It’s time for another #EndNeurophobia #tweetorial!
PUPILS AND ANISOCORIA
#MedStudentTwitter #neurotwitter #MedEd
@DxRxEdu @rabihmgeha @CPSolvers @Tracey1milligan @NMatch2022
🧠❤️
PUPILS AND ANISOCORIA
#MedStudentTwitter #neurotwitter #MedEd
@DxRxEdu @rabihmgeha @CPSolvers @Tracey1milligan @NMatch2022
🧠❤️
The pupils can constrict (miosis) and dilate (mydriasis)
Mydriasis = bigger word = bigger pupil.
Constriction is a PARASYMPATHETIC function (tiny relaxed happy pupils)
Dilation is a SYMPATHETIC function (eyes wide with fear)
Mydriasis = bigger word = bigger pupil.
Constriction is a PARASYMPATHETIC function (tiny relaxed happy pupils)
Dilation is a SYMPATHETIC function (eyes wide with fear)
Pupils constrict in response to LIGHT and NEAR
Pupils dilate in response to DARKNESS and ADRENERGIC TONE
Drugs can also affect the pupils as can prior trauma/surgery
Pupils dilate in response to DARKNESS and ADRENERGIC TONE
Drugs can also affect the pupils as can prior trauma/surgery
If BOTH pupils are small consider:
Older age (normal finding)
Pontine lesion
Opiates
Syphilis
If BOTH pupils are large consider:
Sympathomimetic medications (amphetamines, cocaine)
Bilateral CN 3 (would be rare in isolation)
Older age (normal finding)
Pontine lesion
Opiates
Syphilis
If BOTH pupils are large consider:
Sympathomimetic medications (amphetamines, cocaine)
Bilateral CN 3 (would be rare in isolation)
It the pupils are unequal = ANISOCORIA
The first question is: which pupil is the abnormal one, the small one or the large one?
First clue: the EYELIDS
Ptosis + small pupil = Horner (usually ptosis is mild, more below)
Ptosis + large pupil = CN 3 palsy (usual ptosis complete)
The first question is: which pupil is the abnormal one, the small one or the large one?
First clue: the EYELIDS
Ptosis + small pupil = Horner (usually ptosis is mild, more below)
Ptosis + large pupil = CN 3 palsy (usual ptosis complete)
If Horner, where along pathway?
1st order=hypothalamus/brainstem/spinal cord (look for neighborhood signs eg. lat med syndrome)
2nd order=sympathetic chain over lung apex to carotid bifurcation (risk for lung CA or TB?)
3rd order=along Int carotid to eye (carotid dissection)
1st order=hypothalamus/brainstem/spinal cord (look for neighborhood signs eg. lat med syndrome)
2nd order=sympathetic chain over lung apex to carotid bifurcation (risk for lung CA or TB?)
3rd order=along Int carotid to eye (carotid dissection)
Most sweating fibers for the face travel with external carotid, so lesion along the internal carotid (eg. dissection)=ptosis+miosis, NO anhidrosis (except small region of medial nose/forehead)
Anihidrosis can be hard to detect – there is always some sweat on forehead, can run tuning fork across and see if ‘smoother’ on one side. Or look for asymmetric flushing (Harlequin syndrome):
n.neurology.org
n.neurology.org
Can also localize Horner with drops. Confusing and lwho has cocaine eyedrops (!?), but if interested or fan of #Ophthotwitter @DGlaucomflecken see figure
Complete lesion of CN 3=ptosis (complete), eye down/out, pupil dilated. But pupilloconstrictor fibers run on medial outer surface of CN3 so compressive lesion (eg. uncal herniation, pcomm aneurysm) can cause pupil dilation w/o other CN 3 signs
Conversely diabetic microinfarct of 3 can cause pupil sparing 3rd nerve palsy (eye down/out + ptosis, but pupil normal/reactive)
Common consult= "NEURO STAT: blown pupil!
?herniation"
Actually due to…nebulizer treatment blowing into one eye or scopolamine patch->touch eye
Toxic/metabolic/drug always on Ddx for any neuro symptom!
?herniation"
Actually due to…nebulizer treatment blowing into one eye or scopolamine patch->touch eye
Toxic/metabolic/drug always on Ddx for any neuro symptom!
Anisocoria can also be seen:
During migraine
During seizure or postictal state
2/2 local iris surgery or trauma
Physiologic (will be same in light/dark and both pupils react)
During migraine
During seizure or postictal state
2/2 local iris surgery or trauma
Physiologic (will be same in light/dark and both pupils react)
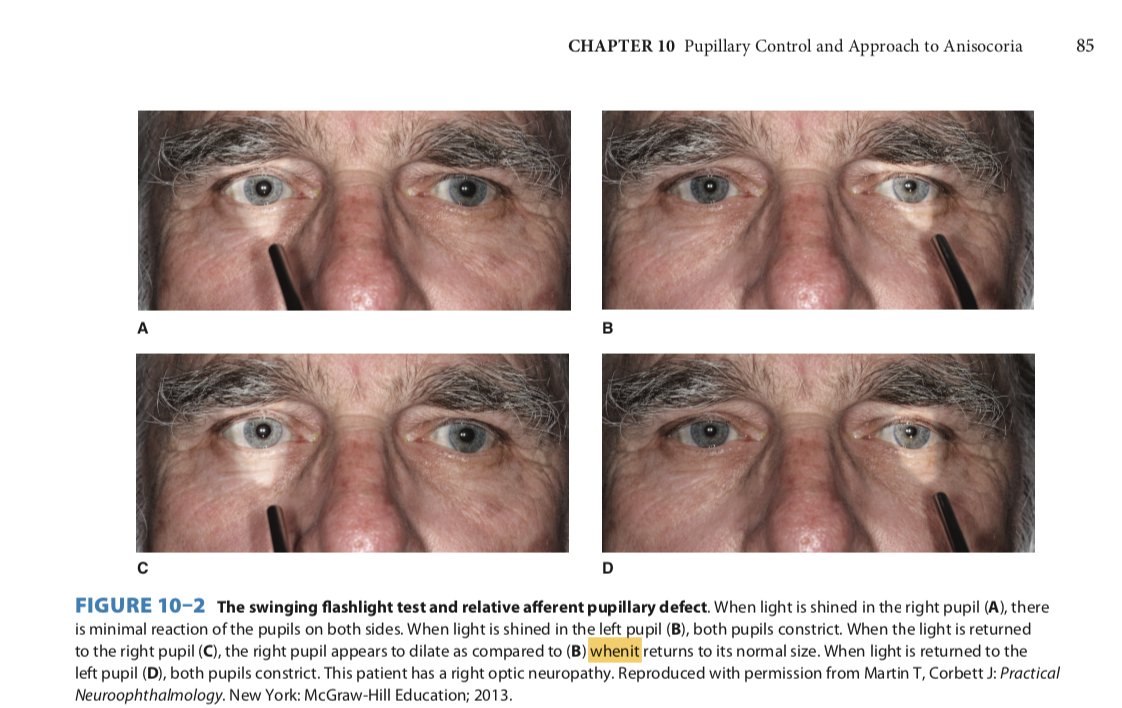
RAPD (cont)
Shine light in CN2 lesion side: neither pupil constricts (light not detected)
So swinging flashlight test = looks like Cn2 lesion side ‘dilates’ to light (actually just going from constricted (from contralateral light stimulus/consensual response) back to normal
Shine light in CN2 lesion side: neither pupil constricts (light not detected)
So swinging flashlight test = looks like Cn2 lesion side ‘dilates’ to light (actually just going from constricted (from contralateral light stimulus/consensual response) back to normal
RAPD (cont)
Can rarely be caused by unilateral optic tract or rarely unilateral midbrain lesion, or severe unilateral or asymmetric retinal disease but most commonly optic neuropathy
Can rarely be caused by unilateral optic tract or rarely unilateral midbrain lesion, or severe unilateral or asymmetric retinal disease but most commonly optic neuropathy
Light near dissociation:
Many more fibers devoted to NEAR response than light and chronic CN 3 injury=preferential reinnervation of near fibers than light
Classic is syphilis (ArgYll-RobertsoN: Ay-Rn = accommodates yes, reacts no)
Many more fibers devoted to NEAR response than light and chronic CN 3 injury=preferential reinnervation of near fibers than light
Classic is syphilis (ArgYll-RobertsoN: Ay-Rn = accommodates yes, reacts no)
Light near dissociation (cont)
Also
Part of Parinaud (light-near dissoc/lid retraction/upgaze palsy/convergence retraction nystagmus 2/2 dorsal midbrain lesion e.g., pineloma)
Adie pupil (A-Di = A Di-lated pupil): idiopathic, constricts to pilocarpine
Check out @neudrawlogy
Also
Part of Parinaud (light-near dissoc/lid retraction/upgaze palsy/convergence retraction nystagmus 2/2 dorsal midbrain lesion e.g., pineloma)
Adie pupil (A-Di = A Di-lated pupil): idiopathic, constricts to pilocarpine
Check out @neudrawlogy
In sum:
Constriction = paraymp (CN 3)
Dilation = symp (Horner pathway)
Anisocoria: look for ptosis (ptosis + small = Horner; ptosis + large = CN 3)
Check light v dark (worse in light = dilated pupil abnormal (CN3); worse in dark = small pupil abnormal (Horner))
Constriction = paraymp (CN 3)
Dilation = symp (Horner pathway)
Anisocoria: look for ptosis (ptosis + small = Horner; ptosis + large = CN 3)
Check light v dark (worse in light = dilated pupil abnormal (CN3); worse in dark = small pupil abnormal (Horner))
What did I miss @prasad_sashank? 🧠👀
All figures from amazon.com
#EndNeurophobia🧠❤️
@MariaMjaleman @gabifpucci @valeroldan23 @DrSakhii
All figures from amazon.com
#EndNeurophobia🧠❤️
@MariaMjaleman @gabifpucci @valeroldan23 @DrSakhii
like these? Check out the #EndNeurophobia series here:
and let me know what topics to cover next! 🧠❤️
and let me know what topics to cover next! 🧠❤️
Loading suggestions...