It's time folks! Welcome to this week's CbD! Tonight we have the fantastic @aswinchari as our moderator 🧠👏 look out for the code word that will be required for the feedback form to receive certificates of participation... and with that, let get started!
3. Great work guys! Some differentials include: extradural haematoma, subdural haematoma, subarachnoid haemorrhage, depressed skull fracture, traumatic brain injury, transient ischemia attack, intracranial abscess.
4. On arrival in ED, the patient is assessed by the nursing staff. The patient is alert and oriented to time, place, person. He’s chatting and able to move his whole body. He recalls the events of this afternoon quite well. What would you like to do?
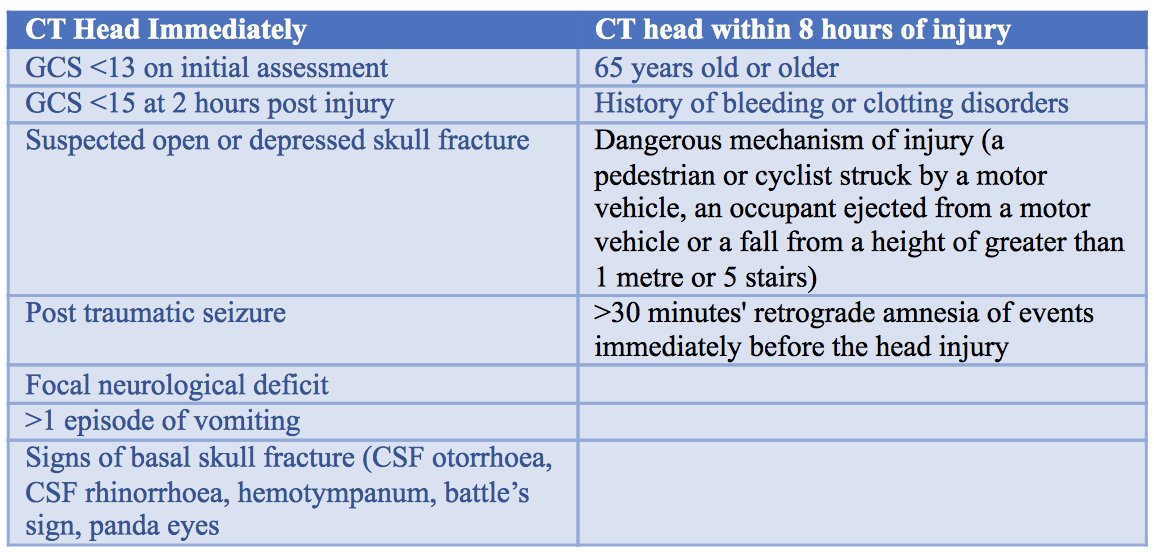
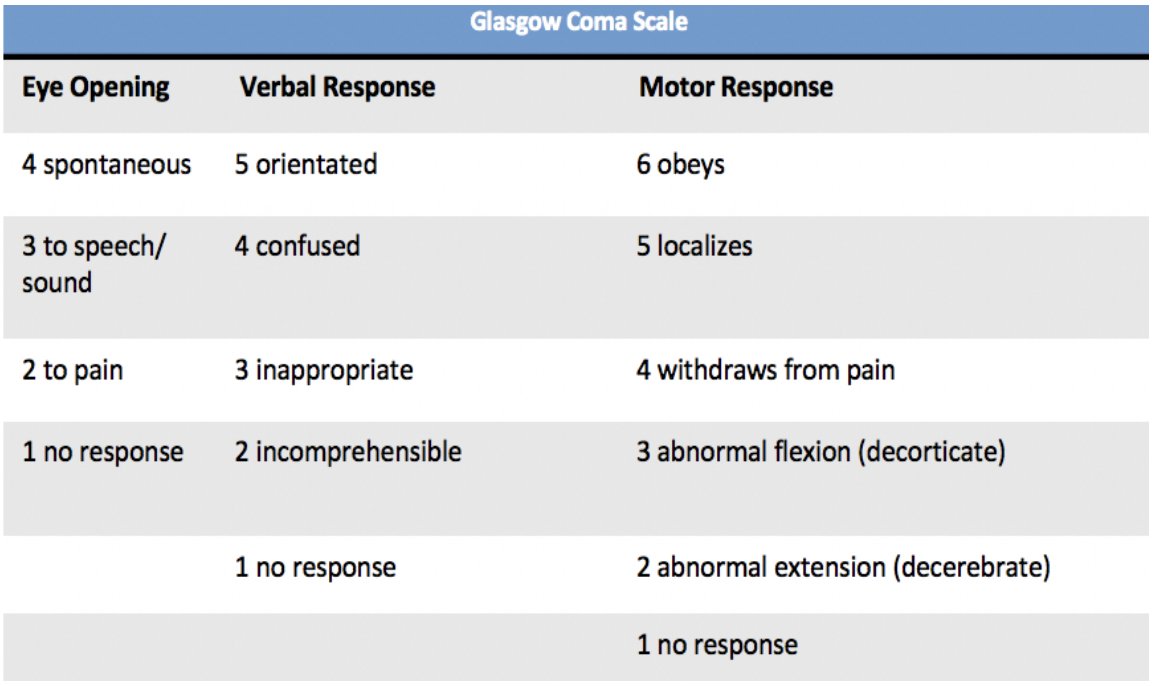
Well done guys! The patient has a GCS of 8 (E2 V2 M4). Check out our video here which goes through a detailed examination of the GCS! youtube.com
17. Anaesthetics yes! This is for intubation and mechanical ventilation. Patients with a low conscious level may lack protective airway reflexes and require a definitive airway. A GCS of 8 or less should be considered as such a risk and should be intubated.
21. Uncal herniation occurs when rising ICP causes herniation of the medial temporal lobe from the middle into the posterior fossa, across the tentorial opening. The uncus herniates over the tentorial notch compressing the third cranial nerve located just medial to the uncus.
25. Subfalcine herniation (brain extends under the falx cerebri), tonsillar (inferior descent of the cerebellar tonsils below the foramen magnum, central (diencephalon (thalamus and hypothalamus) and medial parts of temporal lobe are forced through a notch in tentorium cerebelli.
27. Raise head of bed to 30 degrees, Mannitol prescription: 0.25-1 g/kg over <20 mins. If the patient had a cervical collar you would consider loosening or removing it. Continue neuro-obs...
29. Well done guys! The accepting neurosurgeon informs you she is going to prepare CT and theatres so that the ambulance team can go straight from the ambulance bay to CT then up to theatres.
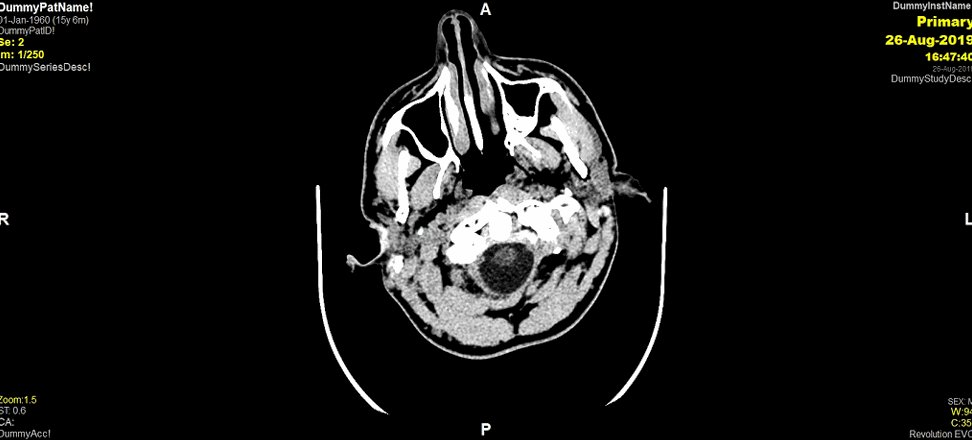
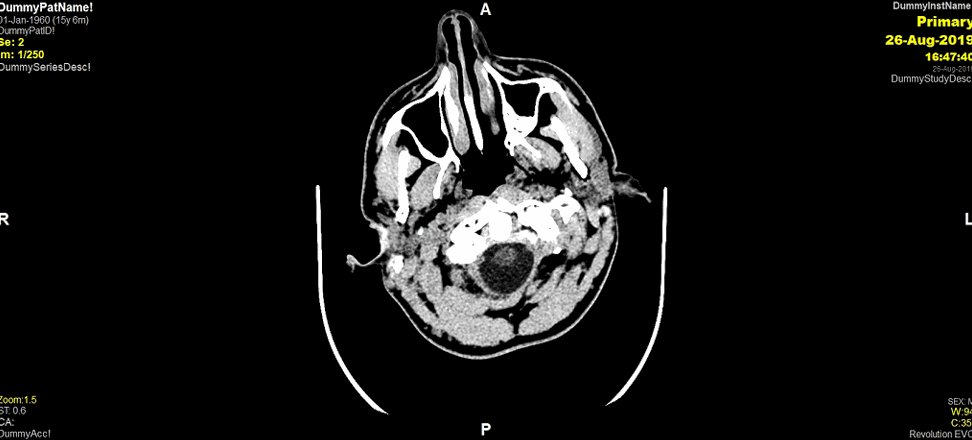
31. On neuro-imaging, extradural haematomas give a biconvex/elliptical/ lentiform shape. Does anyone know why this is? (gif inspired by @AbbieTutt!)
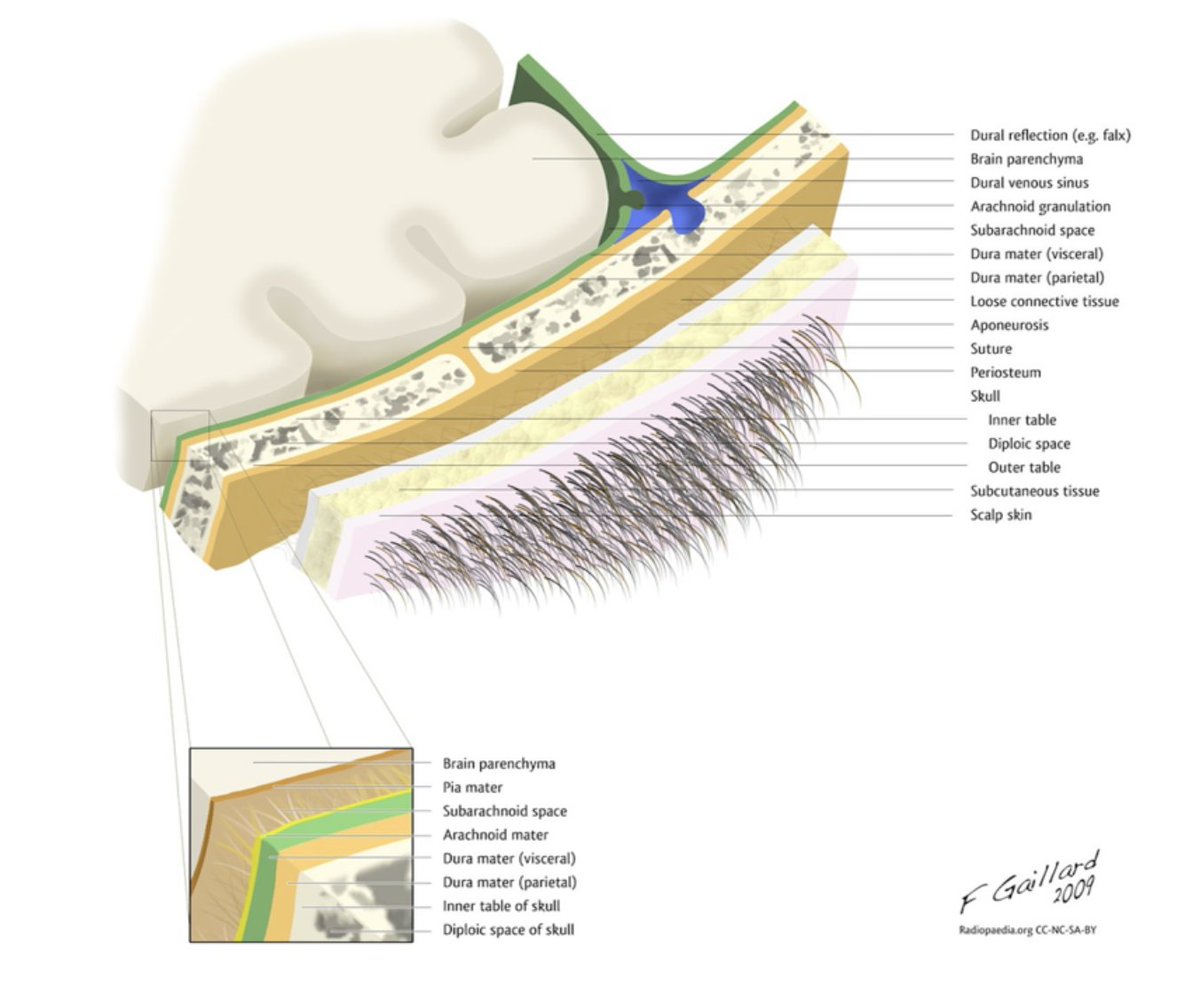
36. Within the cranial cavity, the dura consists of two connective tissue sheets: periosteal and meningeal layer. The periosteal layer lines the inner surface of the bones of the cranium; the meningeal layer lies deep to the periosteal layer in the cranial cavity...
40. Spot on! The middle meningeal artery. The middle meningeal artery is a branch of the maxillary artery. The maxillary artery is one of the terminal branches of the external carotid artery.
45. They present similar to our patient, patients typically present with an initial loss of consciousness following the trauma then a complete transient recovery known as the ‘lucid interval’. This is then followed by a rapid neurological deterioration.
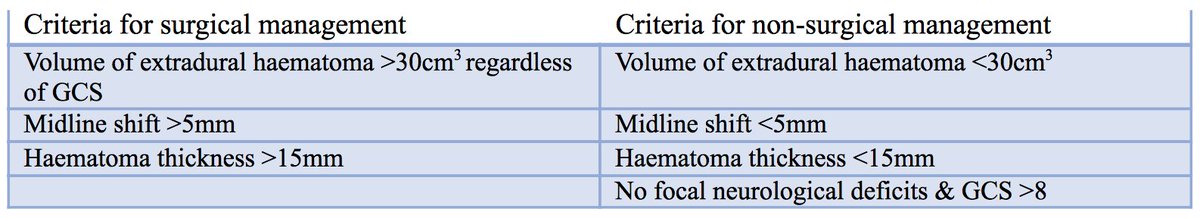
47. So how do we treat extradural haematomas?
51. It is decided to take the patient to theatre for a craniotomy and evacuation of the extradural haematoma. To find out how we perform this surgery, click this link to here! youtu.be
52. Who knows any complications of a craniotomy we look out for?
53. Complications include bleeding intra-operatively and post-operatively, seizure, hydrocephalus, meningitis, neurological deficit related to the area of surgery, coma, death.
54. The EDH is successfully evacuated and the patient is transferred to the neuro-observations ward where he is monitored. A post-operative CT shows complete evacuation of the haematoma and resolution of midline shift.
58. Contact the DVLA. A head injury often requires 6-12 months off driving and is dependent on a number of factors so it’s important to inform the DVLA and seek advice.
59. And that's a wrap! Amazing work guys, you clever bunch! And a BIG thank you to @aswinchari for his amazing words of wisdom 👏 Here is the feedback form to complete in order to receive your certificates of participation (don't forget the code word!) forms.gle
Loading suggestions...