🚨 Here are the ⭐️ new ⭐️ @AmCollegeGastro guidelines on the Prevention, Diagnosis, and Treatment of Clostridioides difficile Infections! I'll summarize in 🧵 below!
🦠 ▶️ 💩 💩 💩 ▶️ 😷
#GITwitter #GI #gut #Cdiff #microbiome
journals.lww.com
🦠 ▶️ 💩 💩 💩 ▶️ 😷
#GITwitter #GI #gut #Cdiff #microbiome
journals.lww.com
PREVENTION
😷 isolation precautions
🧤Gloves and gowns
🧼 Hand hygiene
💊 antibiotic stewardship
😷 isolation precautions
🧤Gloves and gowns
🧼 Hand hygiene
💊 antibiotic stewardship
🦠 #Probiotics are ❌ recommended for primary or secondary prevention of CDI.
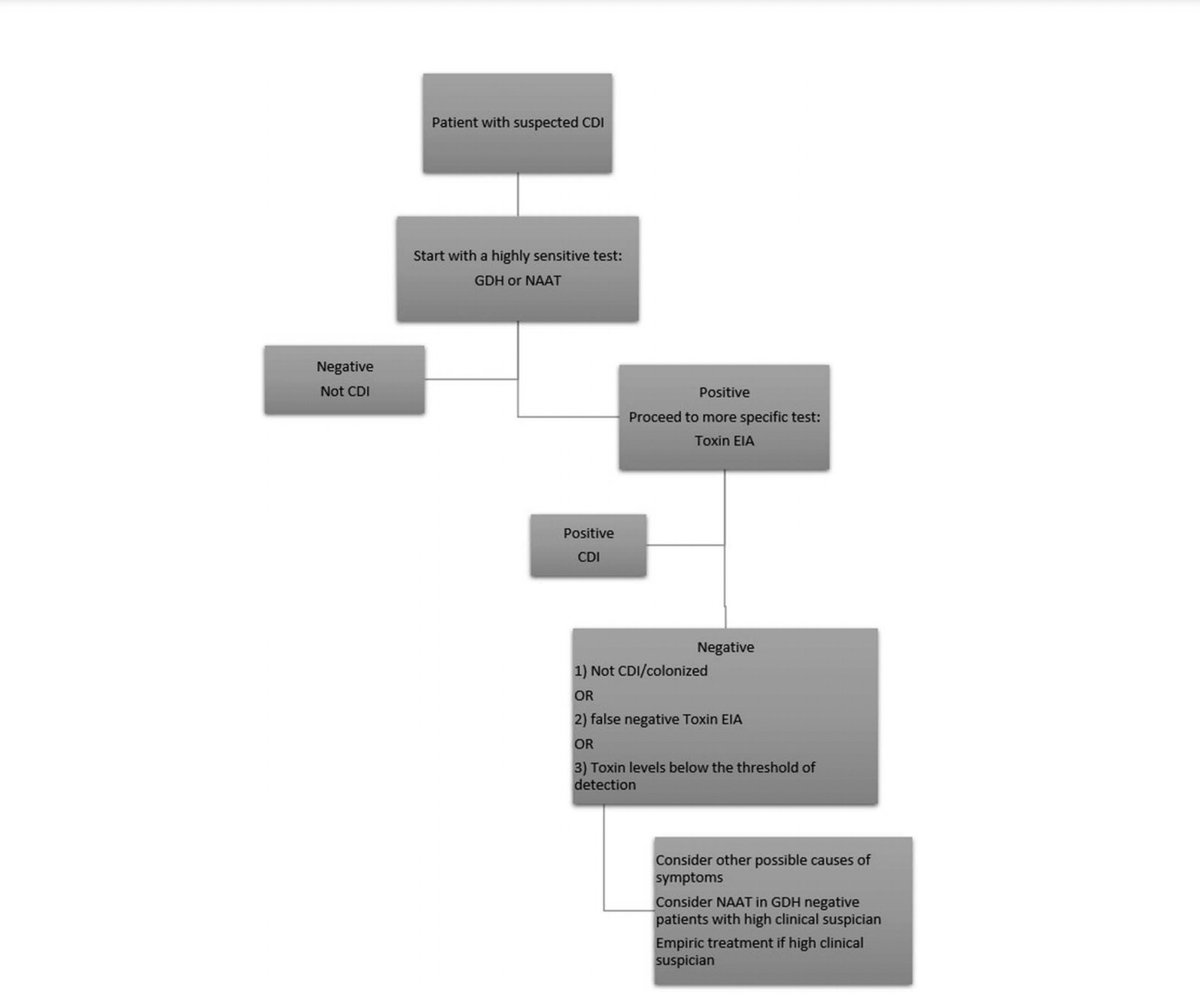
1⃣Sensitive NAAT or GDH
2⃣Specific toxin EIA
1➕ 2➕ = CDI
1 ➖ 2 ➖ = ❌ CDI
1 ➕ 2➖ = colonization OR low levels of toxin OR false negative (if high pre-test probability, re-test)
🧠There are alternative causes of diarrhea in C. diff colonized patients (PI-#IBS very common)
2⃣Specific toxin EIA
1➕ 2➕ = CDI
1 ➖ 2 ➖ = ❌ CDI
1 ➕ 2➖ = colonization OR low levels of toxin OR false negative (if high pre-test probability, re-test)
🧠There are alternative causes of diarrhea in C. diff colonized patients (PI-#IBS very common)
SEVERE CDI
🧪 WBC ≥ 15,000
OR
🧪serum creatinine > 1.5
FULMINANT CDI = severe CDI ➕
🩸 hypotension or shock
OR
💩 ileus or megacolon
Other poor prognostics: ⬇️albumin, ⬆️FCP, peripheral eosinophilia, 🥵 > 38.5, NAP/027/BI strain 🦠, pseudomembranes
🧪 WBC ≥ 15,000
OR
🧪serum creatinine > 1.5
FULMINANT CDI = severe CDI ➕
🩸 hypotension or shock
OR
💩 ileus or megacolon
Other poor prognostics: ⬇️albumin, ⬆️FCP, peripheral eosinophilia, 🥵 > 38.5, NAP/027/BI strain 🦠, pseudomembranes
Treatment of non-severe CDI
💊oral vancomycin 125 mg 4x daily for 10
days (for initial infection)
💊oral fidaxomicin 200 mg 2x daily for 10
days (for initial infection)
💊oral metronidazole 500 mg 3x daily for 10 days may be considered in low-risk patients (for initial infection)
💊oral vancomycin 125 mg 4x daily for 10
days (for initial infection)
💊oral fidaxomicin 200 mg 2x daily for 10
days (for initial infection)
💊oral metronidazole 500 mg 3x daily for 10 days may be considered in low-risk patients (for initial infection)
⚠️Fidaxomicin is equivalent to vancomycin for cure and superior to prevent recurrence (and 💰 is roughly equivalent if we take into account the effect on recurrence...)
❌Rifaximin, tigecycline, cadazolid, surotomycin, teicoplanin, nitazoxanide
❌Rifaximin, tigecycline, cadazolid, surotomycin, teicoplanin, nitazoxanide
❌anti-motility agents before treatment, but ok for prn once 💊 has started
❌cholestyramine (can interact with antibiotics)
✅psyllium or dietary fiber
❌cholestyramine (can interact with antibiotics)
✅psyllium or dietary fiber
Treatment of severe CDI
💊 oral vancomycin 125 mg 4x a day for 10 days
💊 fidaxomicin 200 mg 2x for 10 days
⛔️ metronidazole❗️
💊 oral vancomycin 125 mg 4x a day for 10 days
💊 fidaxomicin 200 mg 2x for 10 days
⛔️ metronidazole❗️
Treatment of fulminant CDI
💊adequate volume resuscitation & treatment w 500 mg oral vancomycin every 6 hours daily for the first 48–72 hrs. Combo therapy w IV metronidazole 500 mg every 8 hrs can be considered
💉if ileus, vancomycin enema 500
mg every 6 hours) may be beneficial
💊adequate volume resuscitation & treatment w 500 mg oral vancomycin every 6 hours daily for the first 48–72 hrs. Combo therapy w IV metronidazole 500 mg every 8 hrs can be considered
💉if ileus, vancomycin enema 500
mg every 6 hours) may be beneficial
#Surgery
✂️If patient needs surgery: total colectomy with end ileostomy & a stapled rectal stump OR diverting loop ileostomy with colonic lavage & intraluminal vancomycin (depending on clinical circumstances, patient’s estimated tolerance to surgery, & surgeon’s best judgment)
✂️If patient needs surgery: total colectomy with end ileostomy & a stapled rectal stump OR diverting loop ileostomy with colonic lavage & intraluminal vancomycin (depending on clinical circumstances, patient’s estimated tolerance to surgery, & surgeon’s best judgment)
#FMT
💩FMT should be considered in severe &
fulminant CDI refractory to antibiotic therapy, especially in patients who are poor surgical candidates
⚠️Most will require sequential FMT in conjunction with antibiotics (V or F) (repeat every 3-5d until resolution of pseudomembrane)
💩FMT should be considered in severe &
fulminant CDI refractory to antibiotic therapy, especially in patients who are poor surgical candidates
⚠️Most will require sequential FMT in conjunction with antibiotics (V or F) (repeat every 3-5d until resolution of pseudomembrane)
💩 Consider #FMT in severe or fulminant CDI after 48-72 hrs of maximum medical therapy
✂️ surgery is still a standard treatment for these patients though, especially if there is toxic megacolon, ischemia, or
perforation
✂️ surgery is still a standard treatment for these patients though, especially if there is toxic megacolon, ischemia, or
perforation
Treatment of recurrent CDI
💊taper/pulsed-dose vancomycin for 1st recurrence after initial course of fidaxomicin, vancomycin, or metronidazole
💊fidaxomicin for 1st recurrence after an initial course of vancomycin or metronidazole
⛔️metronidazole should ❌ be used in rCDI
💊taper/pulsed-dose vancomycin for 1st recurrence after initial course of fidaxomicin, vancomycin, or metronidazole
💊fidaxomicin for 1st recurrence after an initial course of vancomycin or metronidazole
⛔️metronidazole should ❌ be used in rCDI
#FMT for rCDI
💩FMT for 2nd or further recurrences to prevent future recurrences
💩deliver via colonoscopy or capsules ("crapsules" 😆); enema if those are unavailable
💩repeat FMT for patients experiencing a recurrence of
CDI within 8 weeks of an initial FMT
💩FMT for 2nd or further recurrences to prevent future recurrences
💩deliver via colonoscopy or capsules ("crapsules" 😆); enema if those are unavailable
💩repeat FMT for patients experiencing a recurrence of
CDI within 8 weeks of an initial FMT
PREVENTION
💊 For patients with rCDI who are not candidates for #FMT, who relapsed after FMT, or who require ongoing or frequent courses of antibiotics, long-term suppressive oral vancomycin may be used to prevent further recurrences
💊 For patients with rCDI who are not candidates for #FMT, who relapsed after FMT, or who require ongoing or frequent courses of antibiotics, long-term suppressive oral vancomycin may be used to prevent further recurrences
PREVENTION
💊 Oral vancomycin prophylaxis (OVP) may be considered during subsequent systemic antibiotic use in patients with a history of CDI who are at high risk of recurrence to prevent further recurrence
💊 Oral vancomycin prophylaxis (OVP) may be considered during subsequent systemic antibiotic use in patients with a history of CDI who are at high risk of recurrence to prevent further recurrence
PREVENTION
💉consider bezlotoxumab for prevention of
CDI recurrence in patients who are at high risk of recurrence
BEZ = monoclonal antibody that binds to toxin B
🔸given during abx treatment
⚠️avoid in those with 🫀 failure
💉consider bezlotoxumab for prevention of
CDI recurrence in patients who are at high risk of recurrence
BEZ = monoclonal antibody that binds to toxin B
🔸given during abx treatment
⚠️avoid in those with 🫀 failure
❓PPI
💊PPIs ⬆️ risk of CDI, but the risk is small
💊⛔️stop PPI in CDI (as long as there is appropriate indication)
💊PPIs ⬆️ risk of CDI, but the risk is small
💊⛔️stop PPI in CDI (as long as there is appropriate indication)
CDI in #IBD
🧪test for CDI in IBD patients presenting with flare with diarrhea
💊vancomycin 125 mg p.o. 4 times a day for a minimum
of 14 days
🧪test for CDI in IBD patients presenting with flare with diarrhea
💊vancomycin 125 mg p.o. 4 times a day for a minimum
of 14 days
#IBD and CDI
💩IBD⬆️CDI risk 4.8x
💩more likely to be younger, have community-onset CDI, and rCDI
💩RFs: steroids, infliximab/adalimumab, previous hospitalizations, more frequent ambulatory care visits, shorter duration of IBD, ⬆️comorbidities
💩IBD⬆️CDI risk 4.8x
💩more likely to be younger, have community-onset CDI, and rCDI
💩RFs: steroids, infliximab/adalimumab, previous hospitalizations, more frequent ambulatory care visits, shorter duration of IBD, ⬆️comorbidities
💩4x⬆️mortality risk if #IBD patient is hospitalized (cf IBD or CDI hospitalization alone)
💩Higher mortality in UC > CD
💩CDI ⬆️ risk of colectomy ✂️ in the long term
💩Higher mortality in UC > CD
💩CDI ⬆️ risk of colectomy ✂️ in the long term
SPECIAL POPULATIONS
🤰treat pregnant individuals with vancomycin
🤰treat breatfeeding individuals with vancomycin (does not enter breastmilk)
😷Immunocompromised: vancomycin or fidaxomicin
🤰treat pregnant individuals with vancomycin
🤰treat breatfeeding individuals with vancomycin (does not enter breastmilk)
😷Immunocompromised: vancomycin or fidaxomicin
Loading suggestions...