Health
Pharmaceuticals
Neurology
Neurotwitter
NeuroICU
Hydralazine
Cerebral Hemodynamics
ICP
Anti-hypertensive
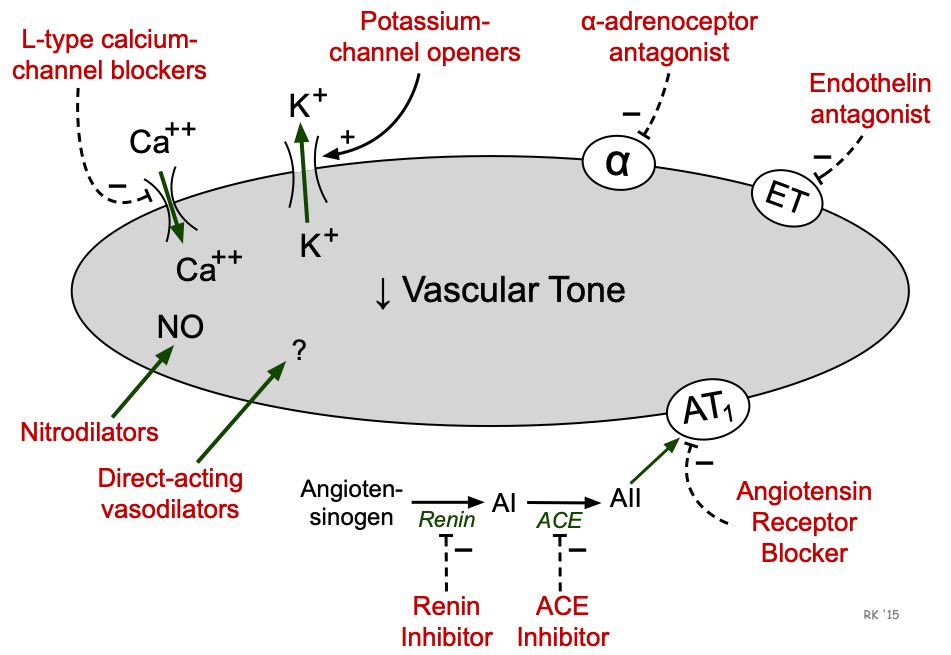
Mechanism of Action
Smooth Muscle Relaxation
Arterial Vasodilation
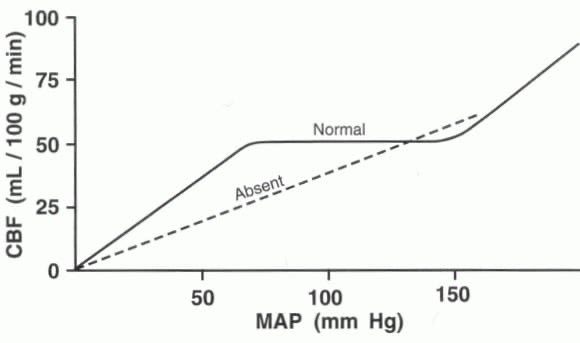
Cerebral Blood Flow
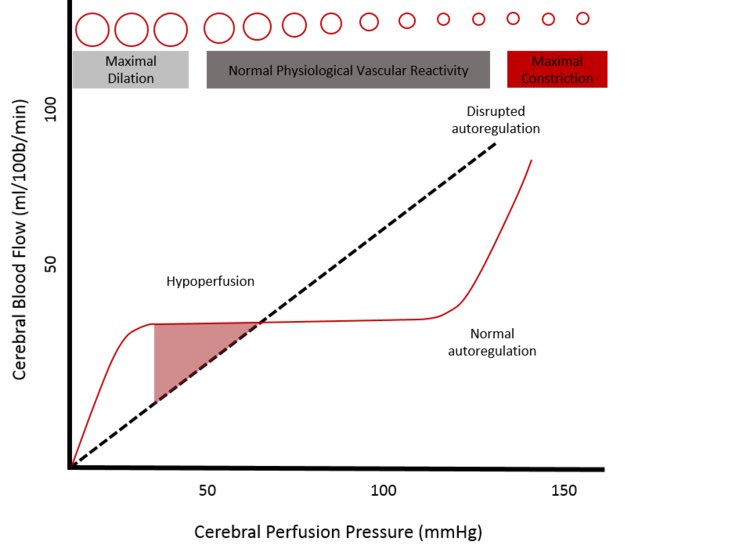
Cerebral Autoregulation
Let’s discuss (one of the many) reasons why hydralazine should be used with caution ⚠️ in the NeuroICU
Hydralazine 💉 can NEGATIVELY ✖️ impact cerebral hemodynamics 🧠 and cause an ⤴️ in ICP 💦
But the question is, how? 🤔
A #Neurotwitter 🧵
Hydralazine 💉 can NEGATIVELY ✖️ impact cerebral hemodynamics 🧠 and cause an ⤴️ in ICP 💦
But the question is, how? 🤔
A #Neurotwitter 🧵
4/n So.. what about the hydralazine (HDLZ)? 🤔
⭐️HDLZ = POTENT vasodilator ▶️rapid, significant⤵️in MAP➡️⬇️CPP
⭐️HDLZ ALSO dilates cerebral vessels (arteries>veins)▶️further impairing (the already impaired) cerebral autoregulation in 🧠 injuries
But wait, there’s more! ⚠️👇🏻
⭐️HDLZ = POTENT vasodilator ▶️rapid, significant⤵️in MAP➡️⬇️CPP
⭐️HDLZ ALSO dilates cerebral vessels (arteries>veins)▶️further impairing (the already impaired) cerebral autoregulation in 🧠 injuries
But wait, there’s more! ⚠️👇🏻
5/n The “cerebral steal” phenomenon 😯
Similar to coronary🫀steal
🌟If blood vessels within abnormal brain regions are selectively responsive to vasodilators ➡️ then ⬆️perfusion in only select regions leaving other areas poorly perfused may result in risk of ischemia 🧠
Similar to coronary🫀steal
🌟If blood vessels within abnormal brain regions are selectively responsive to vasodilators ➡️ then ⬆️perfusion in only select regions leaving other areas poorly perfused may result in risk of ischemia 🧠
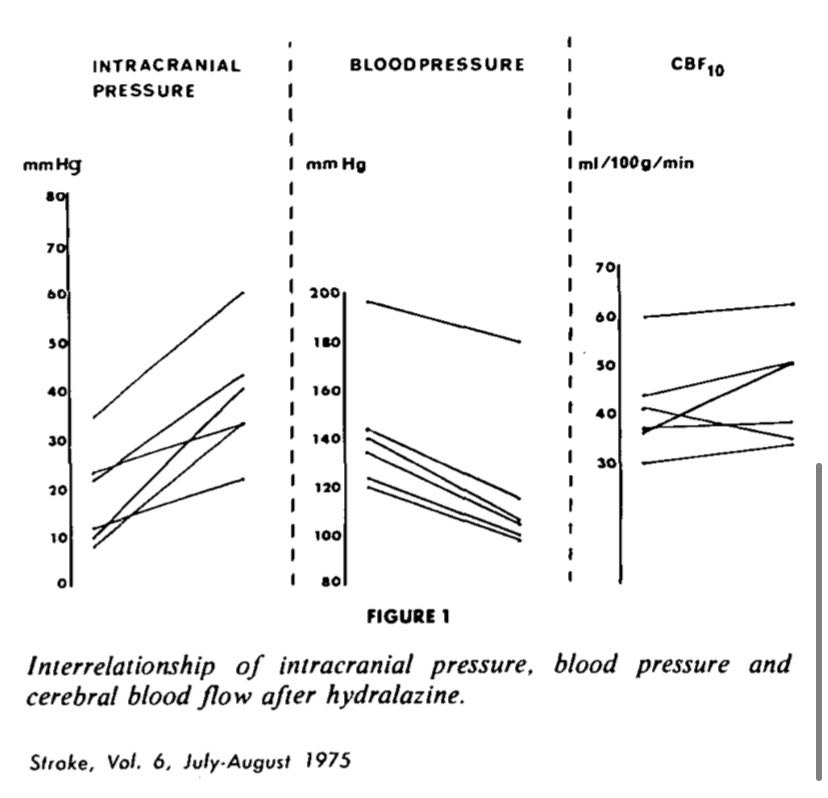
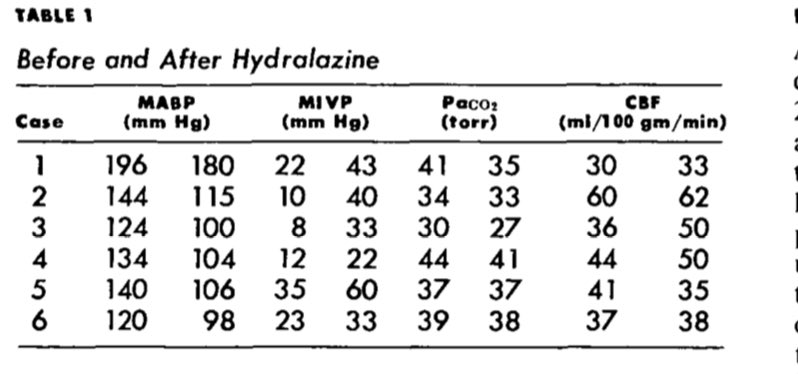
6/n Here is one of the first cases that was reported back in the 1970s describing increased ICP with hydralazine
🚨 alarming to note, authors found an ~ 20% reduction in SBP after a single dose of 12-18 mg of hydralazine that lead to a 110% ⬆️ in ICP ⚠️
ahajournals.org
🚨 alarming to note, authors found an ~ 20% reduction in SBP after a single dose of 12-18 mg of hydralazine that lead to a 110% ⬆️ in ICP ⚠️
ahajournals.org
All that being said, hope this provided insight on 1 (of the many) reasons to consider alt BP meds in 🧠injured pts!
Thanks to @pouyeah for inspiring this 🧵
Any additional pearls? @CaseyMayPharmD @KeatonSmetana @GilbertPharmD @caseyalbin @tigernole13 @AJWPharm @UFNeuroICU
Thanks to @pouyeah for inspiring this 🧵
Any additional pearls? @CaseyMayPharmD @KeatonSmetana @GilbertPharmD @caseyalbin @tigernole13 @AJWPharm @UFNeuroICU
Loading suggestions...