Can Cerebellum be affected in seizures??
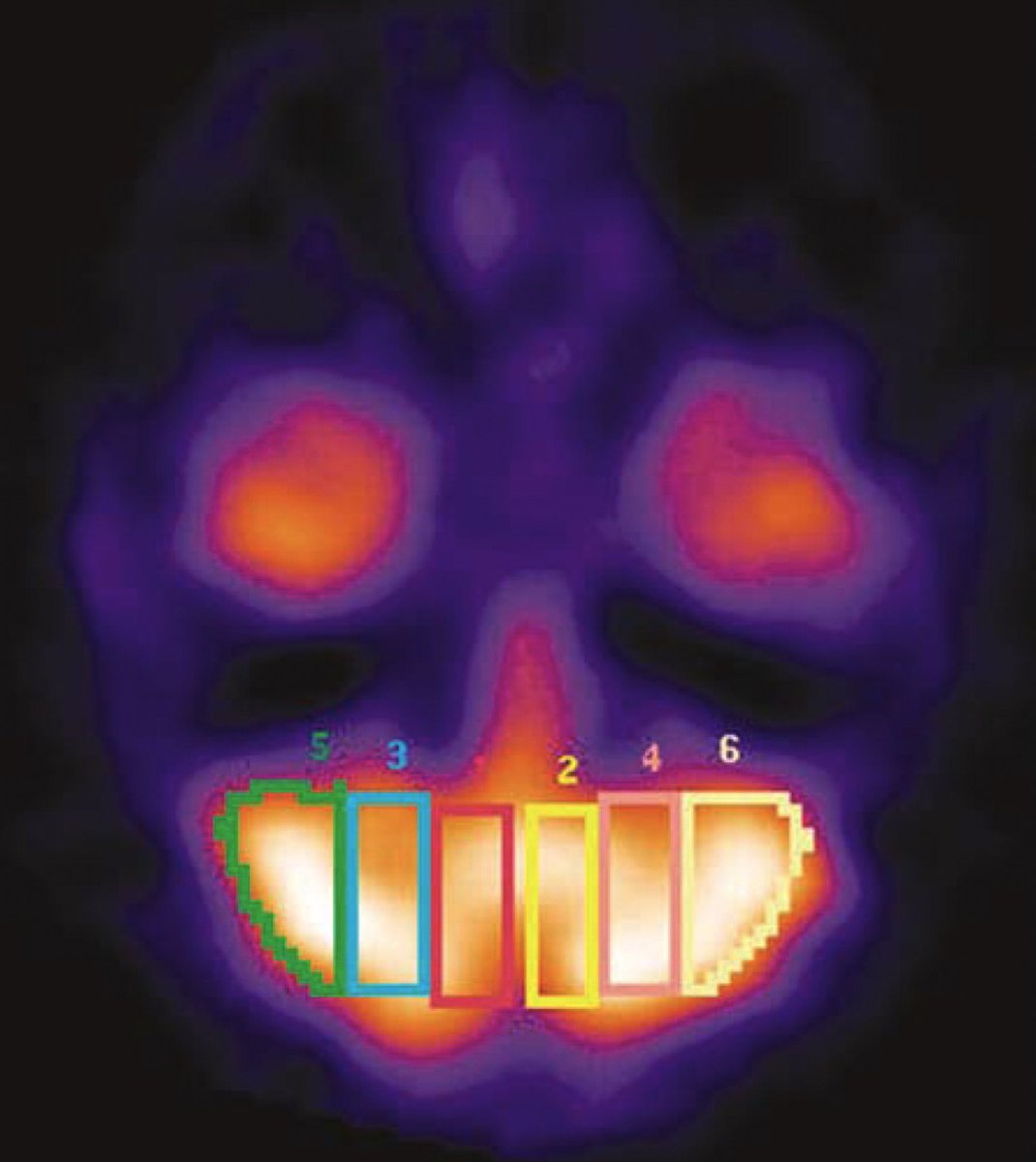
Can cerebellar perfusion predict outcome of cerebral hemispheric stroke??
Find out more below !!
Can cerebellar perfusion predict outcome of cerebral hemispheric stroke??
Find out more below !!
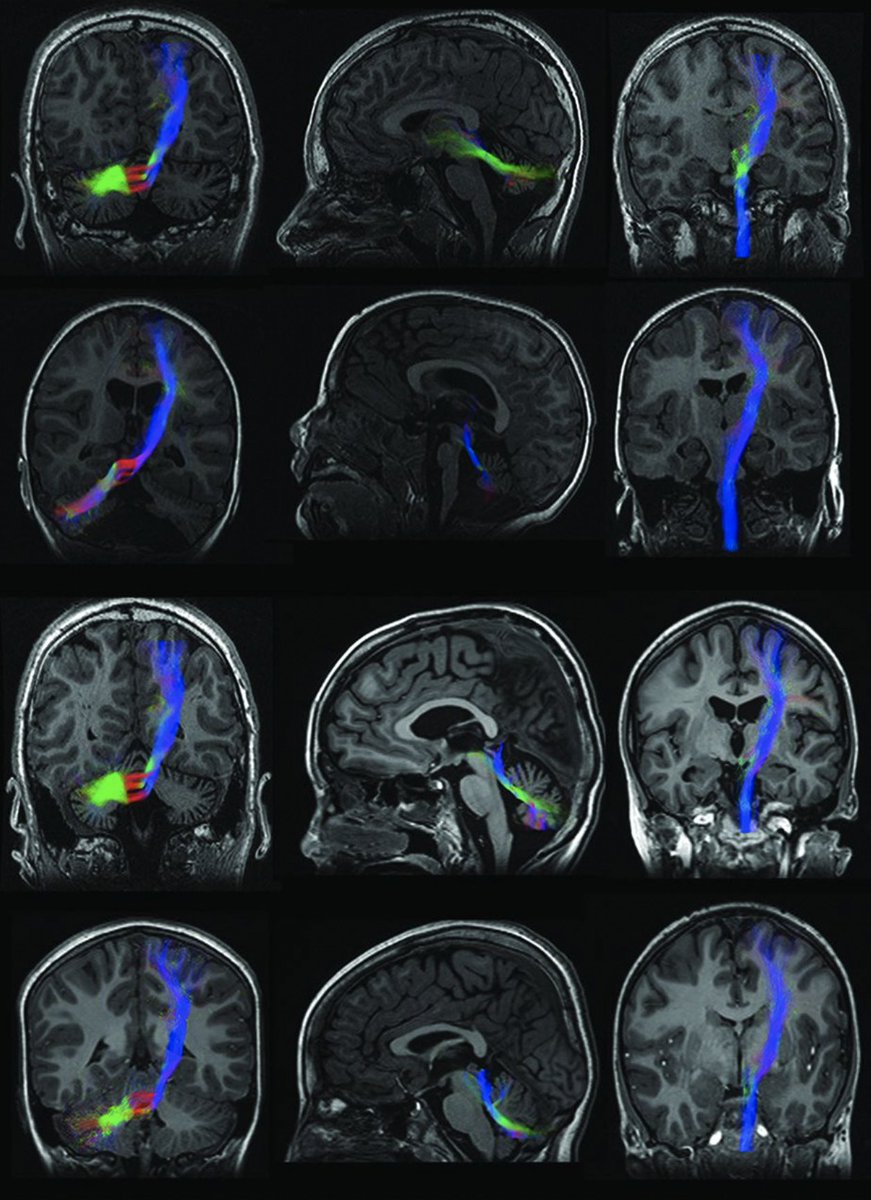
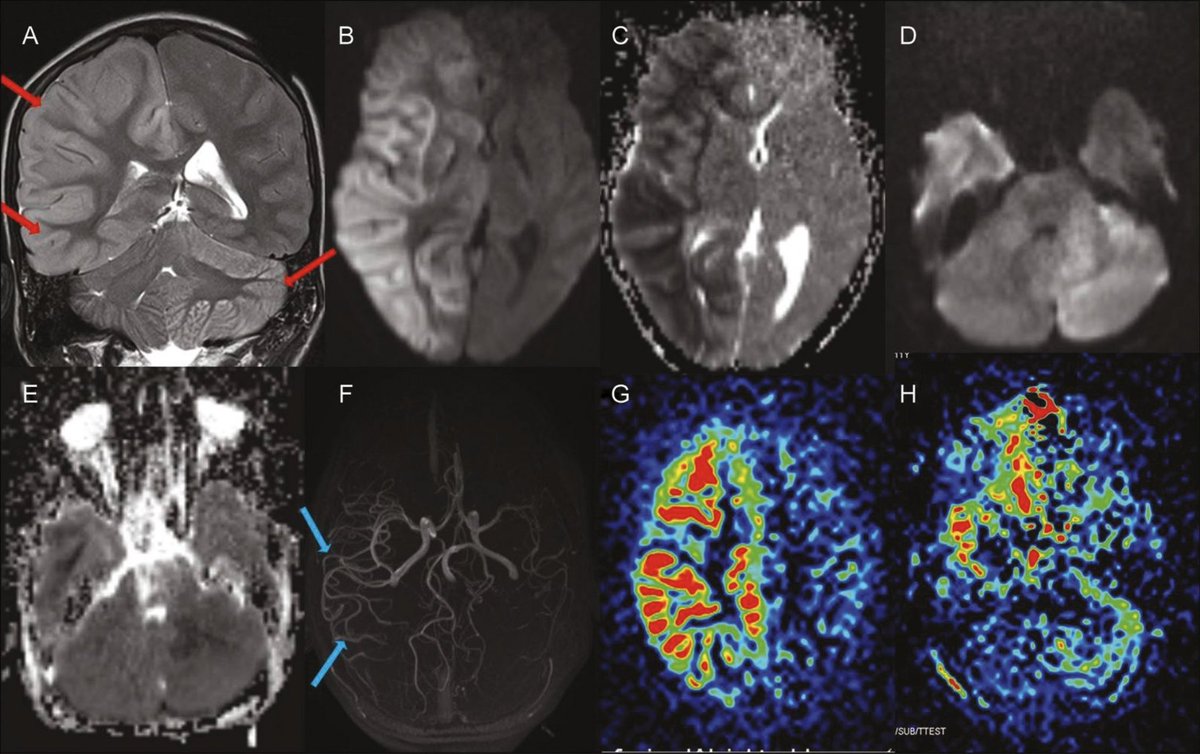
Shows DWI and FLAIR hyper intensity in the left hemisphere and right cerebellum..
Have a look again if missed the first time..
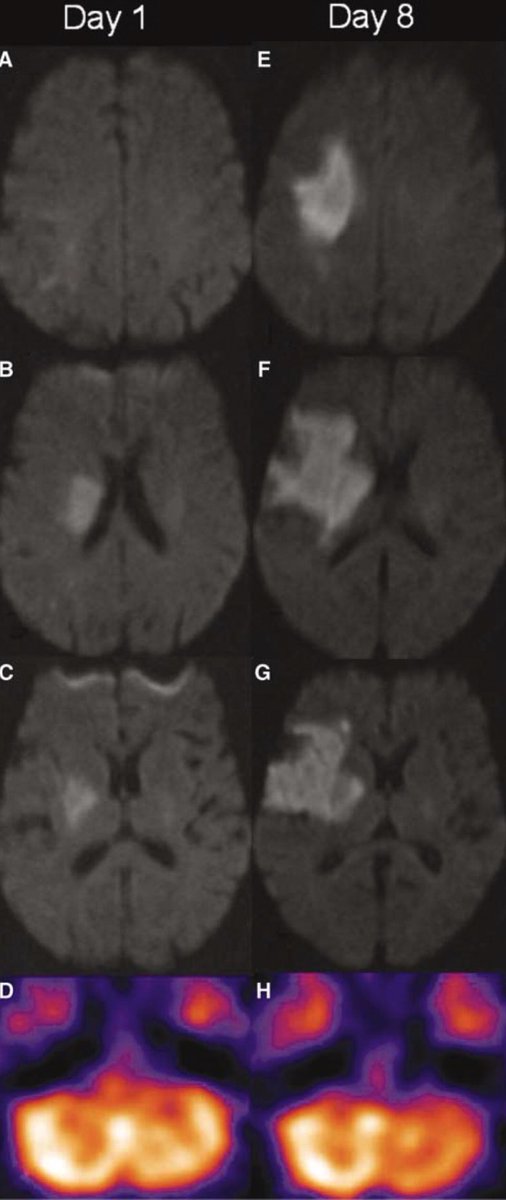
What’s your thought about origin of the patient’s seizures based on this MRI brain above?
Have a look again if missed the first time..
What’s your thought about origin of the patient’s seizures based on this MRI brain above?
If you correctly answered first question, congrats! Here’s your second chance if you didn’t. If we divide the images BELOW⬇️ in 3 columns, column 1, 2 and 3 from left to right, which column you think will provide the answer of the above question?
So why does this happen?
-Ischemic/hemorrhagic stroke
-Epilepsy/Focal status
-Tumors/Diffuse gliomas-32737798
-Alzheimer’s disease-33622918
-CJD-30308445
-NMDA encephalitis-32061394/Rasmussen encephalitis-20473513
-Sturge-Weber-2288389
-Familial hemiplegic migraine(FHM)-9385760
-Ischemic/hemorrhagic stroke
-Epilepsy/Focal status
-Tumors/Diffuse gliomas-32737798
-Alzheimer’s disease-33622918
-CJD-30308445
-NMDA encephalitis-32061394/Rasmussen encephalitis-20473513
-Sturge-Weber-2288389
-Familial hemiplegic migraine(FHM)-9385760
Did you recognize the pattern here?
Every etiology includes cortical involvement (Tumors, too) & are mostly unilateral supratentorial cerebral pathologies. So in order to have contralateral cerebellar involvement, there has to be some connection between the two.
Every etiology includes cortical involvement (Tumors, too) & are mostly unilateral supratentorial cerebral pathologies. So in order to have contralateral cerebellar involvement, there has to be some connection between the two.
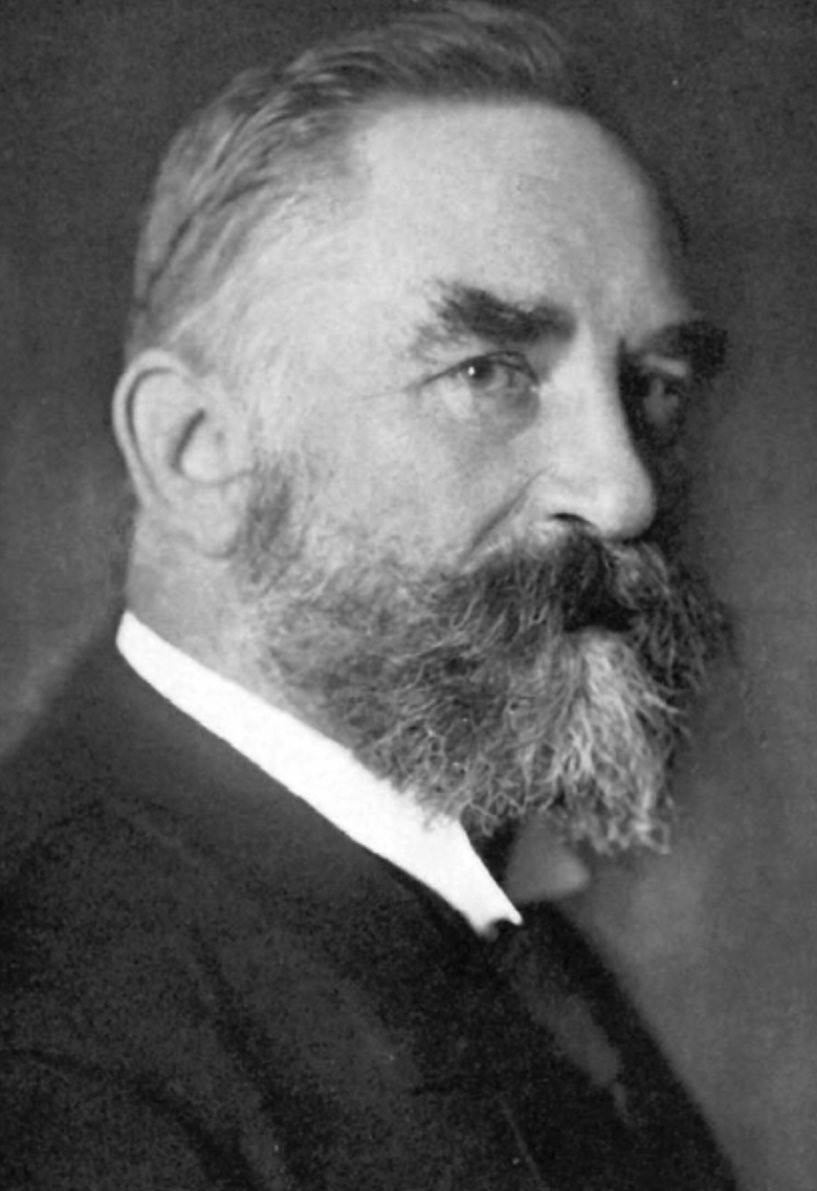
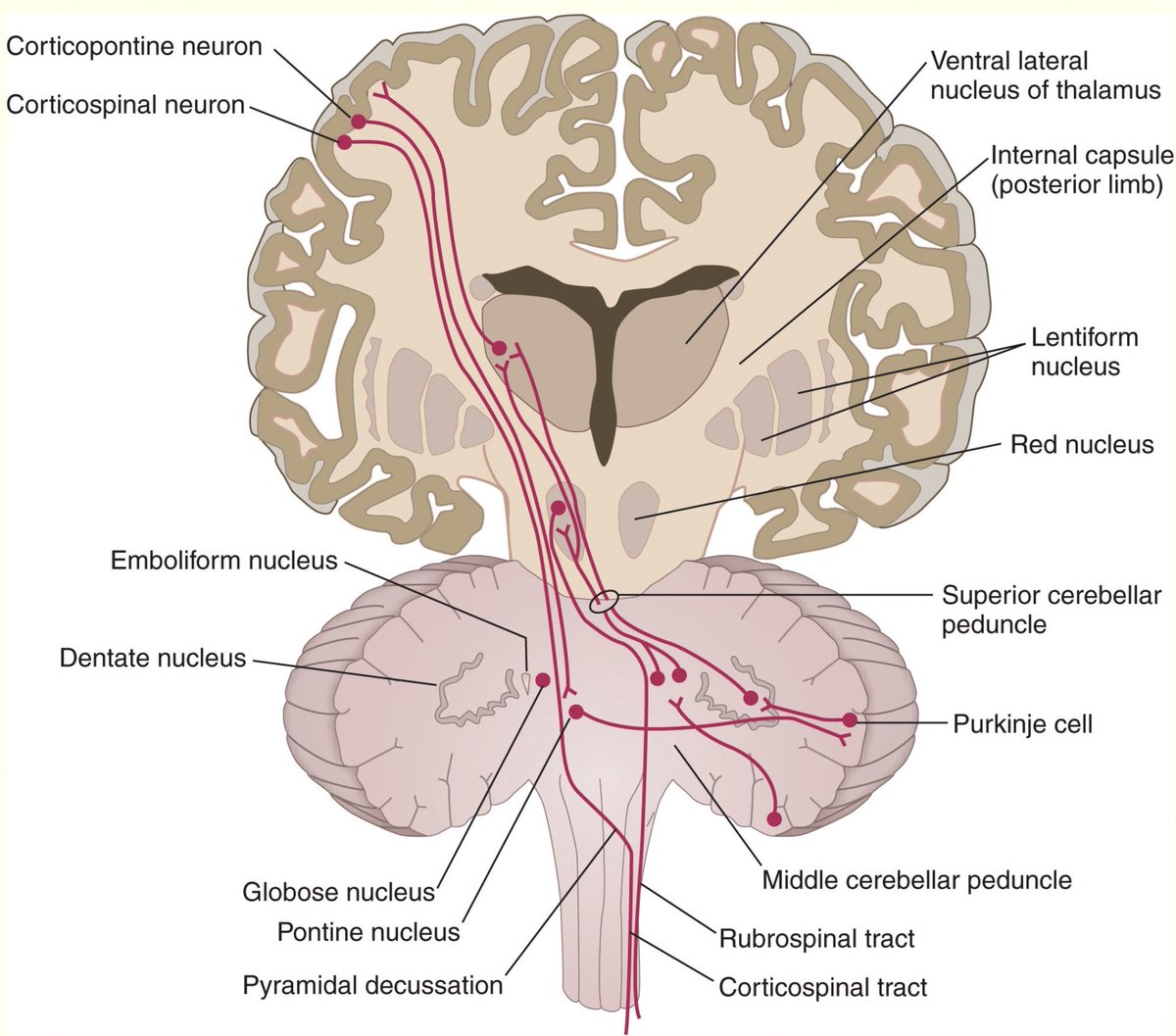
So there it is- Cortico-ponto-cerebellar (CPC) pathway.
For a plot twist, basal ganglia hemorrhagic strokes have also been found to cause CCD! (Brain isn’t always straight forward friends. If so, we - neurologists wouldn’t exist!)
Image source: humanphysiology.academy
For a plot twist, basal ganglia hemorrhagic strokes have also been found to cause CCD! (Brain isn’t always straight forward friends. If so, we - neurologists wouldn’t exist!)
Image source: humanphysiology.academy
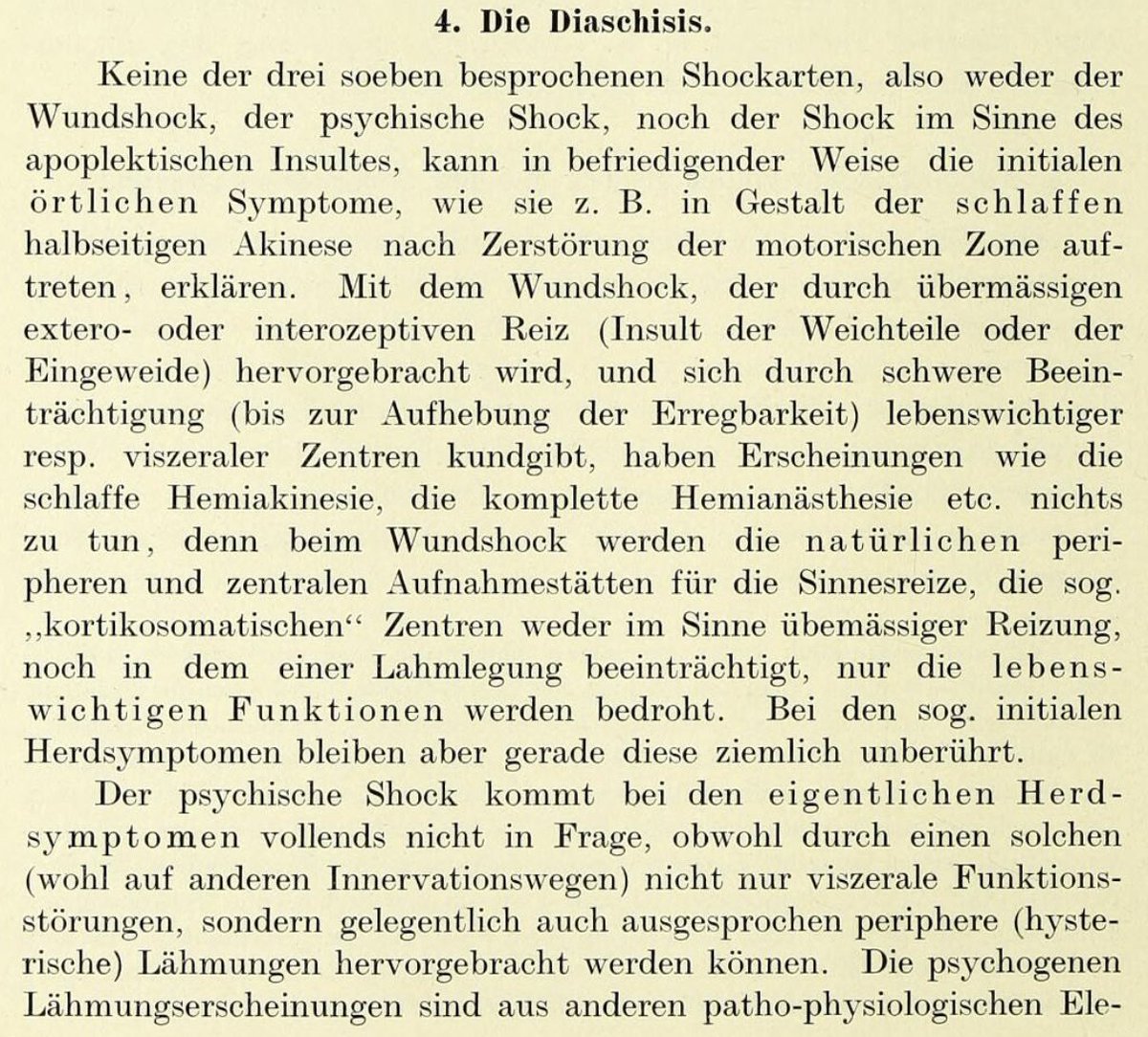
So how this happens in the first place?
🤔
The cerebellum has a significant input from the cerebral hemispheres, the bulk of which is contained in the CPC pathway. The densest cortico-ponto-cerebellar projections arise from the precentral and prefrontal cortical areas-22473241
🤔
The cerebellum has a significant input from the cerebral hemispheres, the bulk of which is contained in the CPC pathway. The densest cortico-ponto-cerebellar projections arise from the precentral and prefrontal cortical areas-22473241
Other cerebro-cerebellar connections are relayed through the inferior olive and reticular formation.
Other pathways postulated in pathophysiology are:
-cerebello-thalamo-cortical (CTC) pathway
-Spinocerebellar tract-2396276
-dentato-rubro-thalamic tract-10929283
Other pathways postulated in pathophysiology are:
-cerebello-thalamo-cortical (CTC) pathway
-Spinocerebellar tract-2396276
-dentato-rubro-thalamic tract-10929283
Now we know the pathway connecting the cerebrum with contralateral cerebellum, let’s understand the mechanism, which depends on the etiology only!!
1.Excitotoxicity(Epilepsy,ICH,CJD,encephalitis,SWS)
2.⬇️ blood flow due to cortical neuronal death (stroke,tumors,Alzheimer,FHM)
1.Excitotoxicity(Epilepsy,ICH,CJD,encephalitis,SWS)
2.⬇️ blood flow due to cortical neuronal death (stroke,tumors,Alzheimer,FHM)
⬇️blood flow due to cortical neuronal death:
Described in SUBACUTE-CHRONIC phase, often IRREVERSIBLE. The proposed mechanism- Cortical neuronal degeneration following insult (stroke, Alzheimer’s) causes transsynaptic neuronal degeneration 2/2 ⛔️of CPC pathway.
Described in SUBACUTE-CHRONIC phase, often IRREVERSIBLE. The proposed mechanism- Cortical neuronal degeneration following insult (stroke, Alzheimer’s) causes transsynaptic neuronal degeneration 2/2 ⛔️of CPC pathway.
Now since we have understood this amazing phenomenon, what’s the practical implication? Or this is just a cool neurology talk with nothing to offer clinically? - like many used to think?
Well, not quite. Knowing CCD progression & mechanism can help with prognostication.
Read⬇️
Well, not quite. Knowing CCD progression & mechanism can help with prognostication.
Read⬇️
Moral:
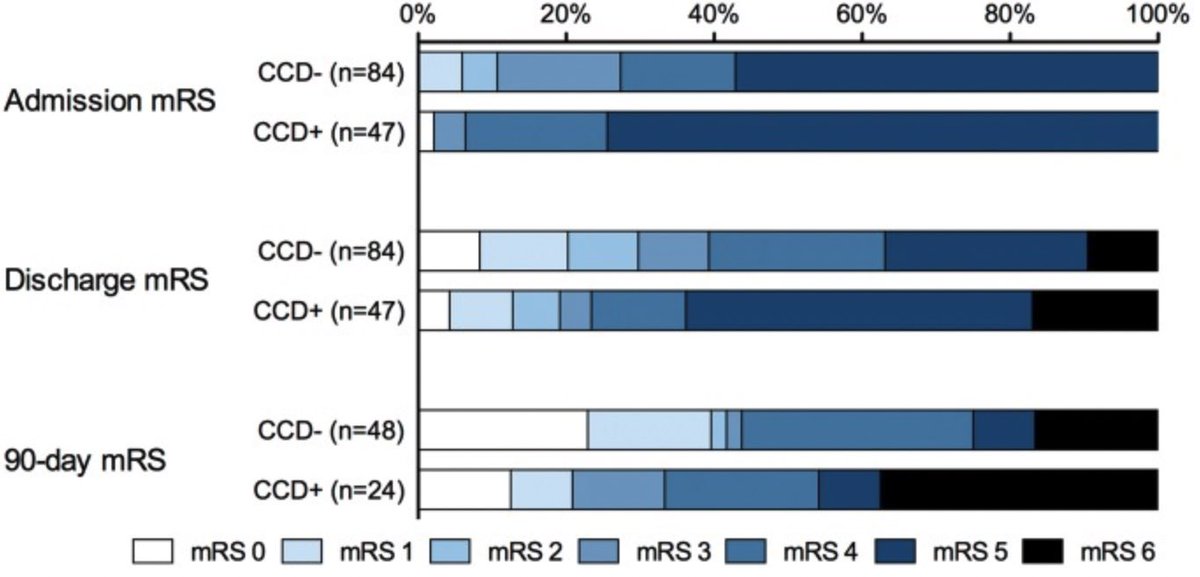
1. Mere presence of CCD in acute phase has no impact on functional outcome in ischemic stroke patients but persistence of CCD is associated with poor mRS-8126499
2. Occurrence of CCD with ICH;not hemorrhagic infarction = poor outcome compared to hemorrhagic infarct.
1. Mere presence of CCD in acute phase has no impact on functional outcome in ischemic stroke patients but persistence of CCD is associated with poor mRS-8126499
2. Occurrence of CCD with ICH;not hemorrhagic infarction = poor outcome compared to hemorrhagic infarct.
I find CCD an exceptional phenomenon revealing secrets of the brain that needs to be looked at closely! It offers an understanding of not only neuroanatomy but also clinical significance in terms of neurological outcome.
Who knows, one could use reverse physiology and gain control of intractable seizures through cerebellum using the same pathway or could stimulate neuroplasticity in cerebral cortex through cerebellum! Imagination has no limits.
Loading suggestions...