🧵
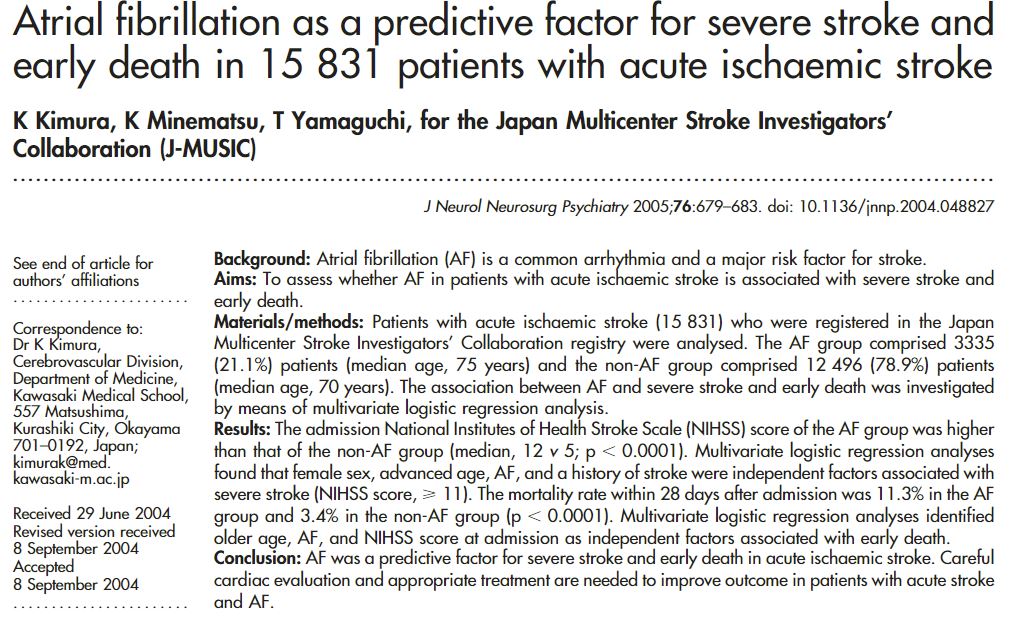
A brief 🧵 about the role of A-Fib in modifying outcomes after stroke, IV tPA complications, and thrombectomy, and new data about how bridging may increase risk for these patients, from @EmoryNeurosurg @EmoryNeuroCrit @EmoryNeurology
1/
jnis.bmj.com
A brief 🧵 about the role of A-Fib in modifying outcomes after stroke, IV tPA complications, and thrombectomy, and new data about how bridging may increase risk for these patients, from @EmoryNeurosurg @EmoryNeuroCrit @EmoryNeurology
1/
jnis.bmj.com
So that begs the question:
Is there an AF penalty for stroke in the endovascular era? Do AF patients still have more complications and worse outcomes with mechanical thrombectomy, or is MT somehow different?
Is there an AF penalty for stroke in the endovascular era? Do AF patients still have more complications and worse outcomes with mechanical thrombectomy, or is MT somehow different?
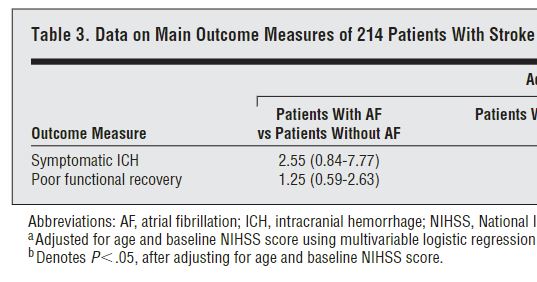
Nope, AF patients respond differently to MT than IVT.
After MT, there is no difference in either outcomes or hemorrhagic complications with respect to AF status.
Interestingly, anecdote about AF clots held true, big AF clots come out faster too!
jnis.bmj.com
After MT, there is no difference in either outcomes or hemorrhagic complications with respect to AF status.
Interestingly, anecdote about AF clots held true, big AF clots come out faster too!
jnis.bmj.com
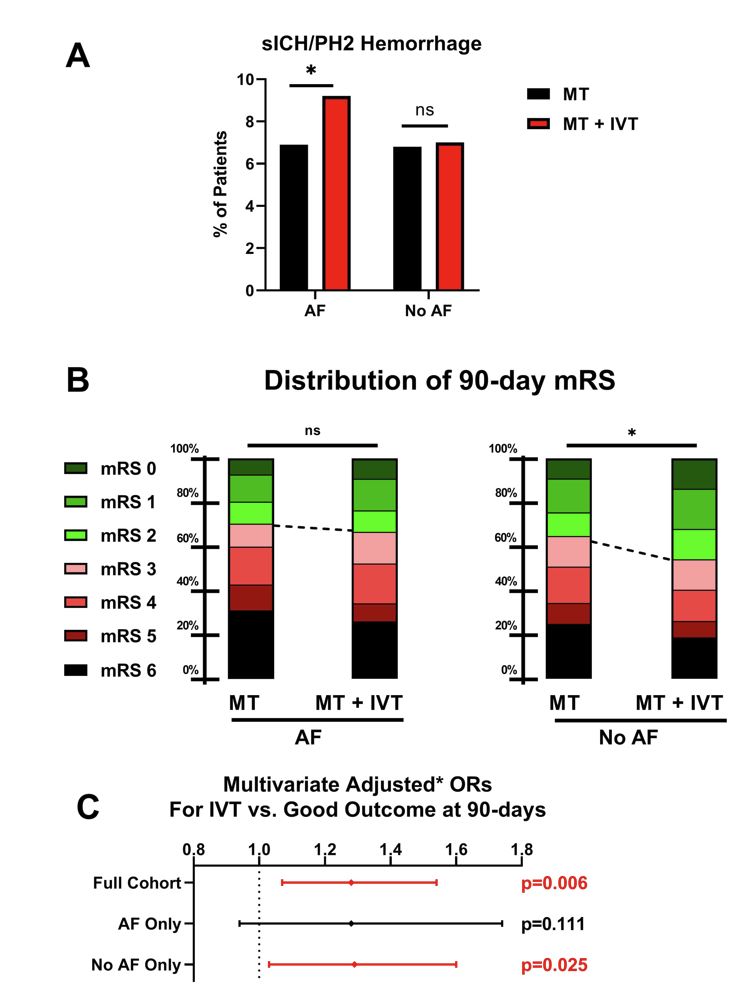
Working with @MUSC_STAR, @AliAlawiehmdphd,@BrianHoward_MD, @alex_spiotta, @JAGrossbergMD, we reviewed >6000 MT patients to ask whether AF modified the effect of bridging therapy, now out in JNIS.
jnis.bmj.com
jnis.bmj.com
Why?
Not sure, but likely enriching for fast progressors (no preconditioning with AF) and thus more infarcted territory prone to bleed.
2 corroborating pieces of evidence to support this idea.
1) A similar finding has has been reported in ICA-T clots
jnis.bmj.com
Not sure, but likely enriching for fast progressors (no preconditioning with AF) and thus more infarcted territory prone to bleed.
2 corroborating pieces of evidence to support this idea.
1) A similar finding has has been reported in ICA-T clots
jnis.bmj.com
2) Interestingly, SHRINE meta-analysis of DEVT and SKIP RCTs reported similarly increased ICH (and inc mortality at 90d) for bridging therapy in AF patients (and ICA T occlusions). Manuscript pending.
professional.heart.org
professional.heart.org
⚠️Lack of AC data is a key limitation in our dataset.
But think about who gets IVT: The AF patient on vs. not on AC? Clearly, the one not on AC.
So, AF patients getting IVT, those LEAST likely to be on AC, are those who are bleeding most in the @musc_star experience.
But think about who gets IVT: The AF patient on vs. not on AC? Clearly, the one not on AC.
So, AF patients getting IVT, those LEAST likely to be on AC, are those who are bleeding most in the @musc_star experience.
We’re working to externally validate these observations with collaborators, but perhaps we need to reframe the bridging therapy debate.
It’s not bridging good or bad, but specific patients at risk for benefit or harm. Maybe consider fast progressors, bigger strokes, etc
It’s not bridging good or bad, but specific patients at risk for benefit or harm. Maybe consider fast progressors, bigger strokes, etc
The work continues to externally validate our findings and identify patients at risk, but this couldn’t have been done without key @musc_star partners @PascalJabbourMD, @Starkeneurosurg, @Ansaar_Rai, @rdeleacymd, @PeterKa80460001, @AdamArthurMD, @JMoccoMD, @rocrossa, @wchrisfox.
Loading suggestions...