What's going on with the intra-aortic balloon pump (IABP)?
Here's a practical🧵 for all residents and fellows during their time on rotation in the cardiac ICU.
Learning objectives
🎈 basics of the IABP
🎈 IABP alarms
🎈 ways to fix them
#CardioTwitter #Medtwitter #tweetorial
Here's a practical🧵 for all residents and fellows during their time on rotation in the cardiac ICU.
Learning objectives
🎈 basics of the IABP
🎈 IABP alarms
🎈 ways to fix them
#CardioTwitter #Medtwitter #tweetorial
Let's start with the basics.
Developed in the 1950s by the Kantrowitz brothers, IABPs have been in clinical practice since the first implant in 1967 at @MaimonidesMC Currently, it is still widely used as modest temporary mechanical circulatory support for cardiogenic shock
Developed in the 1950s by the Kantrowitz brothers, IABPs have been in clinical practice since the first implant in 1967 at @MaimonidesMC Currently, it is still widely used as modest temporary mechanical circulatory support for cardiogenic shock
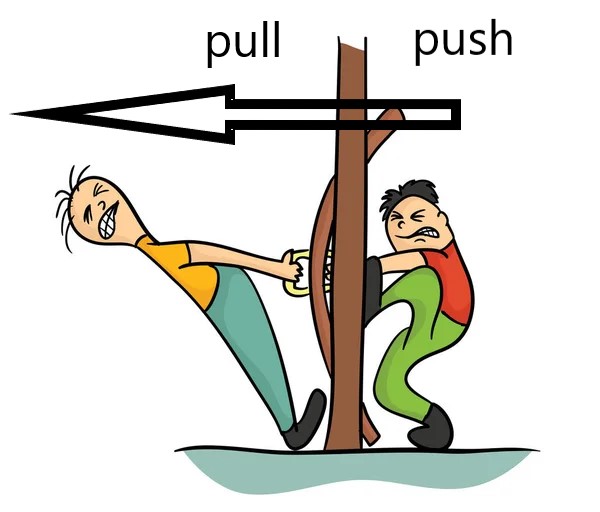
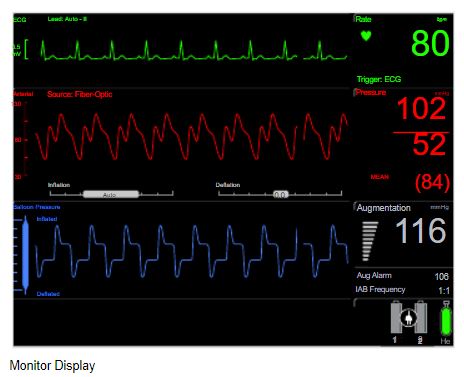
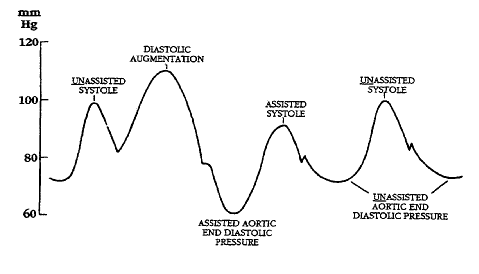
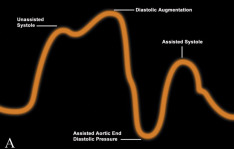
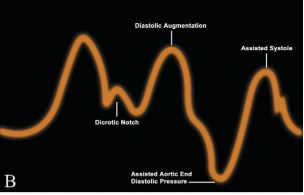
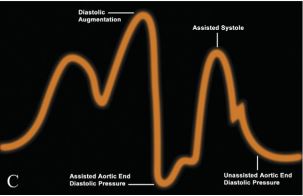
The mechanism of IABP begins with rapid deflation of the helium filled balloon (helium moves faster than air) at the onset of systole. This creates a vacuum effect which reduces the work load of the heart during all of systole thereby reducing afterload
This is followed by inflation of the balloon during all of diastole starting at the moment of aortic valve closure. This displaces blood from the thoracic aorta to peripheral tissues including the coronary arteries.
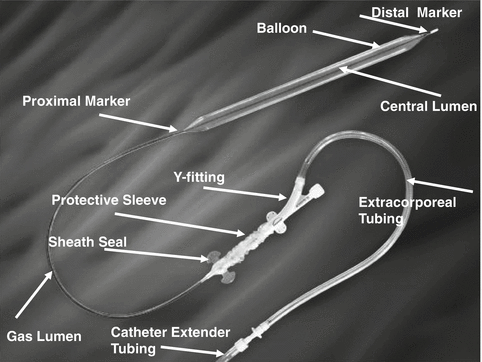
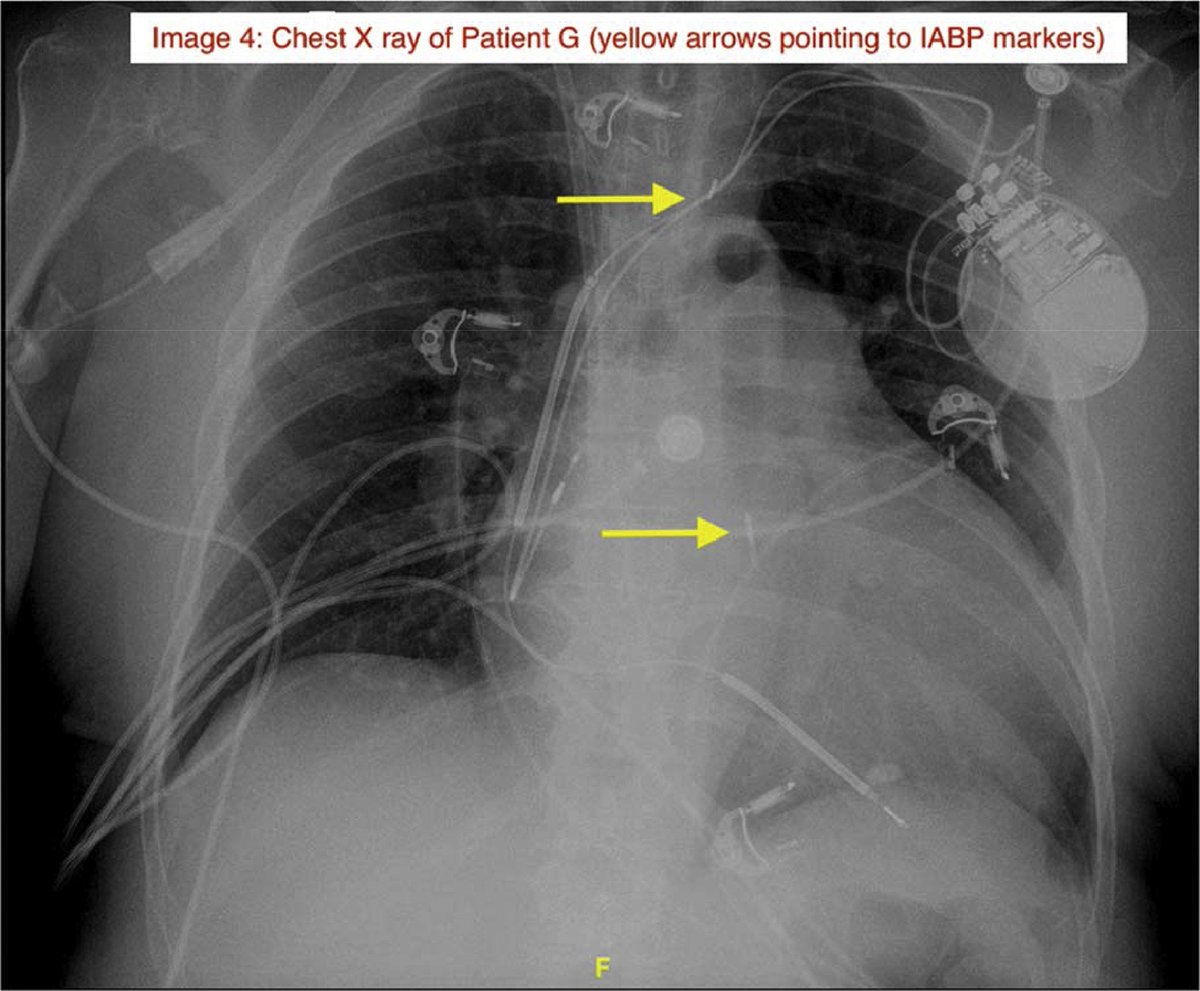
IABPs are properly positioned in the aorta below the left subclavian artery (have traditionally been placed transfemorally, but a common alternative is transaxillary which allows for easier ambulation if used for longer periods of time)
pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
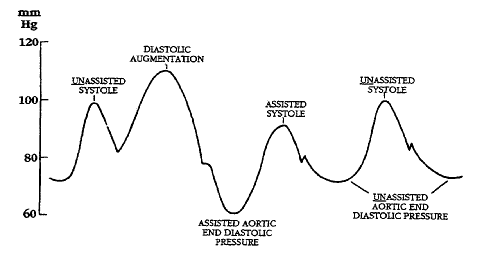
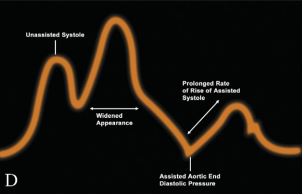
There are a number of scenarios that can occur as a result of mistiming of the IABP
⏲️ early inflation
⏲️ late inflation
⏲️ early deflation
⏲️ late deflation
Let's first start with the case of early inflation...
⏲️ early inflation
⏲️ late inflation
⏲️ early deflation
⏲️ late deflation
Let's first start with the case of early inflation...
So what happens when things go awry? Let's break it down into the major categories of IABP malfunction
🎈 balloon may not be adequately augmenting cardiac output (CO)
🎈 ECG trigger may not be functioning properly
🎈 flow of helium may be impaired or absent
🎈 balloon may not be adequately augmenting cardiac output (CO)
🎈 ECG trigger may not be functioning properly
🎈 flow of helium may be impaired or absent
Augmentation alarms can occur for many reasons:
⬇️ SVR or CO (sepsis, worsening cardiogenic shock, new arrhythmia)
⬇️ helium delivery to balloon (leak in catheter or gas circuit, 🎈rupture/tear)
⬇️ balloon function (incorrect timing, impaired 🎈 opening)
⬇️ SVR or CO (sepsis, worsening cardiogenic shock, new arrhythmia)
⬇️ helium delivery to balloon (leak in catheter or gas circuit, 🎈rupture/tear)
⬇️ balloon function (incorrect timing, impaired 🎈 opening)
How do we address augmentation alarms?
💔See the patient! How do they look?
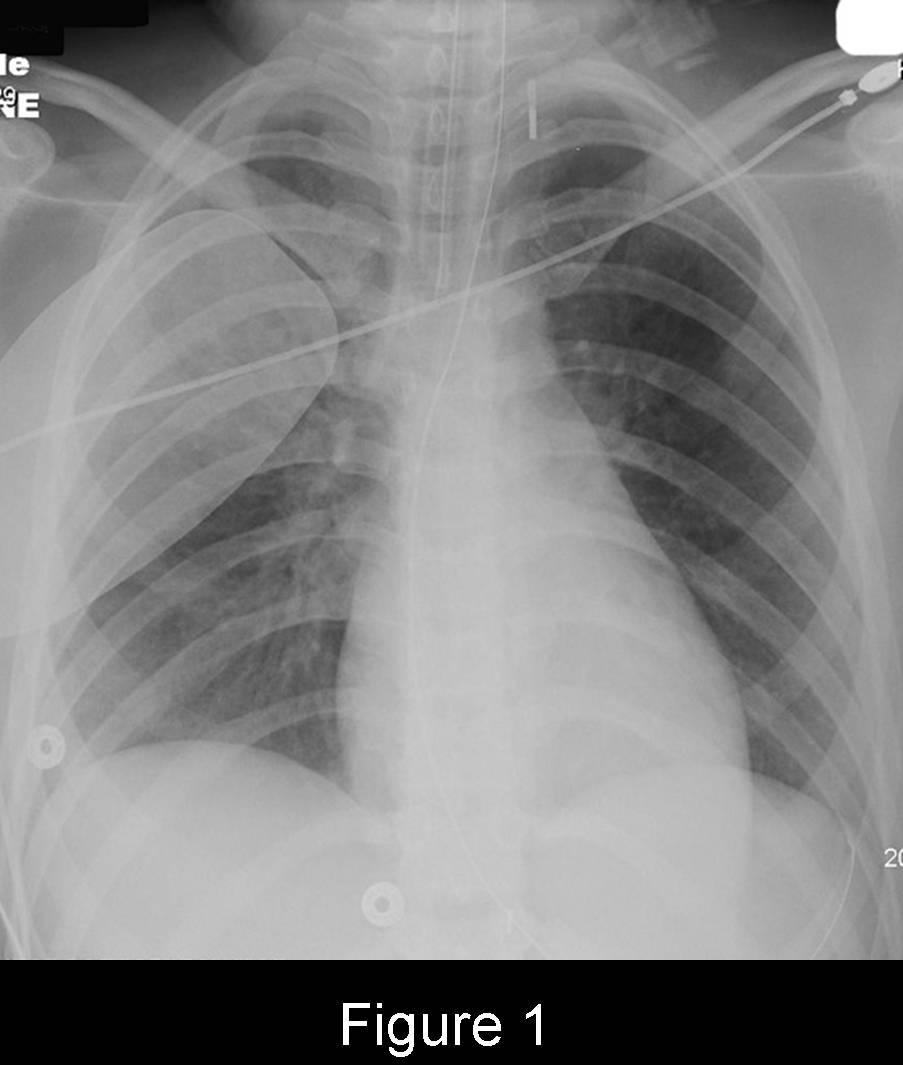
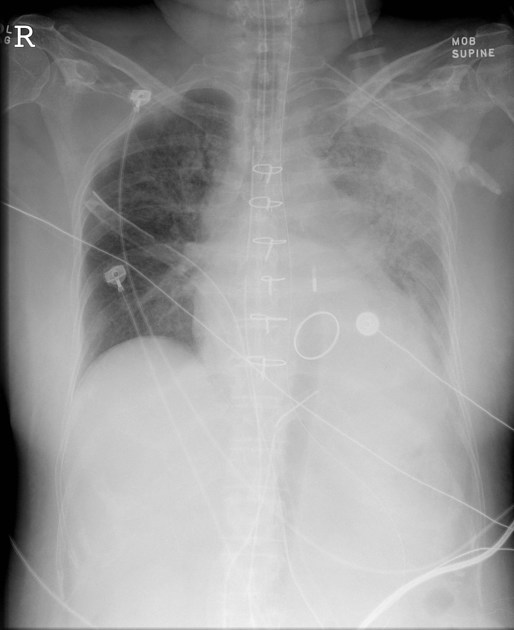
💔Confirm correct placement with CXR (marker 2cm above carina within aortic knob and 22-26cm apart)
💔Evaluate waveform, is it appropriate?
💔Address underlying cause (abx, inotropes, antiarrhythmics)
💔See the patient! How do they look?
💔Confirm correct placement with CXR (marker 2cm above carina within aortic knob and 22-26cm apart)
💔Evaluate waveform, is it appropriate?
💔Address underlying cause (abx, inotropes, antiarrhythmics)
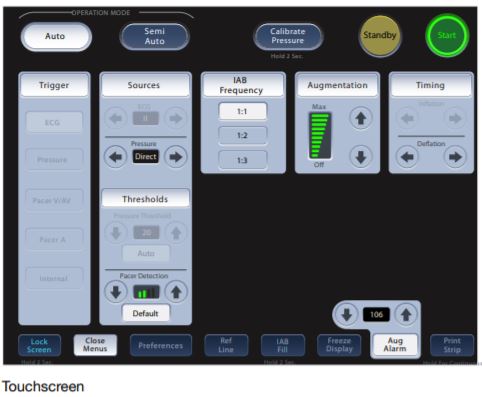
Failure of ECG triggering can occur due to:
💔Poor lead placement
💔Low ECG voltage
💔New arrhythmia (irregular R wave intervals make it difficult to trigger especially at ⬆️ heart rates )
💔Poor lead placement
💔Low ECG voltage
💔New arrhythmia (irregular R wave intervals make it difficult to trigger especially at ⬆️ heart rates )
How do we address issues with ECG triggering?
💔Check electrode placement and tracing for low voltage or new dysrhythmia (replace leads if needed)
💔Consider switching to arterial pressure triggering temporarily
💔if extreme tachycardia, reduce timing from 1:1 to 1:2 or 1:3
💔Check electrode placement and tracing for low voltage or new dysrhythmia (replace leads if needed)
💔Consider switching to arterial pressure triggering temporarily
💔if extreme tachycardia, reduce timing from 1:1 to 1:2 or 1:3
Impaired or absent helium flow indicates a non-functioning 🎈 and represents an emergency! Some causes are:
💔Restriction (in catheter or tubing, during inflation/deflation)
💔Helium loss from circuit
💔All out of helium
💔Restriction (in catheter or tubing, during inflation/deflation)
💔Helium loss from circuit
💔All out of helium
Remember, do not touch the IABP panel if you are not familiar and trained with the IABP and only if and when you have approval from your attending. If you are a resident, call your fellow and/or attending immediately if these issues arise.
Special thanks to @AHajduczok, Gregary Marhefka MD, Indranee Rajapreyar MD, and @YevgeniyBr for help with this🧵.
Recommendations for further reading:
pubmed.ncbi.nlm.nih.gov
jcvaonline.com
#relatedArticles" target="_blank" rel="noopener" onclick="event.stopPropagation()">onlinejcf.com
Recommendations for further reading:
pubmed.ncbi.nlm.nih.gov
jcvaonline.com
#relatedArticles" target="_blank" rel="noopener" onclick="event.stopPropagation()">onlinejcf.com
Loading suggestions...