2/
Firstly – don’t wait for confirmation of ⬆️K
🚨With this history & ECG, the diagnosis = ⬆️K
🚨It is also largely accepted that ECG sensitivity is poor, & subtle or non-classical changes prior to arrest are possible, so even without this ECG starting ⬆️K treatment sensible
Firstly – don’t wait for confirmation of ⬆️K
🚨With this history & ECG, the diagnosis = ⬆️K
🚨It is also largely accepted that ECG sensitivity is poor, & subtle or non-classical changes prior to arrest are possible, so even without this ECG starting ⬆️K treatment sensible
3/
Start usual advanced life support algorithm, plus:
👉 Get calcium in via good access
✅ 10ml calcium chloride 10% recommended, as doesn’t need hepatic metabolism like calcium gluconate
✅ repeat at 5-10 mins if no ROSC
If you do get ROSC, you still need to get the K down….
Start usual advanced life support algorithm, plus:
👉 Get calcium in via good access
✅ 10ml calcium chloride 10% recommended, as doesn’t need hepatic metabolism like calcium gluconate
✅ repeat at 5-10 mins if no ROSC
If you do get ROSC, you still need to get the K down….
4/
Does giving iv adrenaline (epinephrine) earlier than usual ALS protocol help?
Some experts say give it immediately as it’s fast acting & should hide K intracellularly - that’s what I’d do
(but even if just giving it as per usual ALS algorithm, the delay will be minimal)
Does giving iv adrenaline (epinephrine) earlier than usual ALS protocol help?
Some experts say give it immediately as it’s fast acting & should hide K intracellularly - that’s what I’d do
(but even if just giving it as per usual ALS algorithm, the delay will be minimal)
5/
Does iv insulin work? No one knows, but will take 15+ mins to even start.
UKKA recommend:
✔️Give 10 units iv insulin with 25g glucose (e.g. 125ml of dex 20%) via iv bolus
✔️If pre-treatment sugar on low side give additional dextrose infusion, aiming to avoid hypoglycaemia
Does iv insulin work? No one knows, but will take 15+ mins to even start.
UKKA recommend:
✔️Give 10 units iv insulin with 25g glucose (e.g. 125ml of dex 20%) via iv bolus
✔️If pre-treatment sugar on low side give additional dextrose infusion, aiming to avoid hypoglycaemia
6/
Sodium bicarb isn’t used in 'routine’ arrests BUT is for ⬆️K
🟢 Give 50ml iv NaHCO3 8.4%
⛔️ via different access to iv calcium
⁉️Conundrum: does the hypertonic sodium cause more stablisation of the cardiac membrane than the bicarb-driven ⬇️ionised calcium destablises it?⁉️
Sodium bicarb isn’t used in 'routine’ arrests BUT is for ⬆️K
🟢 Give 50ml iv NaHCO3 8.4%
⛔️ via different access to iv calcium
⁉️Conundrum: does the hypertonic sodium cause more stablisation of the cardiac membrane than the bicarb-driven ⬇️ionised calcium destablises it?⁉️
7/
Any drug effectiveness studies?
None without limitations.
Largest:
👉retrospective look at 109 arrests with ⬆️K
👉suggestion if both iv Ca & bicarb used can sometimes get ROSC up to K=9
👉No survivors when K >9.4
However, no patients were dialysed.
pubmed.ncbi.nlm.nih.gov
Any drug effectiveness studies?
None without limitations.
Largest:
👉retrospective look at 109 arrests with ⬆️K
👉suggestion if both iv Ca & bicarb used can sometimes get ROSC up to K=9
👉No survivors when K >9.4
However, no patients were dialysed.
pubmed.ncbi.nlm.nih.gov
8/
If patient was already dialysing does this change things?
Yes!
Most machines NOT shock-proof in UK
✳️Patient needs disconnected prior to shocking
✳️These stickers identify defib-proof machines👇
Survey in 2007 = 25% UK renal units unaware of above
resuscitationjournal.com
If patient was already dialysing does this change things?
Yes!
Most machines NOT shock-proof in UK
✳️Patient needs disconnected prior to shocking
✳️These stickers identify defib-proof machines👇
Survey in 2007 = 25% UK renal units unaware of above
resuscitationjournal.com
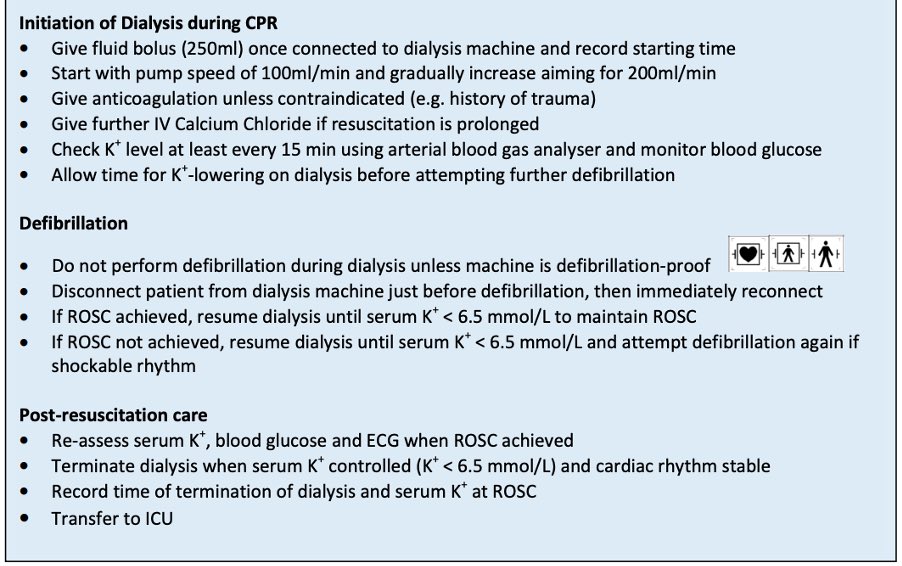
9/
And if not dialysing? Can consider STARTING during arrest when K refractory to medical therapy as:
1️⃣ ROSC unlikely unless get K controlled
2️⃣ Logical to use most effective treatment to ⬇️K, esp when very high
3️⃣ Case reports show feasibility & efficacy of dialysis during CPR
And if not dialysing? Can consider STARTING during arrest when K refractory to medical therapy as:
1️⃣ ROSC unlikely unless get K controlled
2️⃣ Logical to use most effective treatment to ⬇️K, esp when very high
3️⃣ Case reports show feasibility & efficacy of dialysis during CPR
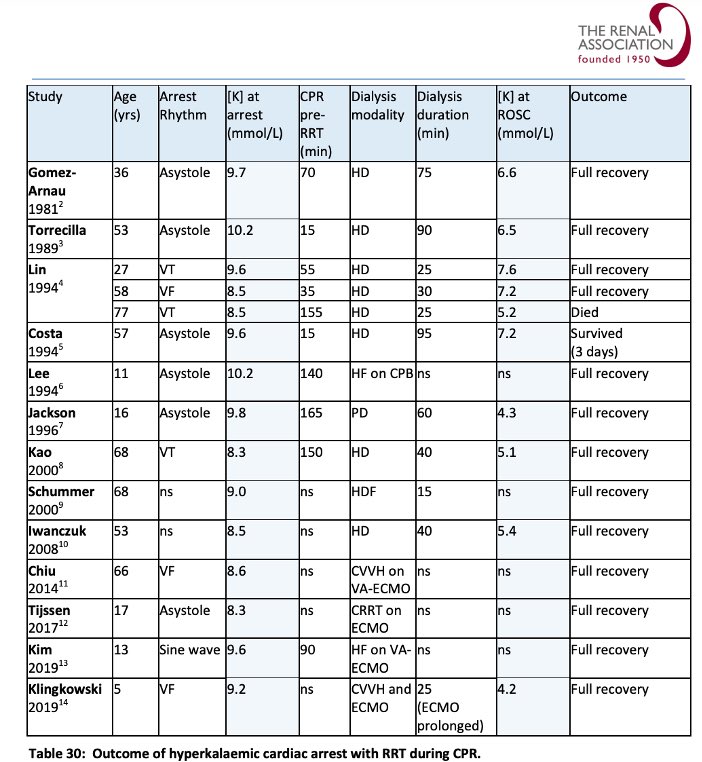
11/
Points from table:
✳️Mean K at arrest = 9.2, mean K at ROSC = 6.1
➡️ very hard to achieve this drop with drugs alone
✳️Mean dialysis time until ROSC = 50 mins
✳️Weak evidence that, even in extreme ⬆️K, outcomes can be good when dialysis used (in contrast to tweet 7 study)
Points from table:
✳️Mean K at arrest = 9.2, mean K at ROSC = 6.1
➡️ very hard to achieve this drop with drugs alone
✳️Mean dialysis time until ROSC = 50 mins
✳️Weak evidence that, even in extreme ⬆️K, outcomes can be good when dialysis used (in contrast to tweet 7 study)
12/
Hesitancy to start dialysis during CPR is inevitable, probably due to expectation of failure.
To quote Dr Annette Alfonzo (author UKKA guidelines) on the issue:
“like most things in life, you may not always succeed, but failure is usually guaranteed if you do not try”
Hesitancy to start dialysis during CPR is inevitable, probably due to expectation of failure.
To quote Dr Annette Alfonzo (author UKKA guidelines) on the issue:
“like most things in life, you may not always succeed, but failure is usually guaranteed if you do not try”
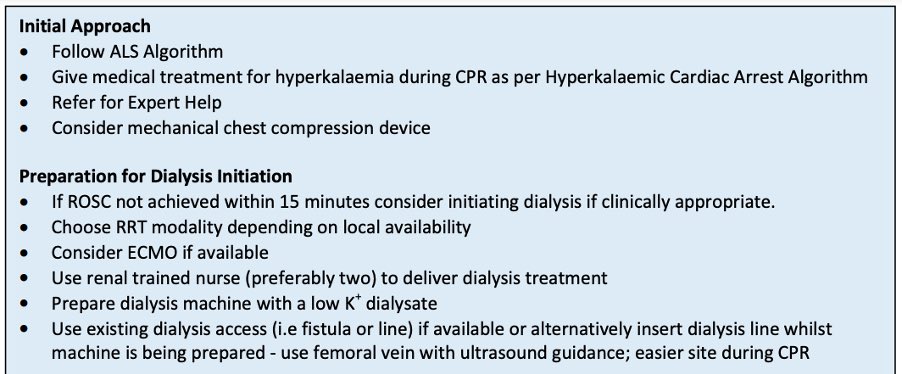
15/
What else?
✔️Consider ECMO
✔️Mechanical chest compression device if prolonged CPR
✔️Given often refractory to shocks until K controlled, some experts advocate to keep going until K normal (if appropriate)
✔️If get ROSC obviously ensure you clear K & monitor for rebound….
What else?
✔️Consider ECMO
✔️Mechanical chest compression device if prolonged CPR
✔️Given often refractory to shocks until K controlled, some experts advocate to keep going until K normal (if appropriate)
✔️If get ROSC obviously ensure you clear K & monitor for rebound….
16/
However, obviously prevention is better than cure…
I wrote a not great, non-exhaustive thread on some pitfalls of inpatient ⬆️K management a few years ago, though I suspect anyone making it this far will know plenty about this already (maybe not about the dried toad skin…)
However, obviously prevention is better than cure…
I wrote a not great, non-exhaustive thread on some pitfalls of inpatient ⬆️K management a few years ago, though I suspect anyone making it this far will know plenty about this already (maybe not about the dried toad skin…)
17/
Summary for ⬆️K cardiac arrest:
✅ Aggressive calcium
✅ Early adrenaline
✅ Insulin-dex bolus
✅ iv 8.4% bicarb
✅ Plan ahead for dialysis during CPR (+-ECMO) if appropriate & practical
✅ If you’re the renal reg on-call, go find out if your HD machines are defib-proof?
Summary for ⬆️K cardiac arrest:
✅ Aggressive calcium
✅ Early adrenaline
✅ Insulin-dex bolus
✅ iv 8.4% bicarb
✅ Plan ahead for dialysis during CPR (+-ECMO) if appropriate & practical
✅ If you’re the renal reg on-call, go find out if your HD machines are defib-proof?
Fin/
As ever, I’m a trainee mostly putting this together just to teach myself, so I welcome any tips/corrections from the more experienced.
The concept of HD during CPR sits uncomfortably with me, but better to mentally prepare in case a v rare scenario presents itself I suppose
As ever, I’m a trainee mostly putting this together just to teach myself, so I welcome any tips/corrections from the more experienced.
The concept of HD during CPR sits uncomfortably with me, but better to mentally prepare in case a v rare scenario presents itself I suppose
Fin 2/
The case was purely fictional.
ECG courtesy of Simmer, Wilde & ECGpedia.
For reference:
The fantastic 161 page UKKA hyperkalaemia guideline
ukkidney.org
European resus guideline “for special circumstances”
#secsect0030" target="_blank" rel="noopener" onclick="event.stopPropagation()">resuscitationjournal.com
The case was purely fictional.
ECG courtesy of Simmer, Wilde & ECGpedia.
For reference:
The fantastic 161 page UKKA hyperkalaemia guideline
ukkidney.org
European resus guideline “for special circumstances”
#secsect0030" target="_blank" rel="noopener" onclick="event.stopPropagation()">resuscitationjournal.com
Loading suggestions...