1/ Gooood morning, #MedTwitter! It’s time for another round of #12LeadThursday.
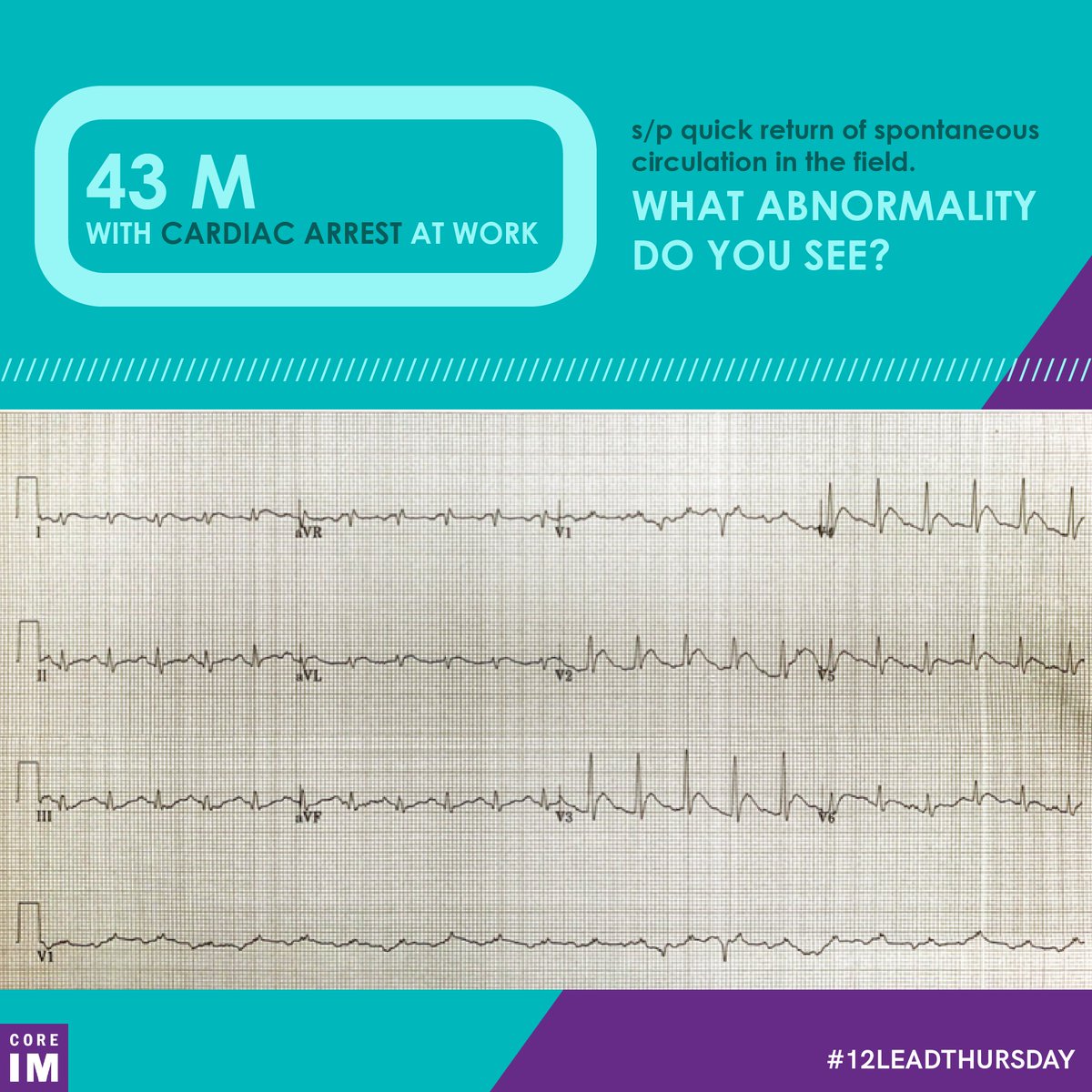
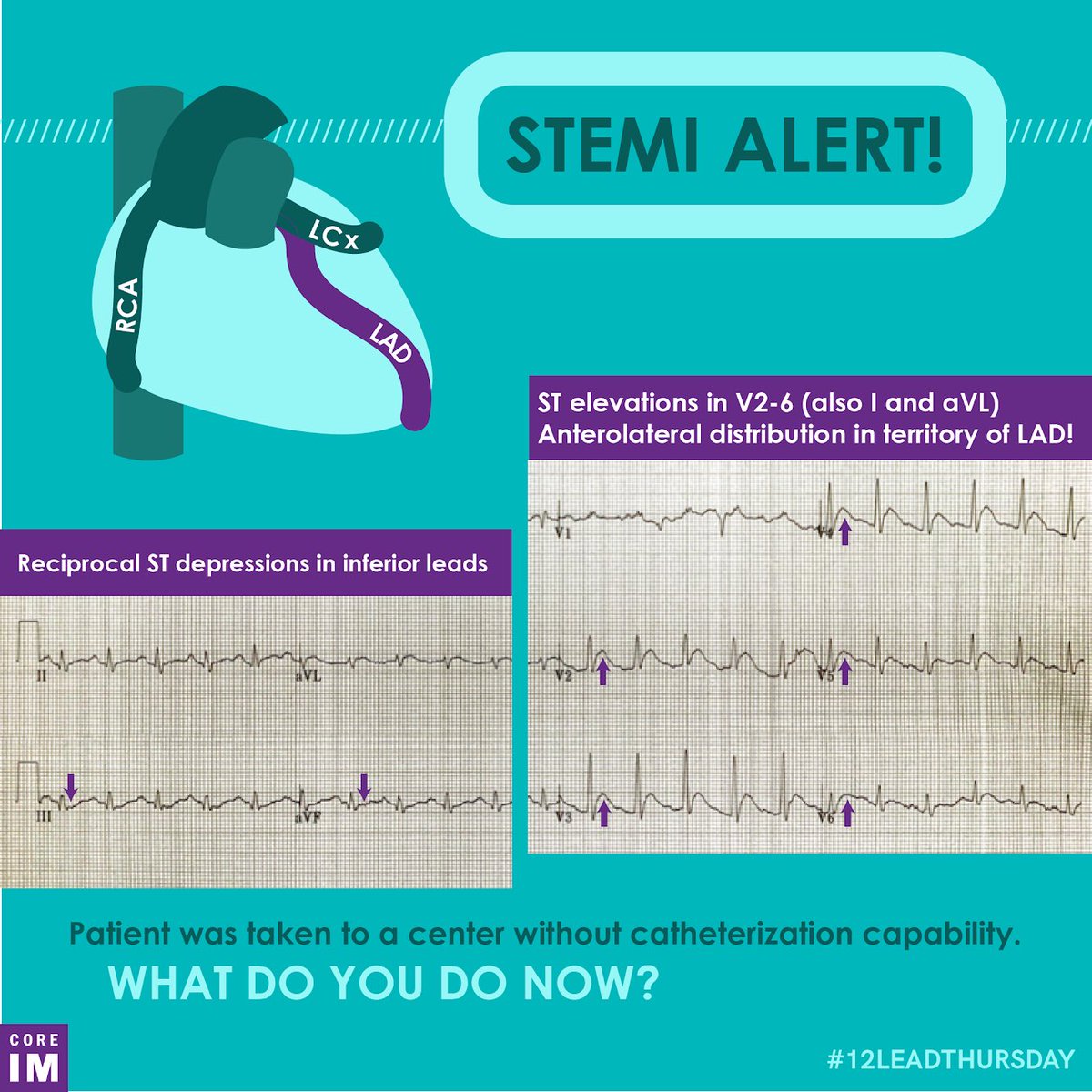
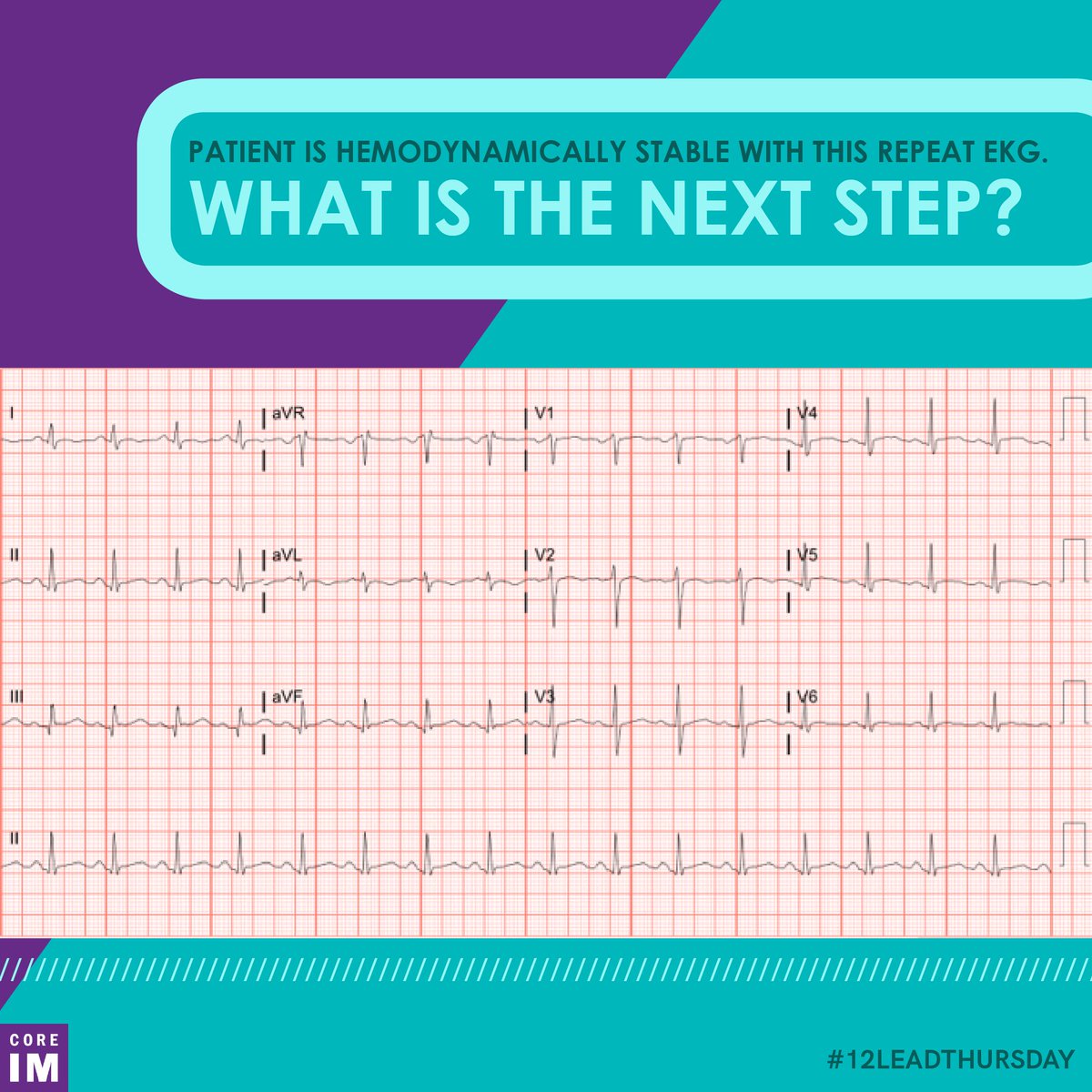
Remember to approach every ECG systematically. Use your system now - this 43 y/o patient had a cardiac arrest in the field and this is his EKG post-ROSC.
What’s going on?
Remember to approach every ECG systematically. Use your system now - this 43 y/o patient had a cardiac arrest in the field and this is his EKG post-ROSC.
What’s going on?
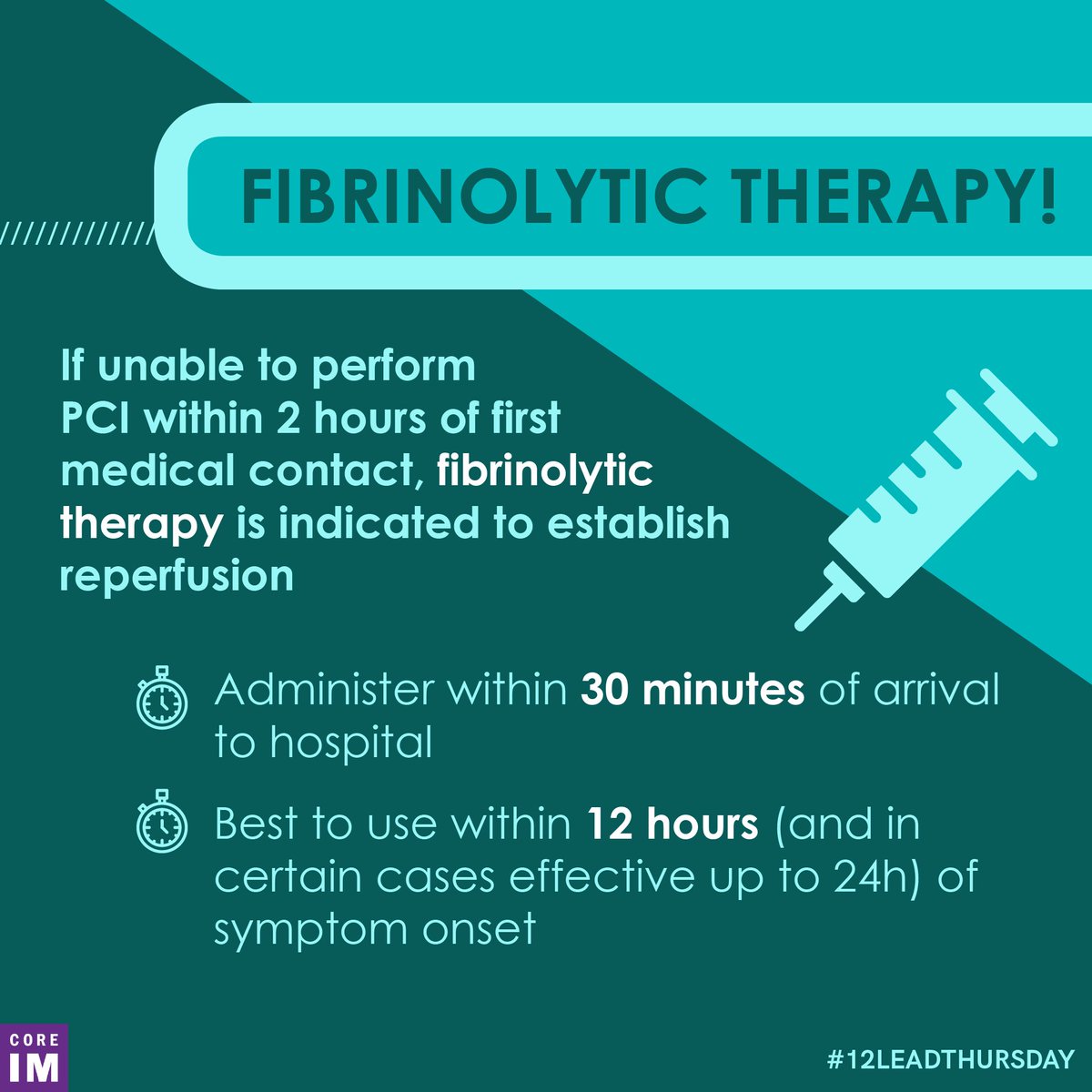
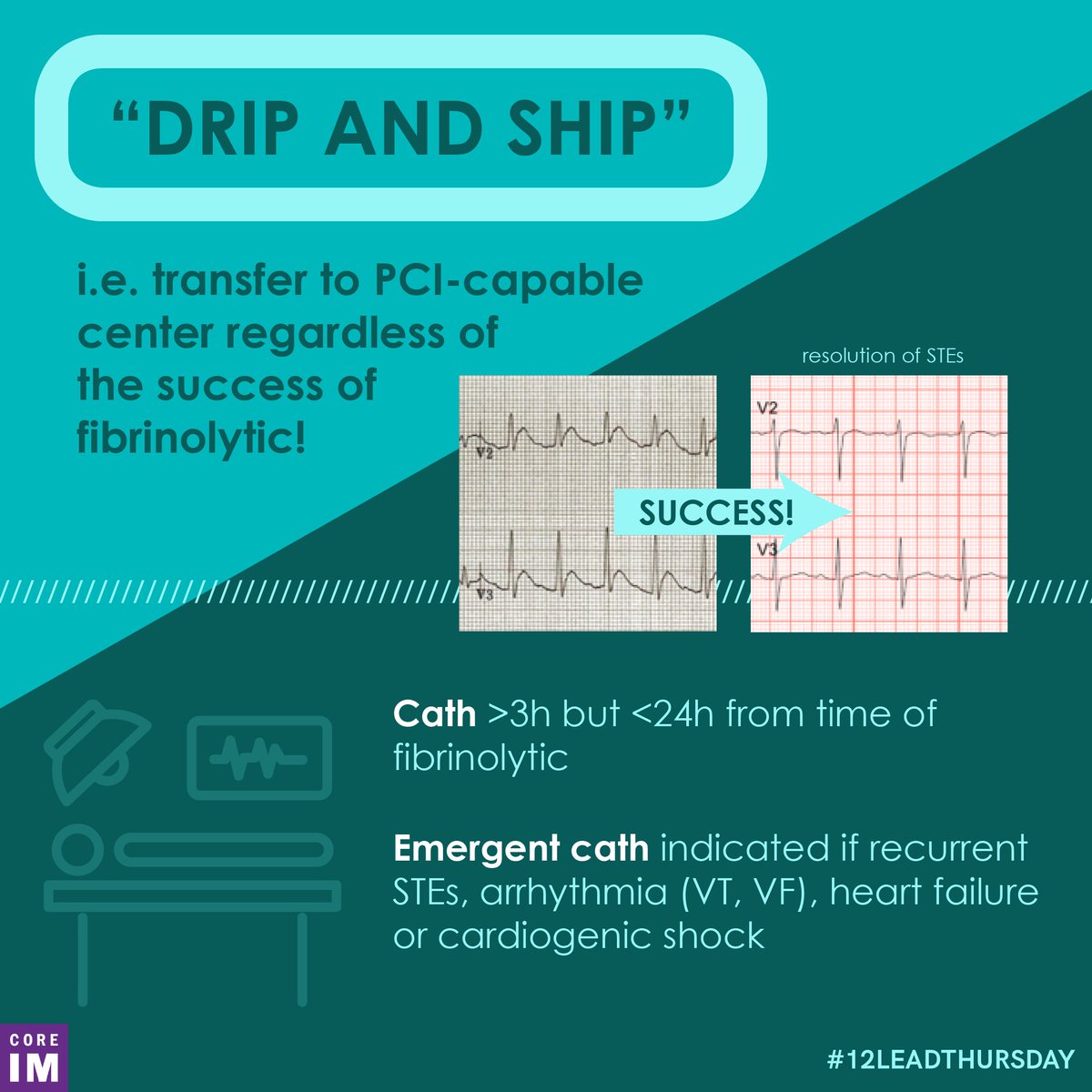
3/ Fibrinolytics are old, and they work; this meta-analysis suggests the totality of the evidence has favored their use since the 1970s (jamanetwork.com).
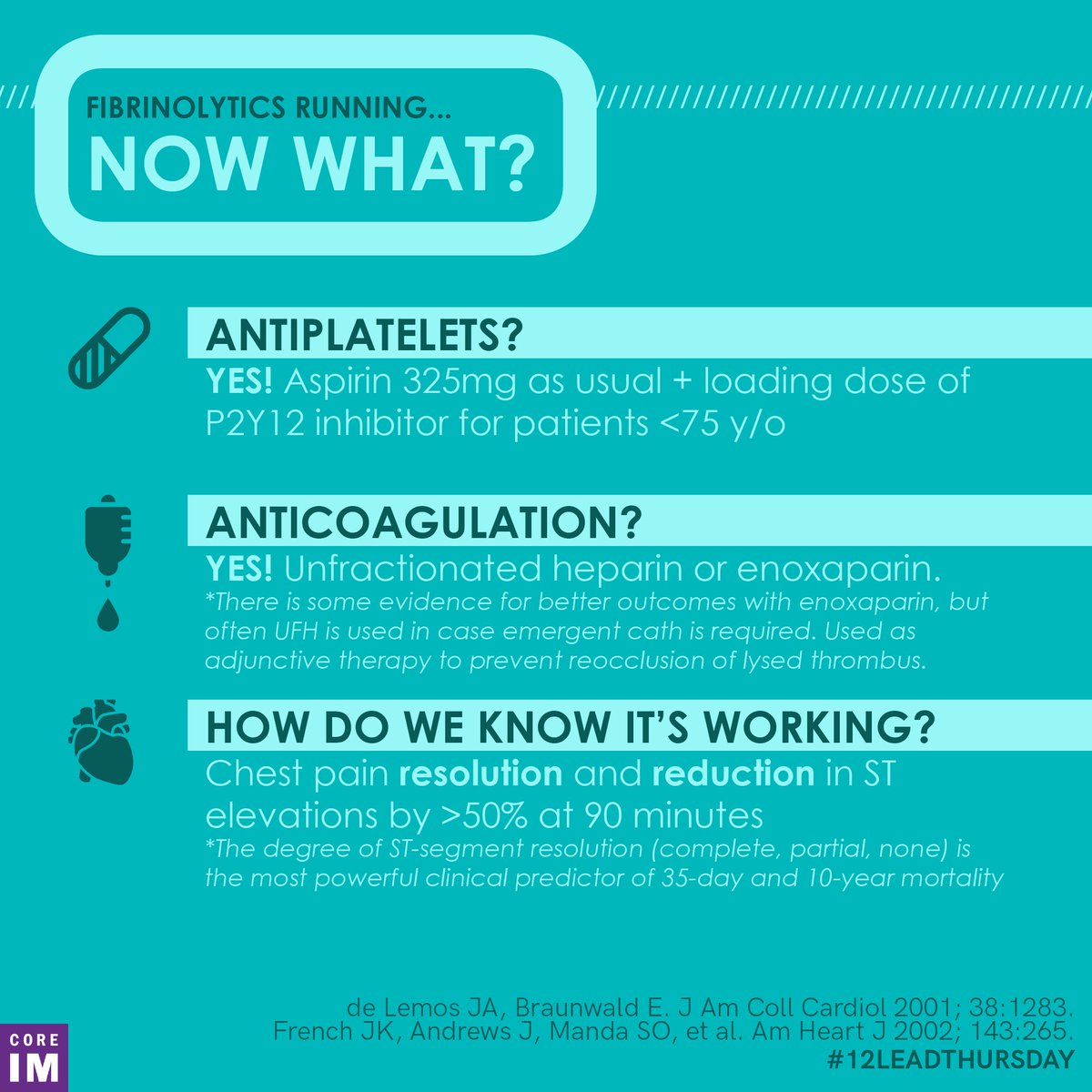
Once you get the fibrinolytics going, what else will you be giving your patient?
Once you get the fibrinolytics going, what else will you be giving your patient?
7/ Be sure to check out this week’s post and all our previous #12LeadThursday content on our website: coreimpodcast.com
8/ In summary: if PCI can’t be performed within 2 hours, patients with STEMIs get fibrinolytics in addition to DAPT and anticoagulation. They still need PCI, and should be transferred to the nearest PCI-capable facility ASAP.
Loading suggestions...