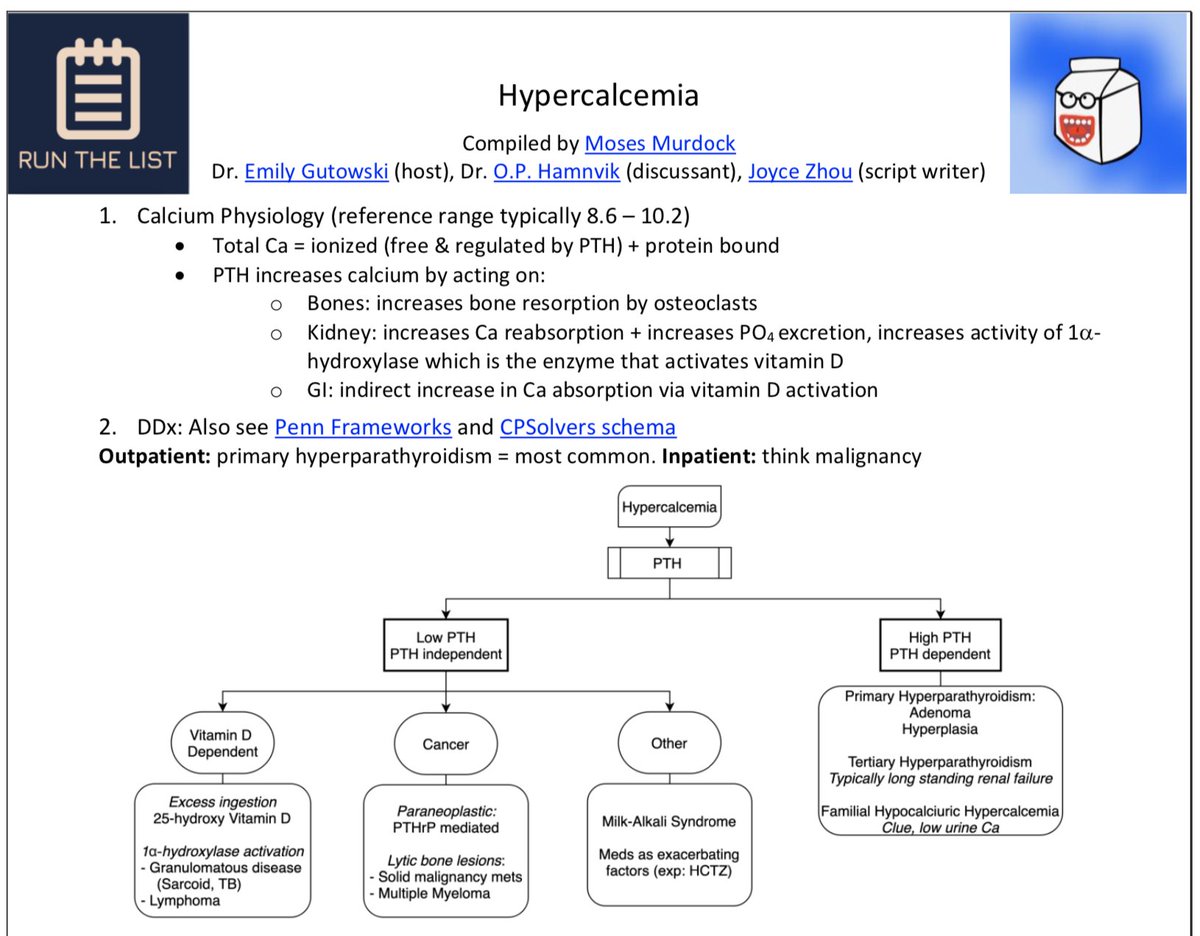
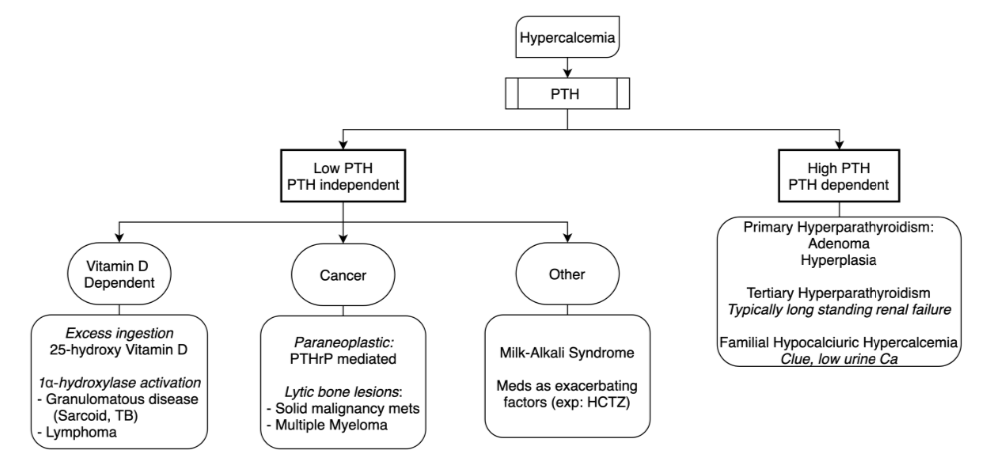
Finally, we arrive at the causes of hypercalcemia
@ohamnvik teaches us to think in TWO major buckets:
1⃣PTH-dependent
2⃣PTH-independent
@haematognomist made this nice framework 👇
2 more frameworks @PennMedicine & @CPSolvers: med.upenn.edu
clinicalproblemsolving.com
@ohamnvik teaches us to think in TWO major buckets:
1⃣PTH-dependent
2⃣PTH-independent
@haematognomist made this nice framework 👇
2 more frameworks @PennMedicine & @CPSolvers: med.upenn.edu
clinicalproblemsolving.com
[*Spoiler alert*]
for more on TUMS-induced hypercalcemia (i.e. Milk Alkali Syndrome) check out Episode 79 from our friends at @CPSolvers & case presenter @AnandJag1:
clinicalproblemsolving.com
for more on TUMS-induced hypercalcemia (i.e. Milk Alkali Syndrome) check out Episode 79 from our friends at @CPSolvers & case presenter @AnandJag1:
clinicalproblemsolving.com
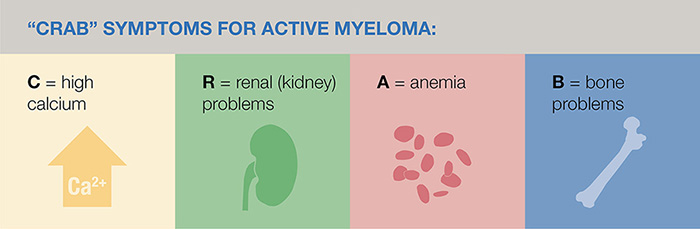
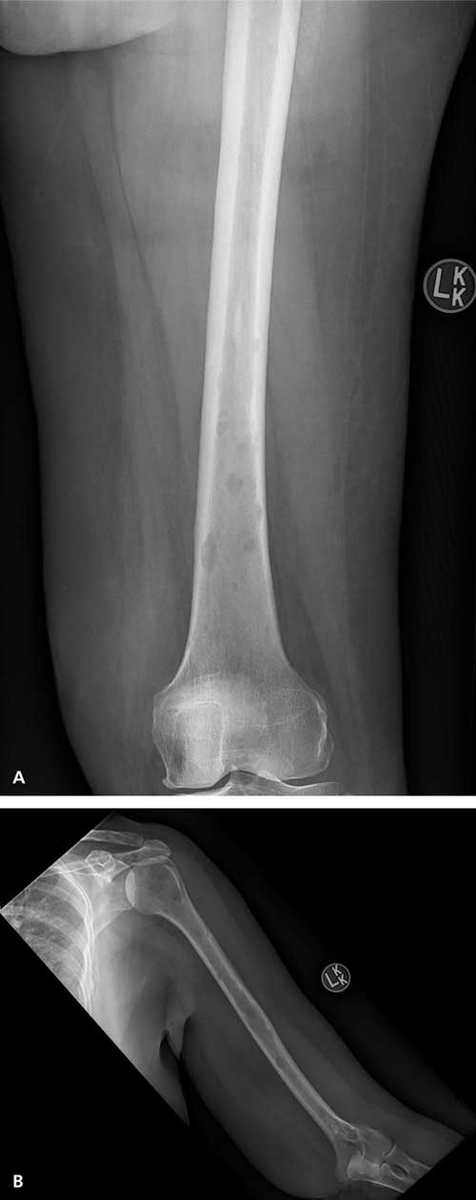
reminder that in Multiple Myeloma the "C" in CRAB criteria = hyperCalcemia
hypercalcemia = secondary to the lytic bone lesions seen w/ MM
for more clinical practice w/ hyperCa in malignancy:
VMR 52 w/ @tmodarressi: clinicalproblemsolving.com
VMR 63: clinicalproblemsolving.com
[10]
hypercalcemia = secondary to the lytic bone lesions seen w/ MM
for more clinical practice w/ hyperCa in malignancy:
VMR 52 w/ @tmodarressi: clinicalproblemsolving.com
VMR 63: clinicalproblemsolving.com
[10]
@ohamnvik reminds us that we can see hyperCa in the absence of any symptoms!
typically start to see sx at ~11.5 mg/dL, severe sx >13 mg/dL
Remember the "classic" hyperCa sx (see image👇)
*HyperCa can precipitate nephrogenic diabetes insipidus (NDI) -> polyuria, & pancreatitis
typically start to see sx at ~11.5 mg/dL, severe sx >13 mg/dL
Remember the "classic" hyperCa sx (see image👇)
*HyperCa can precipitate nephrogenic diabetes insipidus (NDI) -> polyuria, & pancreatitis
Alas, we're nearing the end... How about a quick quiz to test your knowledge?
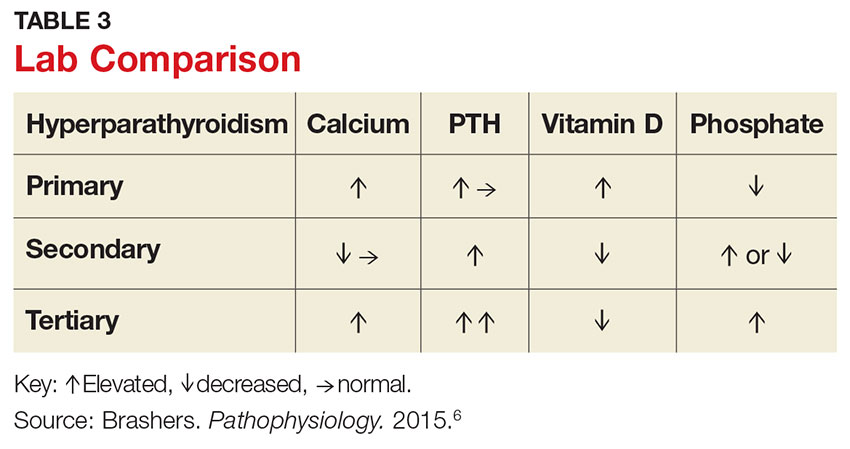
in PRIMARY hyperparathyroidism, what are the typical labs?
in PRIMARY hyperparathyroidism, what are the typical labs?
to recap:
Primary hyperparathyroidism: ⬆️/nl PTH, ⬆️Ca, ⬇️phos
Tertiary hyperparathyroidism: ⬆️⬆️ PTH, ⬆️Ca, ⬆️phos (due to ESRD)
mdedge.com
Primary hyperparathyroidism: ⬆️/nl PTH, ⬆️Ca, ⬇️phos
Tertiary hyperparathyroidism: ⬆️⬆️ PTH, ⬆️Ca, ⬆️phos (due to ESRD)
mdedge.com
For more on clinical presentation, management, case discussion, and other clinical pearls, be sure to check out Episode 33: Hypercalcemia with Dr. OP Hamnvik!
(sneak peek: he'll be back tomorrow for a Hypocalcemia episode!)
apple.co
(sneak peek: he'll be back tomorrow for a Hypocalcemia episode!)
apple.co
IN SUM:
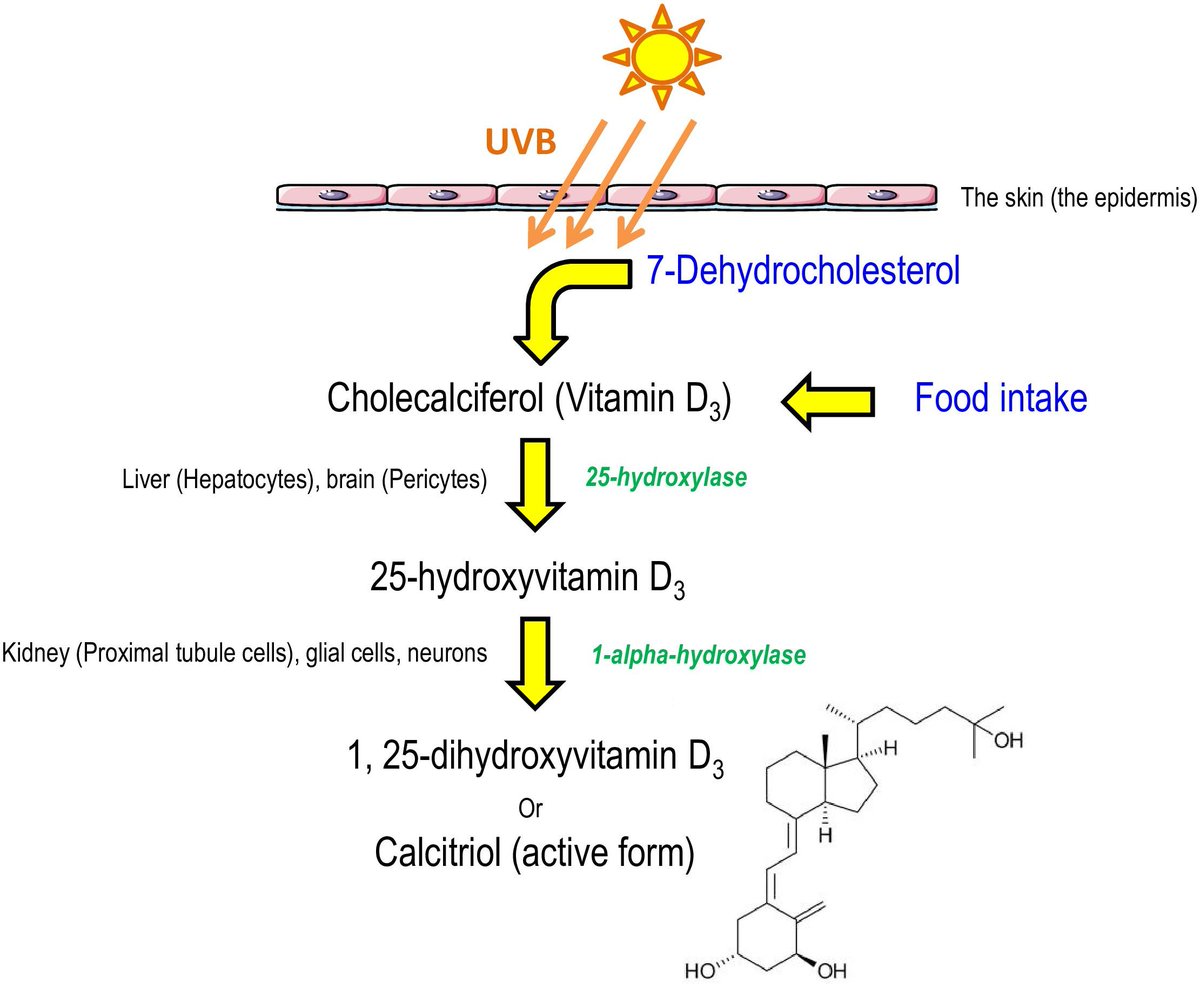
-Ionized = "free" Ca, which controls PTH level
-Ca sensed in parathyroid Chief cells by CaSR
-CaSR LoF mut. -> FHH
-PTH -> ⬆️Ca, ⬆️active vit. D, ⬇️phos
-HyperCa causes: PTH-dependent (primary, tertiary) & -independent (cancer, vit. D, other)
#hypercalcemia" target="_blank" rel="noopener" onclick="event.stopPropagation()">runthelistpodcast.com
-Ionized = "free" Ca, which controls PTH level
-Ca sensed in parathyroid Chief cells by CaSR
-CaSR LoF mut. -> FHH
-PTH -> ⬆️Ca, ⬆️active vit. D, ⬇️phos
-HyperCa causes: PTH-dependent (primary, tertiary) & -independent (cancer, vit. D, other)
#hypercalcemia" target="_blank" rel="noopener" onclick="event.stopPropagation()">runthelistpodcast.com
REFs:
[1]uclahealth.org
[2]nejm.org
[3]proteinatlas.org
[4]nature.com
[5]youtube.com
[6]nature.com
[7]frontiersin.org
[8]sciencedirect.com
[9]jasn.asnjournals.org
10]aafp.org
[1]uclahealth.org
[2]nejm.org
[3]proteinatlas.org
[4]nature.com
[5]youtube.com
[6]nature.com
[7]frontiersin.org
[8]sciencedirect.com
[9]jasn.asnjournals.org
10]aafp.org
Loading suggestions...