Next up in the #Tweetorial series based on my Hemodynamic Rounds Live lectures I’ll be discussing the basics of mechanical circulatory support (MCS) 📚
There is a lot of info to cover so this #Tweetorial will be broken up into four parts.
Follow along below for part 1. ⬇
There is a lot of info to cover so this #Tweetorial will be broken up into four parts.
Follow along below for part 1. ⬇
In this #Tweetorial I will go through the basics of LV function metrics – how do we measure them; how do we understand them & how do we apply them? 📊
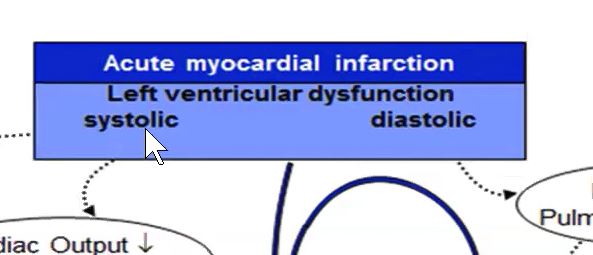
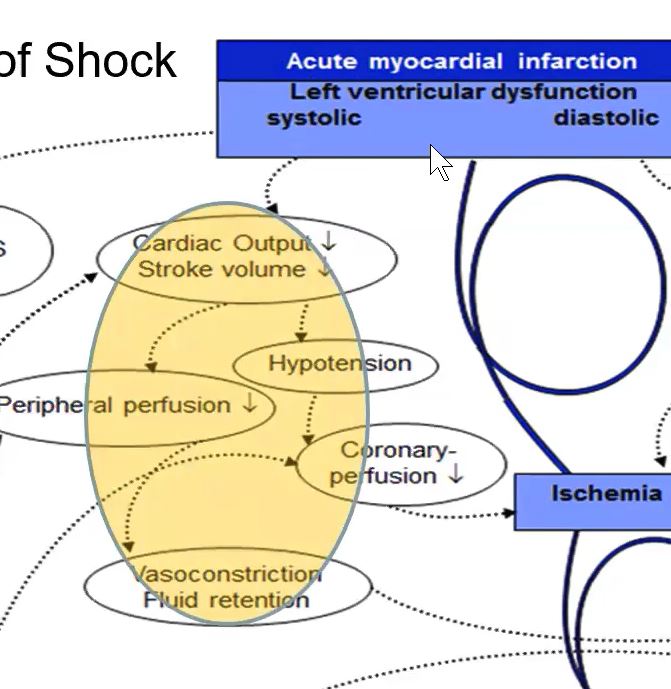
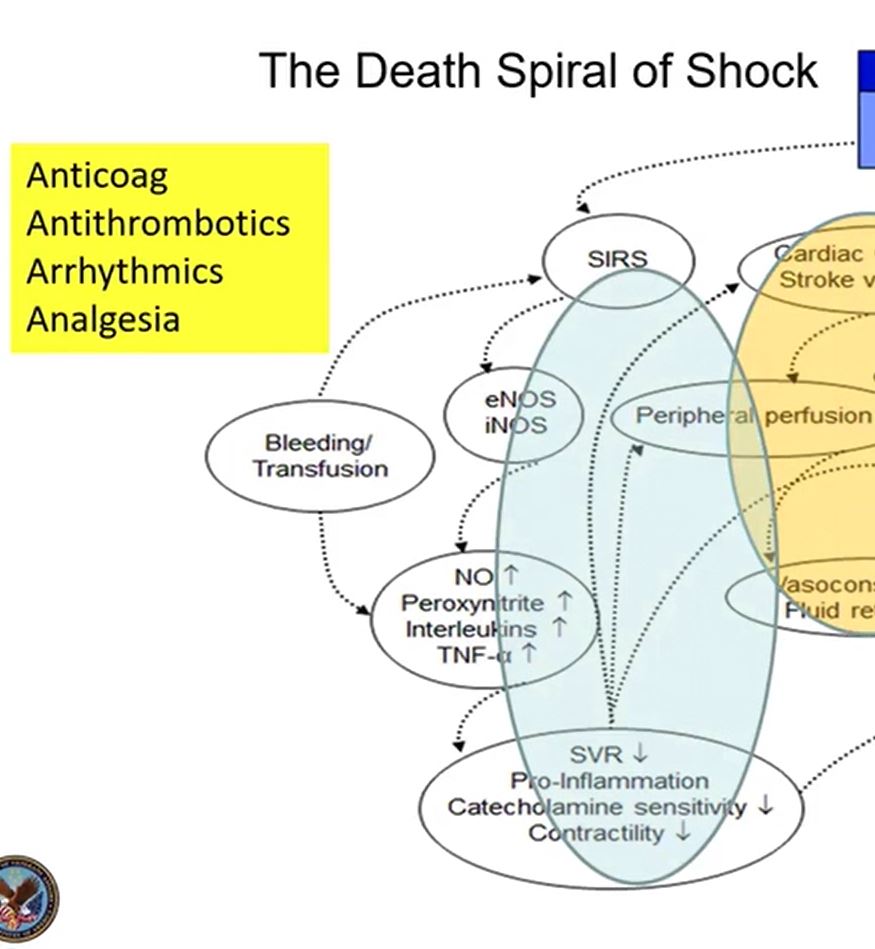
Then we will examine what each device is supposed to do for LV function & understand a couple of pathologic conditions.
Then we will examine what each device is supposed to do for LV function & understand a couple of pathologic conditions.
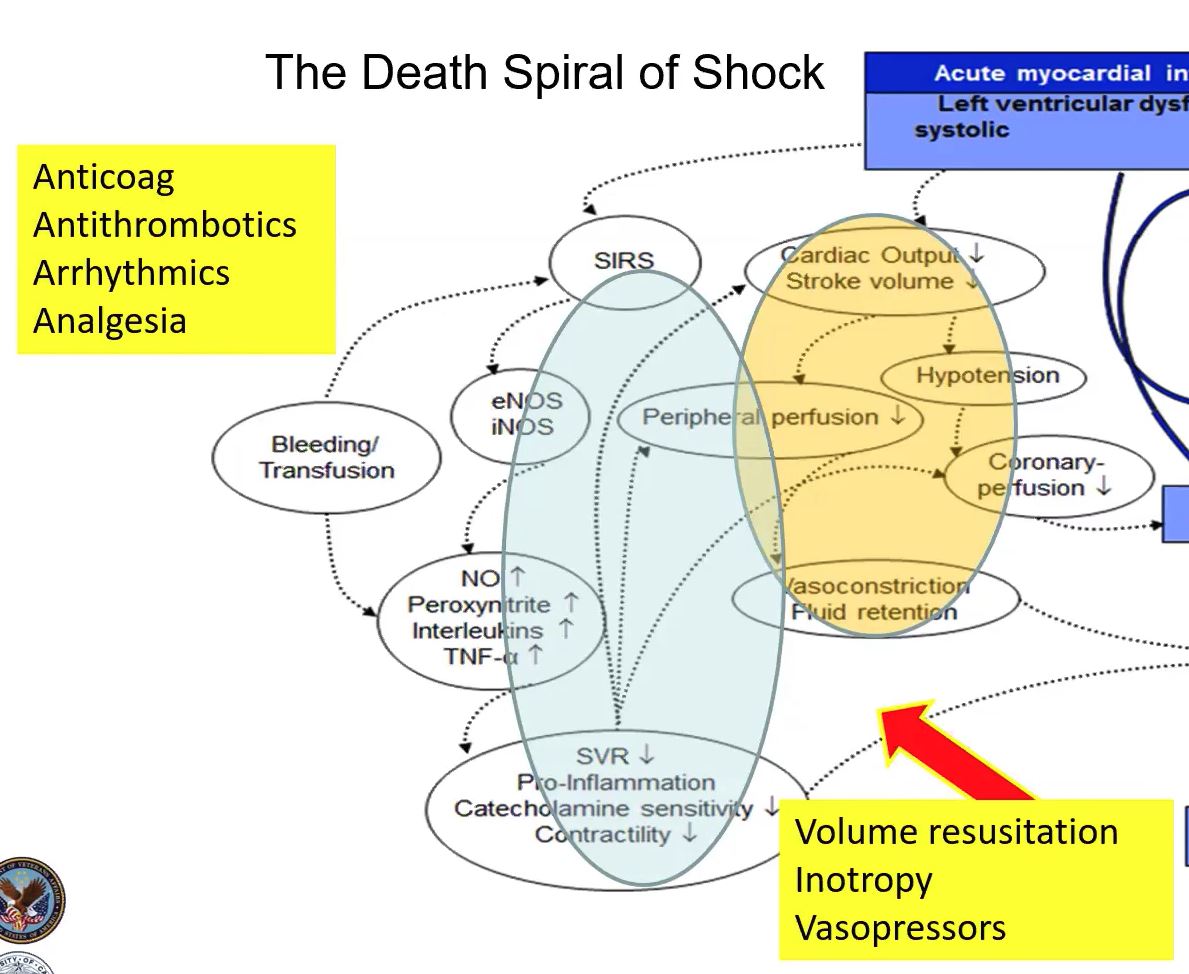
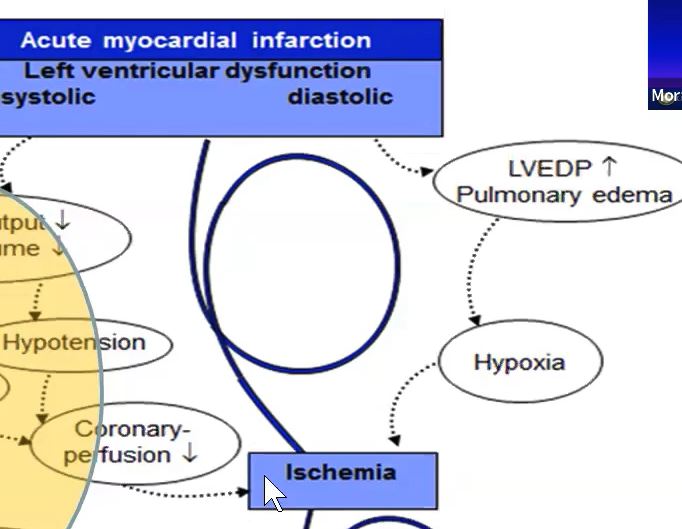
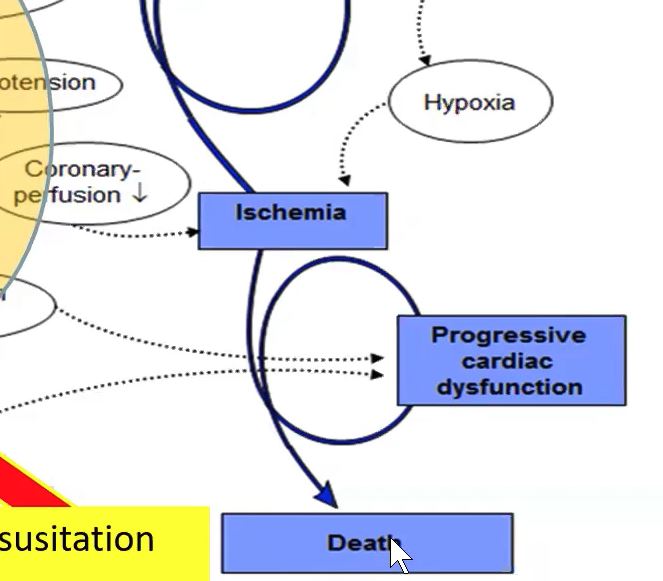
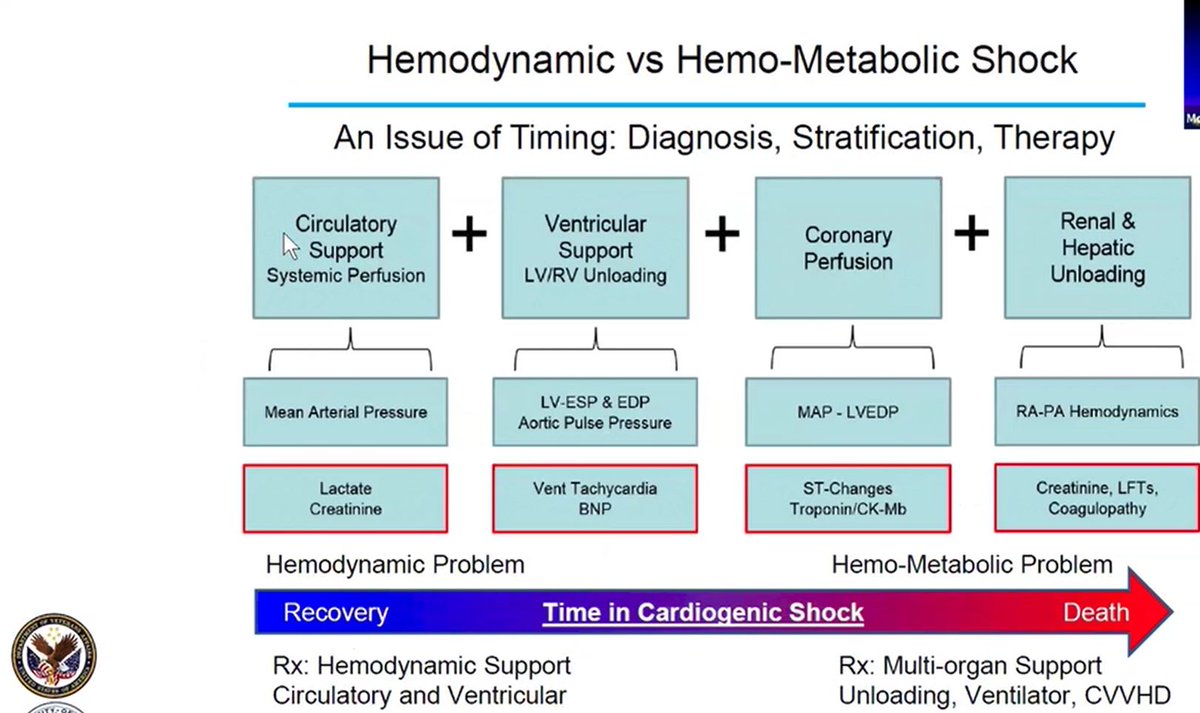
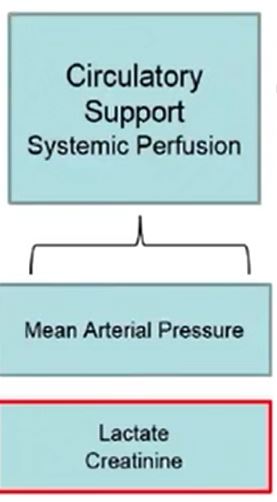
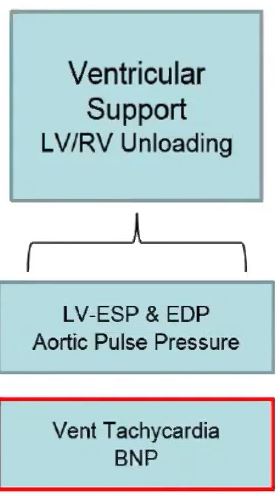
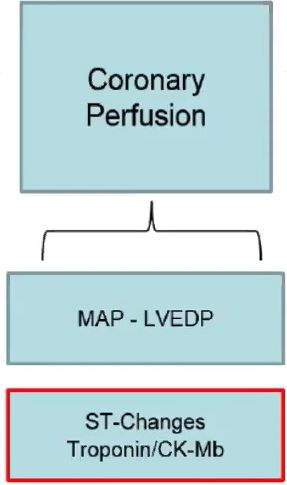
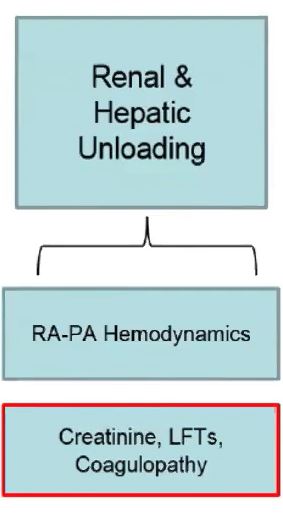
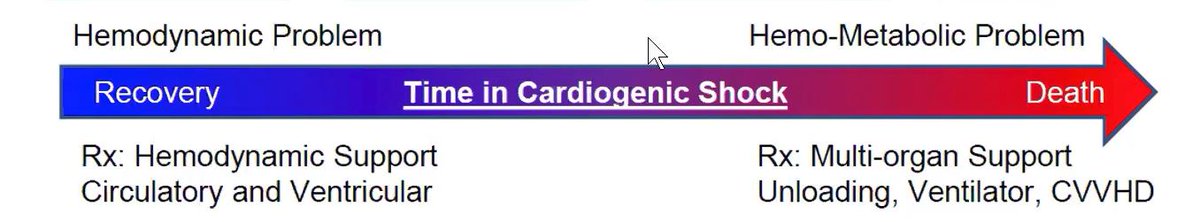
The hemodynamic syndrome of shock ⚡ evolves into a HemoMetabolic syndrome (a term coined by @NavinKapur4). If left unabated shock produces end organ damage and multisystem failure. 🤕
This concludes part 1 of this #Tweetorial on the Basics of MCS.
Stay tuned for part 2, when we will examine different device options.
Stay tuned for part 2, when we will examine different device options.
Loading suggestions...