Important recent trials/studies in PCI, structural heart interventions, and adjunctive pharmacotherapy
❤️ PCI
▫️Antiplatelet, HBR, Complex, Multivessel, Devices, physiology and imaging
❤️ TAVI
▫️Antithrombotic, outcome, cerebral protection
#CardioTwitter
❤️ PCI
▫️Antiplatelet, HBR, Complex, Multivessel, Devices, physiology and imaging
❤️ TAVI
▫️Antithrombotic, outcome, cerebral protection
#CardioTwitter
❤️ PCI:
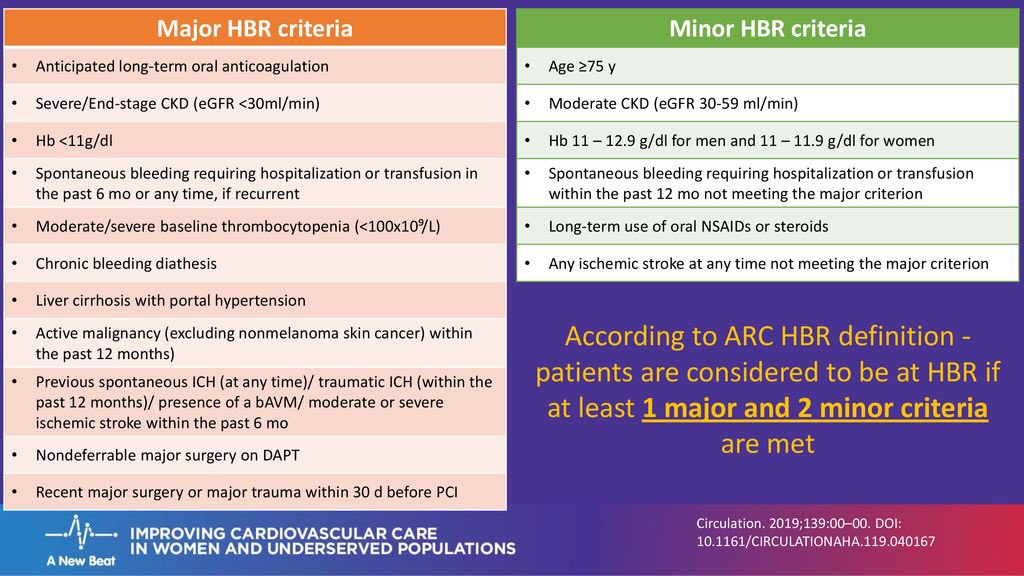
▫️Antiplatelet post PCI:
**STOPDAPT 2:
1 month DAPT noninferior to 12 months DAPT at preventing major ischemic events and superior to 12 months at preventing TIMI major/minor bleeding. BARC 3 or 5 bleeding was low, but 1 month also ⬇️ in this outcome compared w 12 months
▫️Antiplatelet post PCI:
**STOPDAPT 2:
1 month DAPT noninferior to 12 months DAPT at preventing major ischemic events and superior to 12 months at preventing TIMI major/minor bleeding. BARC 3 or 5 bleeding was low, but 1 month also ⬇️ in this outcome compared w 12 months
**TALOS AMI:
In pts with no major events in 1st month after index PCI, deescalation of DAPT switching from ticagrelor to clopidogrel is superior to continuing ticagtelor based DAPT in terms of net clinical benefit, with decreased bleeding risk and no increase in ischaemic risk
In pts with no major events in 1st month after index PCI, deescalation of DAPT switching from ticagrelor to clopidogrel is superior to continuing ticagtelor based DAPT in terms of net clinical benefit, with decreased bleeding risk and no increase in ischaemic risk
**MASTERDAPT trial:
1 month of DAPT following stent implantation in high bleeding risk patients preserves ischaemic benefits and reduces bleeding risk
1 month of DAPT following stent implantation in high bleeding risk patients preserves ischaemic benefits and reduces bleeding risk
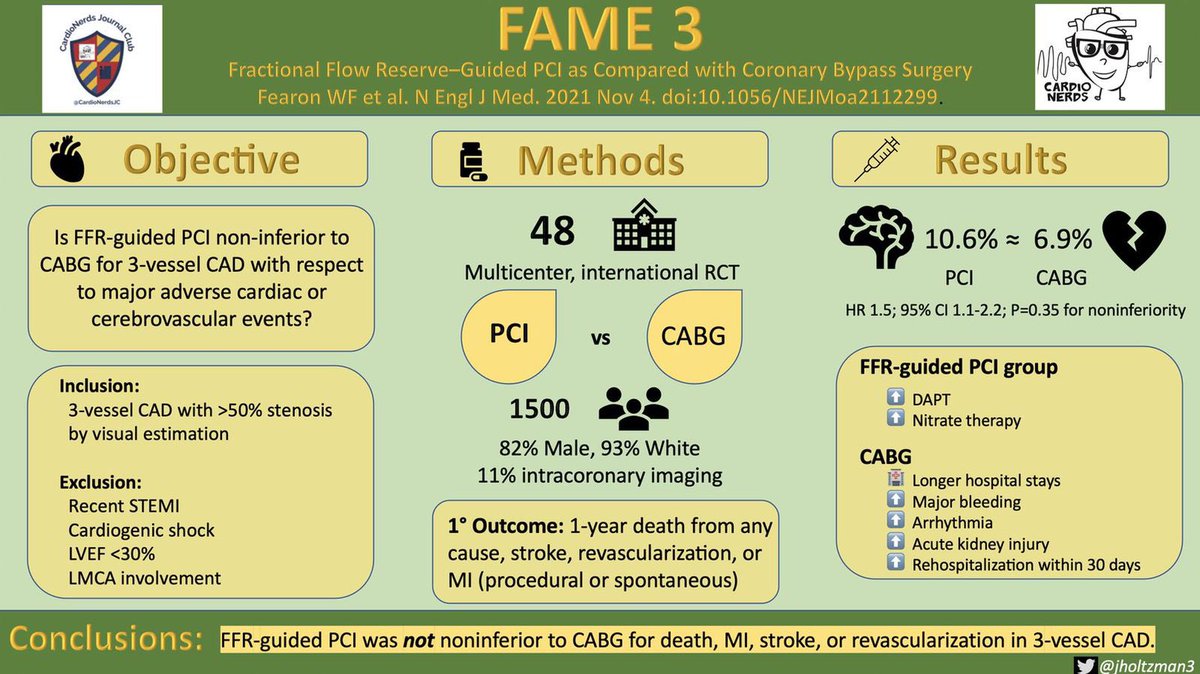
**FLOWER MI :
In STEMI Multivessels FFR guided Non culpril lesions treatment showed non superiority over angiography guided.
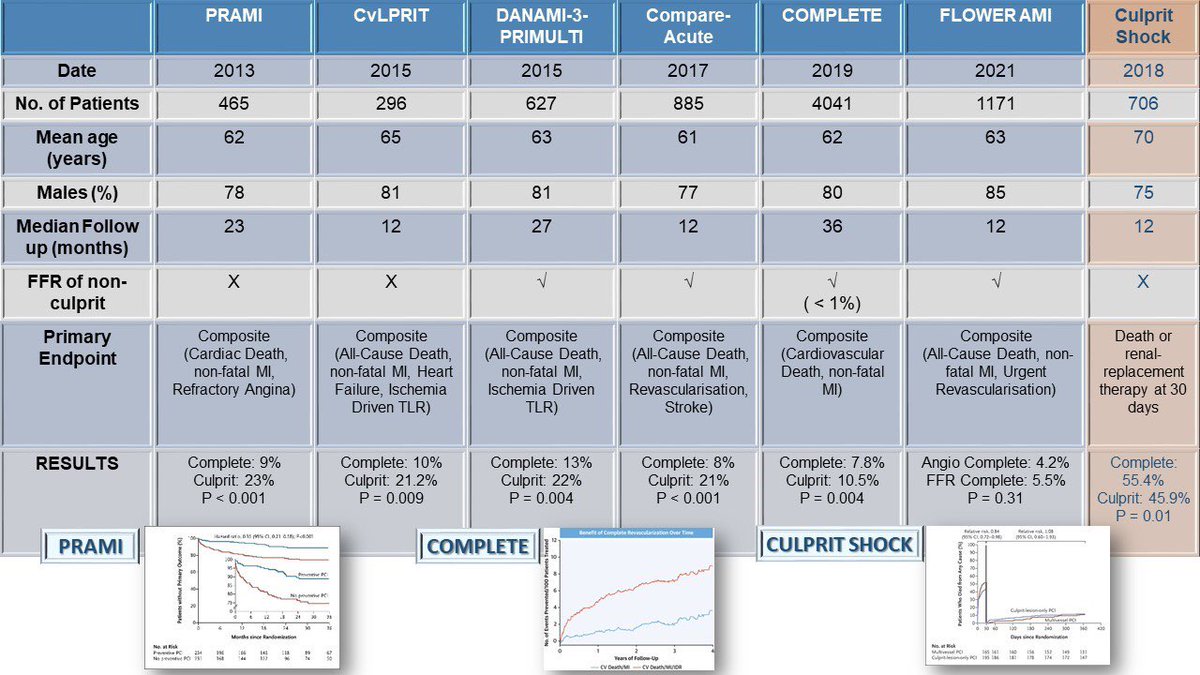
This is amazing table by @mirvatalasnag @drptca summarizes most relevant RCT of culprit-only versus complete revascularization in STEMI
In STEMI Multivessels FFR guided Non culpril lesions treatment showed non superiority over angiography guided.
This is amazing table by @mirvatalasnag @drptca summarizes most relevant RCT of culprit-only versus complete revascularization in STEMI
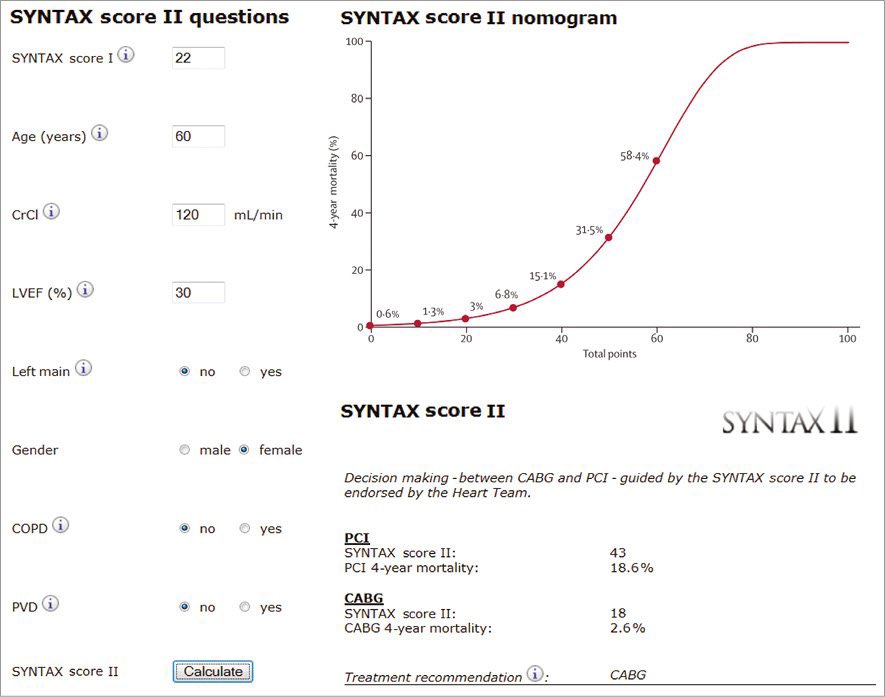
▫️Complex PCI :
**LM EBC :
Provisional vs Dual Stenting of LM ( w/ Resolute Onyx DES)
No sign. difference observed in end points : Death, MI and TLR at 1 year
**LM EBC :
Provisional vs Dual Stenting of LM ( w/ Resolute Onyx DES)
No sign. difference observed in end points : Death, MI and TLR at 1 year
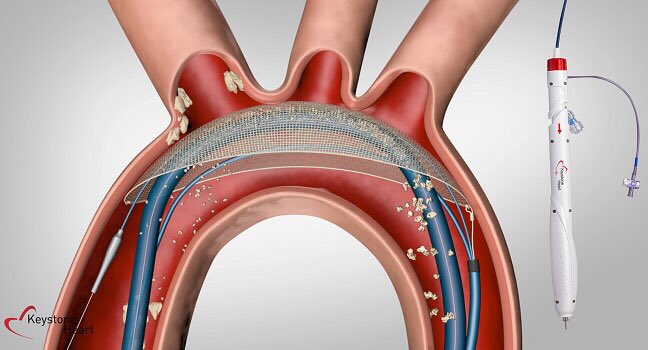
**DISTRUPT CAD :
Intravascular lithotripsy met performance goals for 30-day MACE and procedural success; clinical and angiographic complications low
Intravascular lithotripsy met performance goals for 30-day MACE and procedural success; clinical and angiographic complications low
▫️Physiology and imaging :
**TARGET FFR :
showed that a physiology guided optimization strategy didn’t significantly increase the proportion of pts achieving FFR ≥0.90 post cvPCI, but did significantly reduce the proportion of pts w/ final FFR ≤0.80.
**TARGET FFR :
showed that a physiology guided optimization strategy didn’t significantly increase the proportion of pts achieving FFR ≥0.90 post cvPCI, but did significantly reduce the proportion of pts w/ final FFR ≤0.80.
**FAVOR III China
A QFR-guided strategy improved PCI outcomes in patients compared with a standard angiography guided stragery.
A QFR-guided strategy improved PCI outcomes in patients compared with a standard angiography guided stragery.
**PROSPECT ABSORB :
suggest PCI of angiographically mild lesions with large plaque burden was safe & associated with favorable long term clinical outcomes.
suggest PCI of angiographically mild lesions with large plaque burden was safe & associated with favorable long term clinical outcomes.
▫️Devices :
**ULTRA-THIN STRUT DES :
We found no significant difference in clinical outcomes throughout 5 years between patients with small vessel disease treated with ultrathin-strut BP-SES versus thin-strut DP-EES.
**ULTRA-THIN STRUT DES :
We found no significant difference in clinical outcomes throughout 5 years between patients with small vessel disease treated with ultrathin-strut BP-SES versus thin-strut DP-EES.
**BASKET SMALL II :
In small native coronary artery disease, DCB was non-inferior to DES regarding MACE up to 12 months, with similar event rates for both treatment groups.
In small native coronary artery disease, DCB was non-inferior to DES regarding MACE up to 12 months, with similar event rates for both treatment groups.
❤️ TAVI :
▫️Antithrbombotic treatment :
**ATLANTIS :
After TAVI procedure, apixaban is not superior to standard of care (SOC) antithrombotic treatment in terms of net clinical benefit. Bleeding in apixaban is similar to that of current SOC, globally and in each stratum.
▫️Antithrbombotic treatment :
**ATLANTIS :
After TAVI procedure, apixaban is not superior to standard of care (SOC) antithrombotic treatment in terms of net clinical benefit. Bleeding in apixaban is similar to that of current SOC, globally and in each stratum.
** ENVISAGE-TAVI AF :
showed that edoxaban is noninferior to vitamin K antagonists for efficacy but did not meet criteria for noninferiority for bleeding among patients undergoing TAVR with AFib.
showed that edoxaban is noninferior to vitamin K antagonists for efficacy but did not meet criteria for noninferiority for bleeding among patients undergoing TAVR with AFib.
** GALILEO :
In pts w/o an established indication for OAC after TAVR, a treatment strategy including rivaroxaban at a dose of 10 mg daily was associated with a higher risk of death or thromboembolic complications and a higher risk of bleeding than an antiplatelet-based strategy.
In pts w/o an established indication for OAC after TAVR, a treatment strategy including rivaroxaban at a dose of 10 mg daily was associated with a higher risk of death or thromboembolic complications and a higher risk of bleeding than an antiplatelet-based strategy.
** POPULAR TAVI :
aspirin alone after TAVI reduces bleeding events and does not increase the rate of thromboembolic events
aspirin alone after TAVI reduces bleeding events and does not increase the rate of thromboembolic events
▫️Long term outcome :
** VIVID :
The size of the original failed valve may influence long-term mortality and the type of the transcatheter valve may influence the need for reintervention after aortic ViV.
** VIVID :
The size of the original failed valve may influence long-term mortality and the type of the transcatheter valve may influence the need for reintervention after aortic ViV.
**NOTION :
In pts w severe AS at low surgical risk randomized to TAVI or SAVR, there were no significant differences in the risk for all-cause mortality, stroke, or myocardial infarction, as well as the risk of bioprosthetic valve failure after 8 years of follow-up
In pts w severe AS at low surgical risk randomized to TAVI or SAVR, there were no significant differences in the risk for all-cause mortality, stroke, or myocardial infarction, as well as the risk of bioprosthetic valve failure after 8 years of follow-up
Loading suggestions...