#MedTwitter - we're back with another tweetorial 🥳
Thanks @john_damianosMD for this week's edition on 🩸GI bleeds🩸
Thanks @john_damianosMD for this week's edition on 🩸GI bleeds🩸
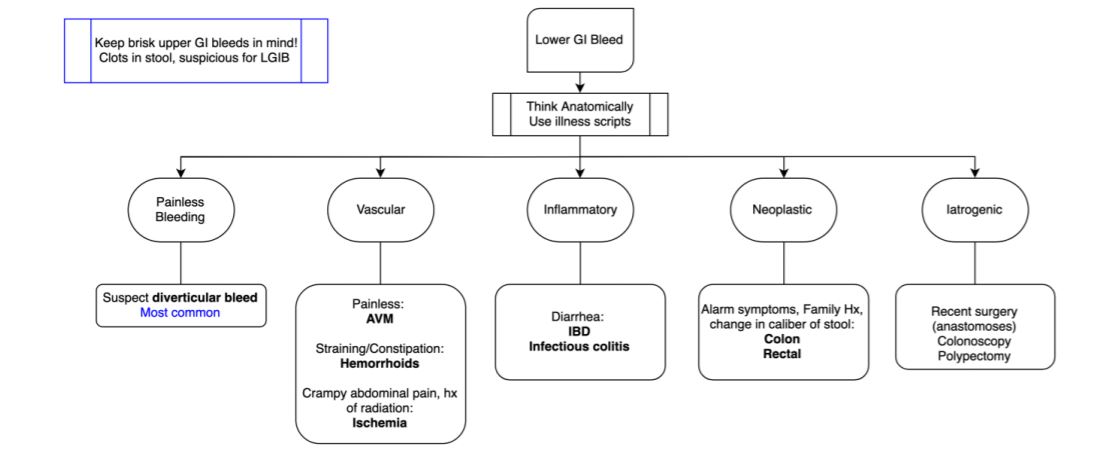
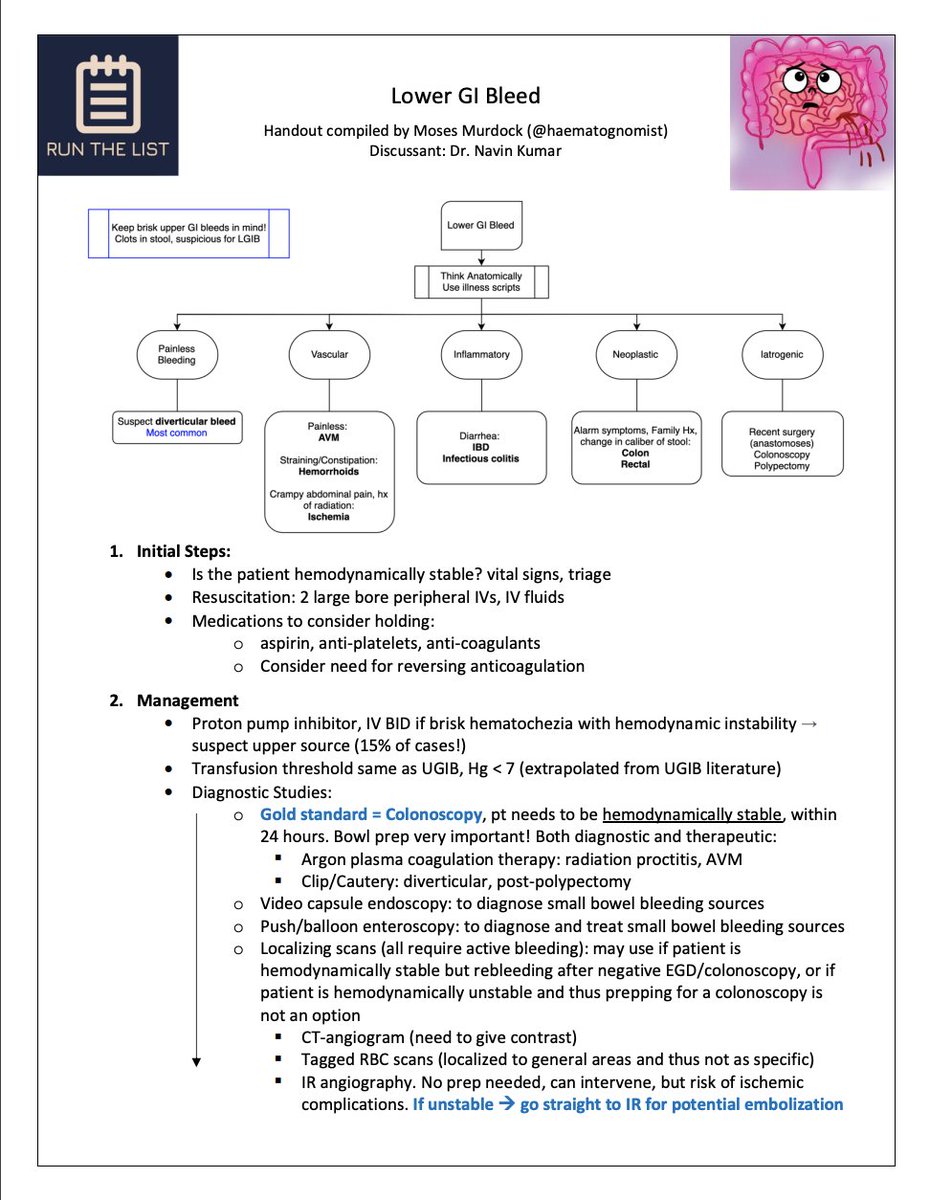
ICYMI, listen to our "Episode 4: Lower GI Bleed" pod which featured Dr. Navin Kumar @NavinKumarMD (gastroenterologist), and Dr. Walker Redd @WalkerReddMD (host).
To listen 🔊🍏: apple.co
Let's start with a guiding question below!🧐
To listen 🔊🍏: apple.co
Let's start with a guiding question below!🧐
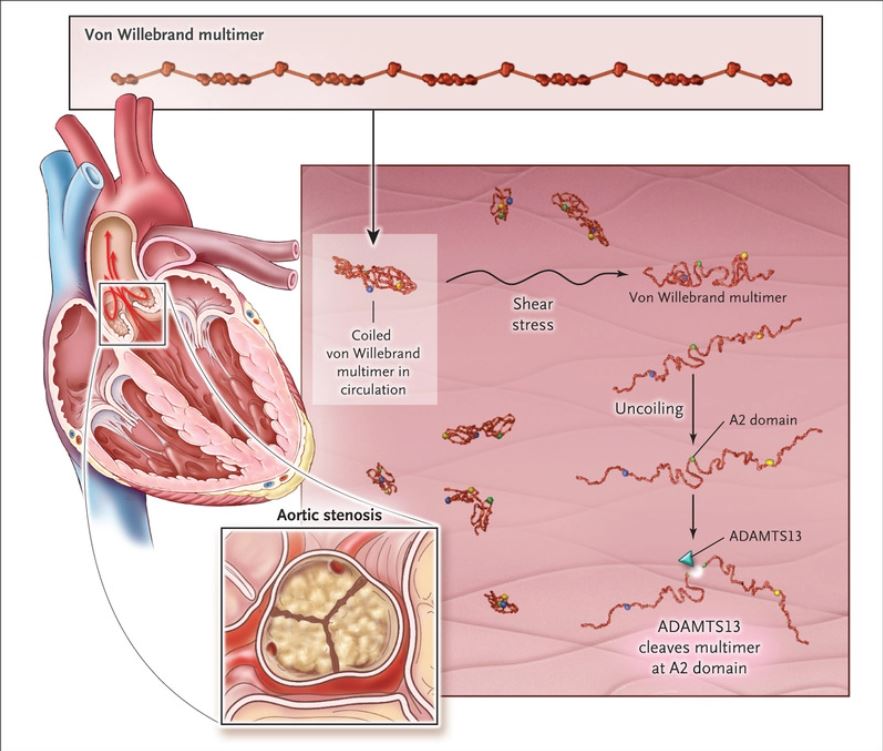
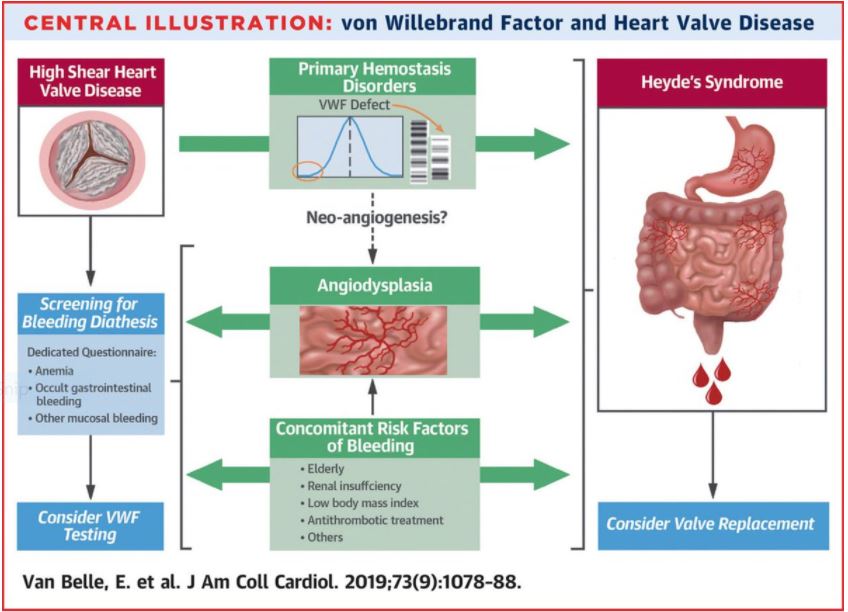
76 yo F w/ HTN, Afib (on apixaban), & moderate aortic stenosis was admitted with progressive weakness, fatigue, & melena, with Hgb = 6 g/dL.
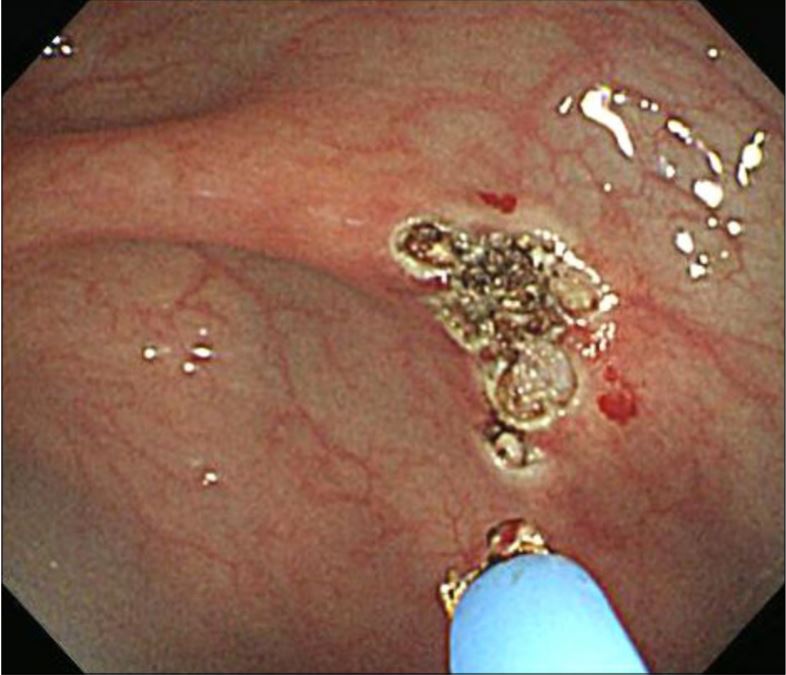
After💧resuscitation and🩸transfusion, she underwent colonoscopy which did❌locate source.
What is the next diagnostic step?
After💧resuscitation and🩸transfusion, she underwent colonoscopy which did❌locate source.
What is the next diagnostic step?
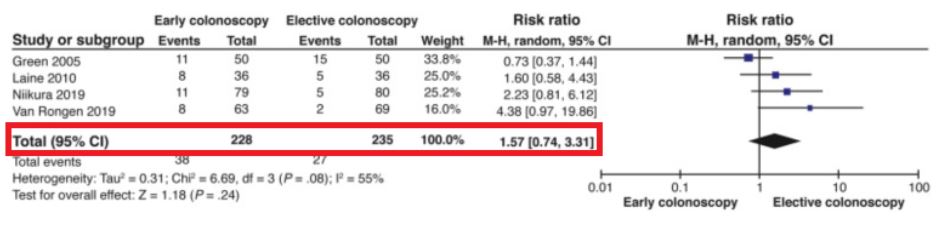
Should we rush to get them in before 24 hours? 🙅♂️
RCTs (pubmed.ncbi.nlm.nih.gov) found that earlier colonoscopy does❌ ⬇️re-bleeding or ⬇️mortality risk.
So instead, focus efforts toward adequate resuscitation & starting bowel prep!
Meta-analysis: pubmed.ncbi.nlm.nih.gov
RCTs (pubmed.ncbi.nlm.nih.gov) found that earlier colonoscopy does❌ ⬇️re-bleeding or ⬇️mortality risk.
So instead, focus efforts toward adequate resuscitation & starting bowel prep!
Meta-analysis: pubmed.ncbi.nlm.nih.gov
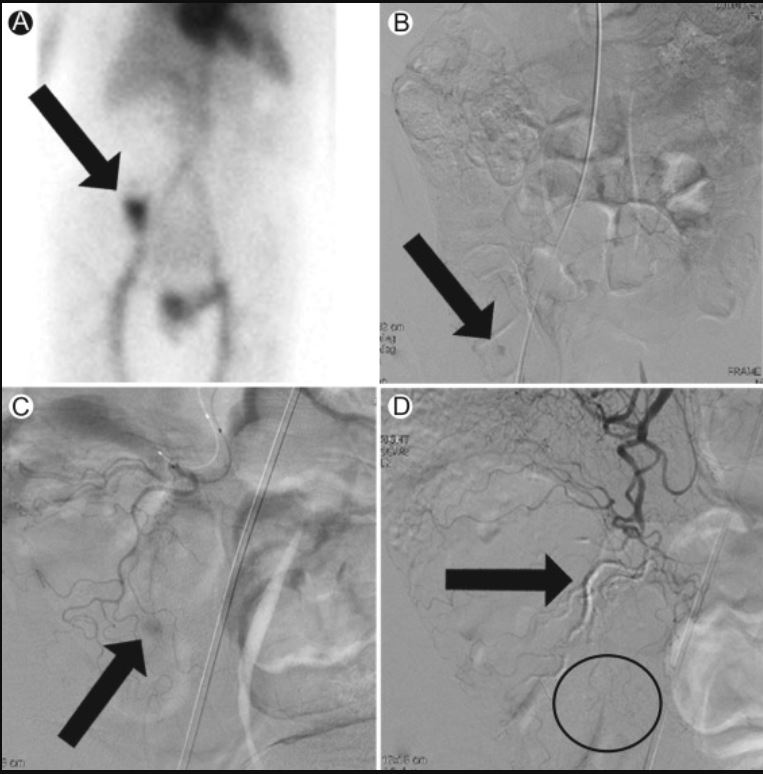
Okay, back to our 👵with a LGIB and negative colonoscopy. What's the next diagnostic step?
References:
[7]linkinghub.elsevier.com
[8]kjg.or.kr
[9]pubmed.ncbi.nlm.nih.gov, pubmed.ncbi.nlm.nih.gov
[10]gut.bmj.com, link.springer.com
[11]techvir.com
[14]nejm.org
[15]dl.uswr.ac.ir
[7]linkinghub.elsevier.com
[8]kjg.or.kr
[9]pubmed.ncbi.nlm.nih.gov, pubmed.ncbi.nlm.nih.gov
[10]gut.bmj.com, link.springer.com
[11]techvir.com
[14]nejm.org
[15]dl.uswr.ac.ir
Loading suggestions...