When do you typically discharge your patients post-TAVR?
Check out the 🧵 below for a #tweetorial about same-day discharge following #TAVR!
@tavrkapadia @Edwards_TAVR @TAVRBot @cardioPCImom @SripalBangalore @SrihariNaiduMD @Pooh_Velagapudi @ehj_ed @DLBHATTMD @JPDeptaMD
Check out the 🧵 below for a #tweetorial about same-day discharge following #TAVR!
@tavrkapadia @Edwards_TAVR @TAVRBot @cardioPCImom @SripalBangalore @SrihariNaiduMD @Pooh_Velagapudi @ehj_ed @DLBHATTMD @JPDeptaMD
After this thread 🧵, you'll:
✅Recognize common complications🩺 after TAVR
✅Understand the feasibility of Same-Day Discharge (#SDD) and predictors of Next Day Discharge (NDD) after TAVR.
@CCIJournal #TAVR @WaqasTahir
✅Recognize common complications🩺 after TAVR
✅Understand the feasibility of Same-Day Discharge (#SDD) and predictors of Next Day Discharge (NDD) after TAVR.
@CCIJournal #TAVR @WaqasTahir
I feel comfortable🙂 identifying patients who can be discharged🚑 on the same-day after TAVR?
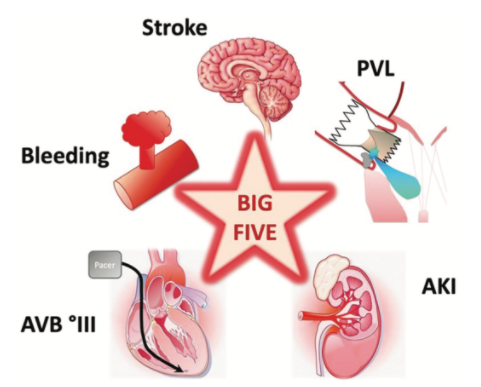
The common complication of #TAVR are:
1⃣Bleeding from the access site
2⃣New-onset LBBB
3⃣CHB
4⃣Stroke
5⃣Coronary occlusion
6⃣Contrast associated nephropathy
Conduction Abnormalities are very common. So how you may quickly predict if your patient may require a PPM?
1⃣Bleeding from the access site
2⃣New-onset LBBB
3⃣CHB
4⃣Stroke
5⃣Coronary occlusion
6⃣Contrast associated nephropathy
Conduction Abnormalities are very common. So how you may quickly predict if your patient may require a PPM?
A @ClevelandClinic study showed post-TAVR rapid atrial pacing (RAP) has 99% NPV for pacemaker implantation:
So, RAP may help risk-stratify patients in the management of post-TAVR conduction disturbances.
So, RAP may help risk-stratify patients in the management of post-TAVR conduction disturbances.
What else should we consider❓
A @TallRoundsTM @CleveClinicCath study compared predictors of NDD (Next Day DC) vs. Non-NDD
Predictors of NDD were male♂️, relatively younger age (less than 90), absence of atrial fibrillation, and lower serum Cr)
A @TallRoundsTM @CleveClinicCath study compared predictors of NDD (Next Day DC) vs. Non-NDD
Predictors of NDD were male♂️, relatively younger age (less than 90), absence of atrial fibrillation, and lower serum Cr)
We report case series of 6 patients #SDD post-TAVR. Pts underwent RAP to risk stratify.
3 hrs➡️➡️ post-TAVR all patients were ambulated🚶♀️🚶♂️ multiple times to ensure an intact vascular access site.
Post-TAVR, vascular complications are one of the major barriers to discharge.
3 hrs➡️➡️ post-TAVR all patients were ambulated🚶♀️🚶♂️ multiple times to ensure an intact vascular access site.
Post-TAVR, vascular complications are one of the major barriers to discharge.
When selecting pts for possible SDD, our pts had similar characteristics as the @CleveClinicCath Study of NDD and were ambulatory w/ good social support.🚶♀️🚶
Here is our protocol for considering #SDD post-TAVR.
@JPDeptaMD @DLBHATTMD @WaqasTahir @InstituteSands
Here is our protocol for considering #SDD post-TAVR.
@JPDeptaMD @DLBHATTMD @WaqasTahir @InstituteSands
In another study from @emoryheart @EmoryCCRI, they developed a protocol for SDD after #TAVR @CCI
Patients not meeting the following criteria were considered for #SDD.
Patients not meeting the following criteria were considered for #SDD.
I learned something in this #Tweetorial that may change my clinical practice.
Many thanks🙏 to @ThomasMDas @Cardionerds @karanpdesai Academy for their feedback and support!
Thanks to @AmitGoyalMD and @Dr_DanMD for democratizing CV🫀 education and bringing all @cardionerds together.
Thanks to @AmitGoyalMD and @Dr_DanMD for democratizing CV🫀 education and bringing all @cardionerds together.
I feel comfortable identifying patients who can be discharged on the same day after TAVR?
Loading suggestions...