Cardiac risk assessment for non-cardiac surgery. Understanding pre-operative risk factors, cardiac testing, and peri-operative medical interventions. Good review prior to an upcoming cardiology consults rotation. @XavierPrida @USFIMres
#Cardiology #cardiotwitter #MedEd
#Cardiology #cardiotwitter #MedEd
Background:
- >50 million surgical procedures year in US, most performed electively
- Pooled analyses estimate 1.4%-3.9% complicated by major peri-operative cardiac event
- Identifying at risk patients can lead to better education about benefit-to-risk ratio of procedures
- >50 million surgical procedures year in US, most performed electively
- Pooled analyses estimate 1.4%-3.9% complicated by major peri-operative cardiac event
- Identifying at risk patients can lead to better education about benefit-to-risk ratio of procedures
CAD:
- Affects ~6.2% of US population, higher rates of peri-operative morbidity and mortality w/ unstable angina or MI
- Increased risk of MACE (major adverse cardiac event) closer to myocardial event
- ACC recommends 60-day interval from ACS to elective non-cardiac surgery
- Affects ~6.2% of US population, higher rates of peri-operative morbidity and mortality w/ unstable angina or MI
- Increased risk of MACE (major adverse cardiac event) closer to myocardial event
- ACC recommends 60-day interval from ACS to elective non-cardiac surgery
HF:
- Projected to affect 8 million people by 2030
- Acutely decompensated HF significant risk for peri-operative MACE
- Higher 30-day post-operative mortality rate w/ non-ischemic HF (9.3%), ischemic HF (9.2%) vs. AF (6.4%) or stable CAD (2.9%)
- Projected to affect 8 million people by 2030
- Acutely decompensated HF significant risk for peri-operative MACE
- Higher 30-day post-operative mortality rate w/ non-ischemic HF (9.3%), ischemic HF (9.2%) vs. AF (6.4%) or stable CAD (2.9%)
Valvular Heart Disease:
- Moderate/severe AS undergoing non-cardiac elective surgery had higher 30-day mortality vs. control (2.1% vs 1.0%) and higher post-op MI (3% vs. 1.1%), p= 0.001.
- Should monitor moderate-severe AS patients w/ invasive hemodynamics and post-op ICU
- Moderate/severe AS undergoing non-cardiac elective surgery had higher 30-day mortality vs. control (2.1% vs 1.0%) and higher post-op MI (3% vs. 1.1%), p= 0.001.
- Should monitor moderate-severe AS patients w/ invasive hemodynamics and post-op ICU
Arrhythmia:
- Prospective study from VA showed no increased risk of peri-operative MACE from asymptomatic ventricular arrhythmias or AF
- Increased risk from presence of increased number of PVC or non-sustained ventricular tachyarrhythmias
- Prospective study from VA showed no increased risk of peri-operative MACE from asymptomatic ventricular arrhythmias or AF
- Increased risk from presence of increased number of PVC or non-sustained ventricular tachyarrhythmias
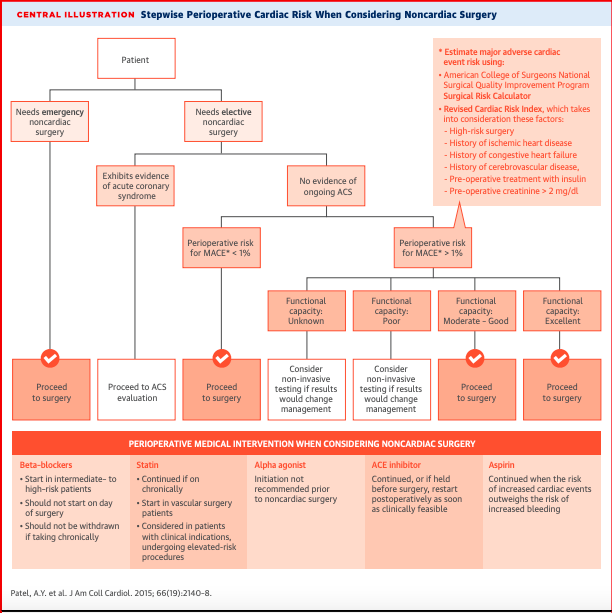
Algorithm:
- RCRI: 6 factors of risk: high-risk surgery, hx of ischemic heart disease, hx of CHF, hx of CVA, pre-operative tx w/ insulin, and pre-op Cr > 2
- NSQIP: 21-patient specific variables and calculates risk of 10 outcomes, including MACE and death riskcalculator.facs.org
- RCRI: 6 factors of risk: high-risk surgery, hx of ischemic heart disease, hx of CHF, hx of CVA, pre-operative tx w/ insulin, and pre-op Cr > 2
- NSQIP: 21-patient specific variables and calculates risk of 10 outcomes, including MACE and death riskcalculator.facs.org
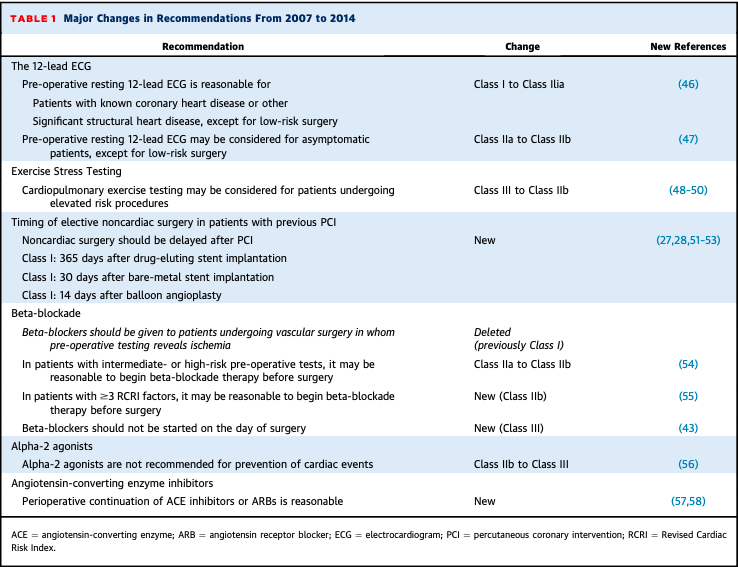
Medications:
- Beta-blockers (Class I): continue for patients on chronic therapy. Atenolol/bisoprolol shown efficacy.
- Statin (Class I): continue peri-operatively
- ACE:(Class IIa) continue peri-operatively and if held before surgery, to restart as clinically feasible post-op
- Beta-blockers (Class I): continue for patients on chronic therapy. Atenolol/bisoprolol shown efficacy.
- Statin (Class I): continue peri-operatively
- ACE:(Class IIa) continue peri-operatively and if held before surgery, to restart as clinically feasible post-op
Antiplatelet:
- Anti-platelet (Class I): continue DAPT for BMS unless risk of bleeding > prevention of stent thrombosis.
- Class IIb for patients w/o stents to continue daily ASA in peri-op period
- Class III to start ASA pre-op b/c risk of bleeding
- Anti-platelet (Class I): continue DAPT for BMS unless risk of bleeding > prevention of stent thrombosis.
- Class IIb for patients w/o stents to continue daily ASA in peri-op period
- Class III to start ASA pre-op b/c risk of bleeding
Conclusions:
- Pre-op assessment is a common cardiology consult
- Need close collaboration b/w patient, primary caregiver, cardiologists, surgeons, and anesthesiologists
- Lack of multiple, prospective, RCT. Future studies can help provide cost-effective care.
- Pre-op assessment is a common cardiology consult
- Need close collaboration b/w patient, primary caregiver, cardiologists, surgeons, and anesthesiologists
- Lack of multiple, prospective, RCT. Future studies can help provide cost-effective care.
Loading suggestions...