10/12
We return to the patient’s hands. We see sclerodactyly, characterized by skin thickening and hardening, giving the skin a shiny appearance and leading to curling of the fingers with loss of mobility. There is also digital skin pitting and poorly healing ulcerations.
We return to the patient’s hands. We see sclerodactyly, characterized by skin thickening and hardening, giving the skin a shiny appearance and leading to curling of the fingers with loss of mobility. There is also digital skin pitting and poorly healing ulcerations.
12/12
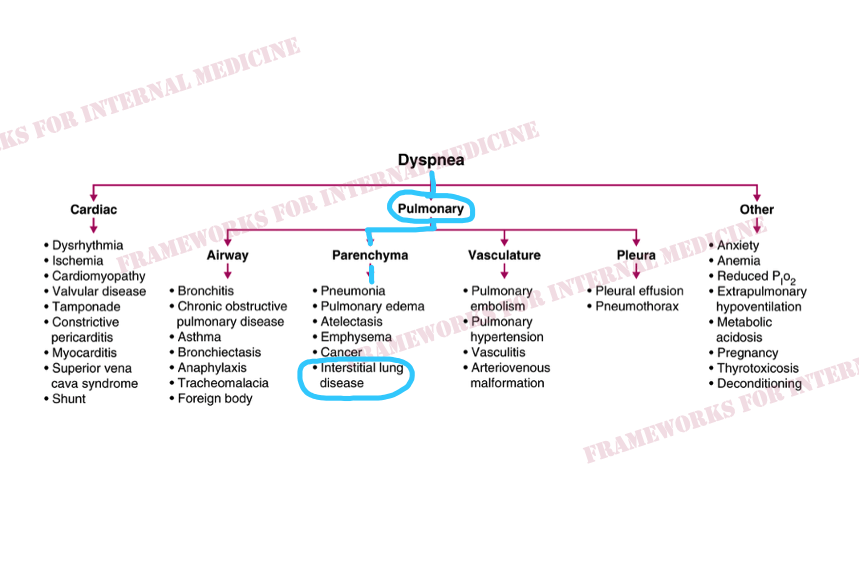
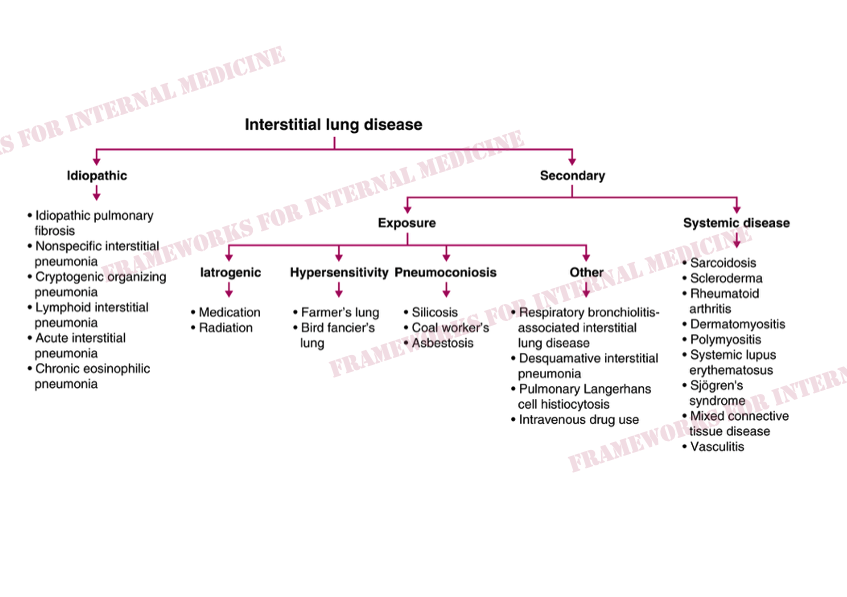
First we diagnosed interstitial lung disease, then we diagnosed underlying scleroderma. All with our eyes, ears, and a little help from hypothesis-driven testing.
For more frameworks: amazon.com
First we diagnosed interstitial lung disease, then we diagnosed underlying scleroderma. All with our eyes, ears, and a little help from hypothesis-driven testing.
For more frameworks: amazon.com
Loading suggestions...