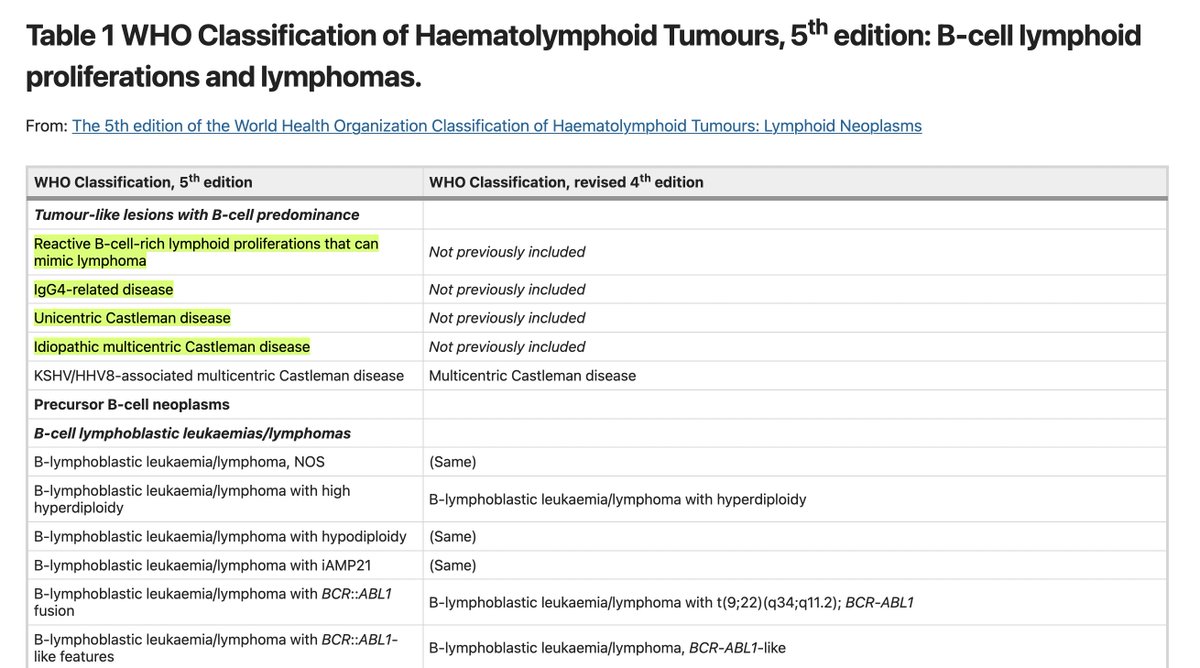
🔬 Previously, a lymphoid neoplasm of the marrow/blood = leukemia, solid lymph node (LN) neoplasm = lymphoma
🔬 However, many "lymphomas" can evolve into "leukemia," & vice-versa
🔬 Now, the WHO classifies lymphoid neoplasms based on cell of origin
🔬 However, many "lymphomas" can evolve into "leukemia," & vice-versa
🔬 Now, the WHO classifies lymphoid neoplasms based on cell of origin
5th Edition of the WHO's Classification of Haematolymphoid Tumours is available here:
nature.com
nature.com
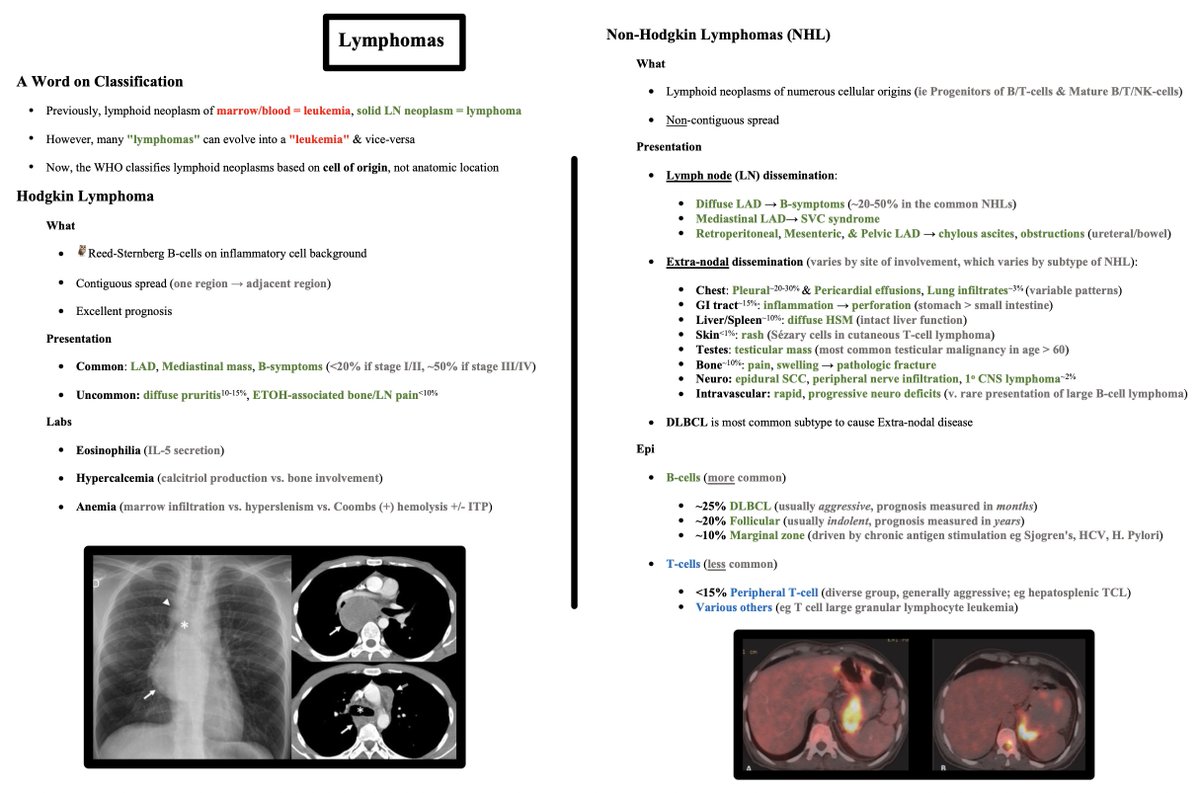
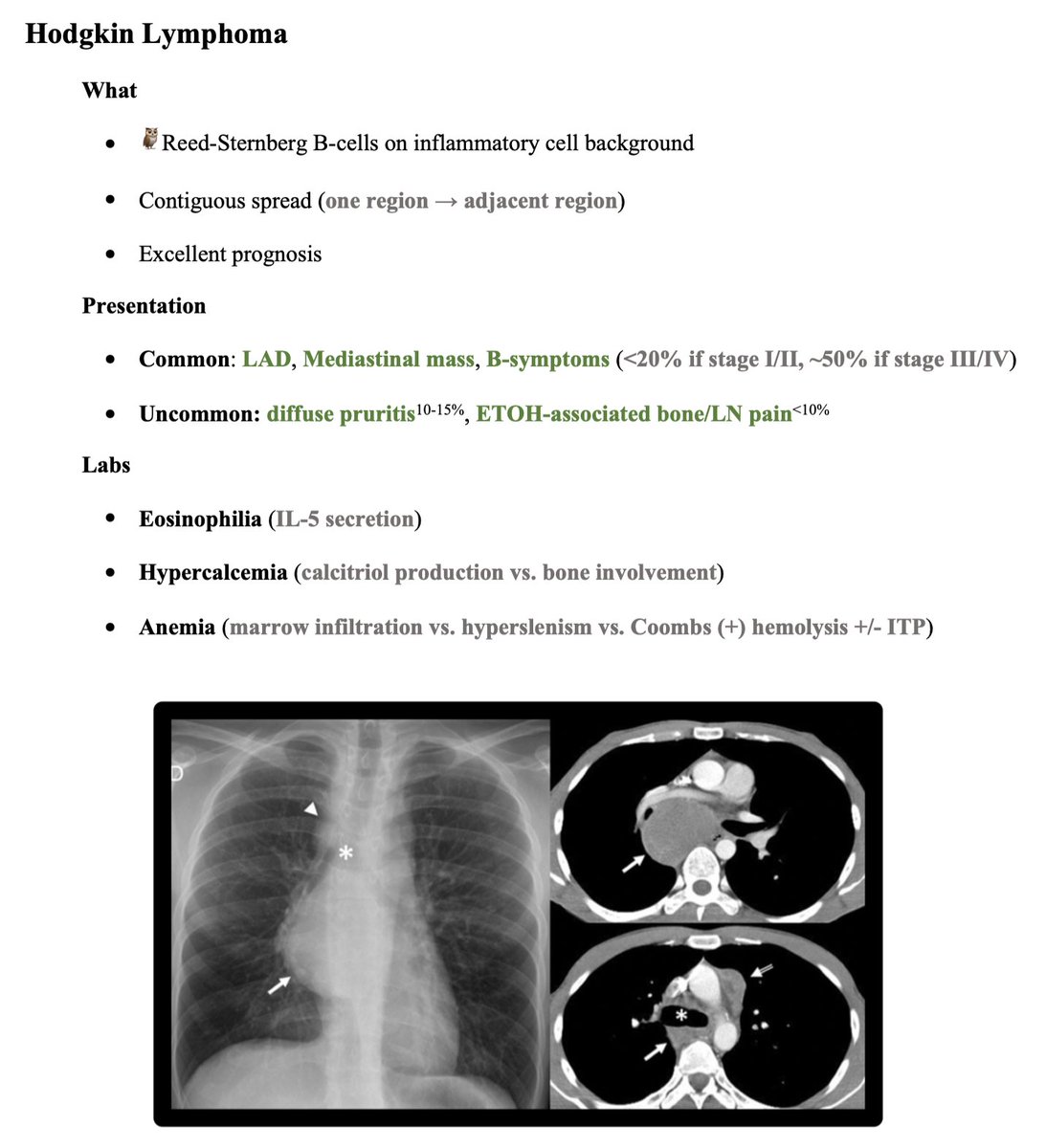
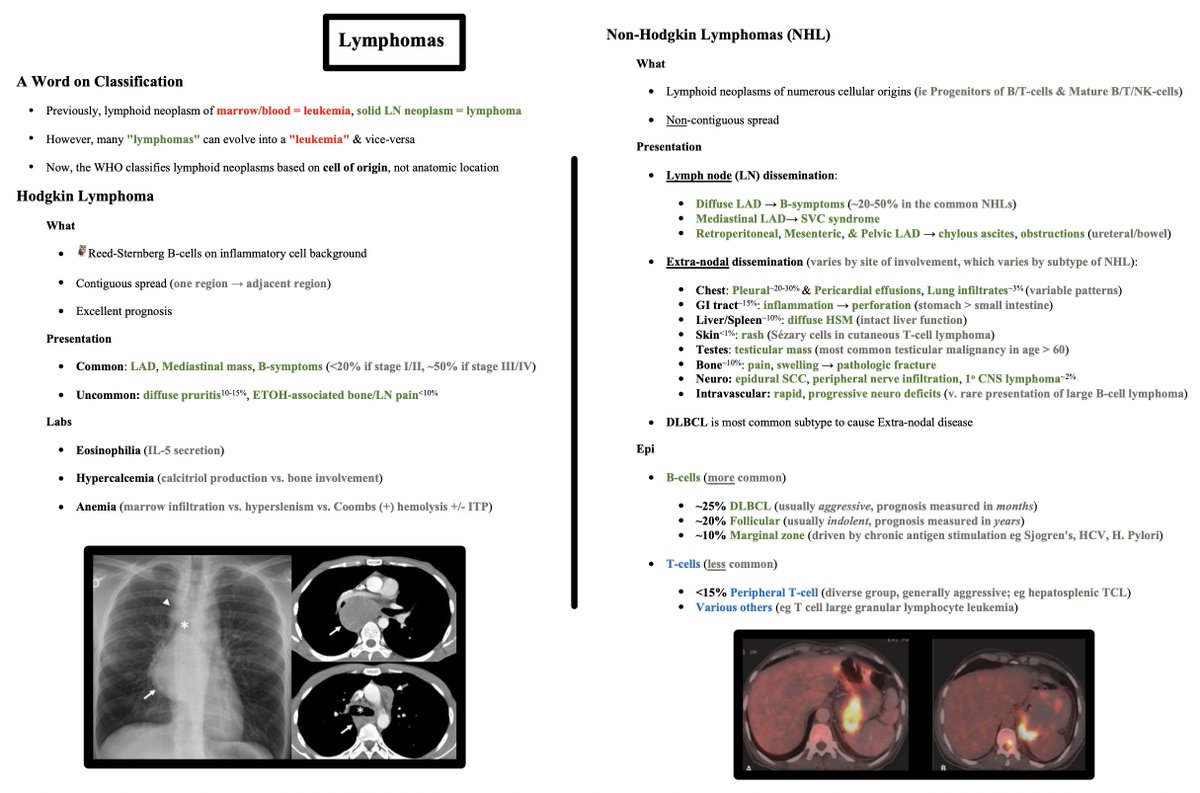
Hodgkin Lymphoma:
What?
🦉 Reed-Sternberg B-cells
🦉 Contiguous LN spread
🦉 Excellent prognosis
Presentation?
🦉 Common: LAD, Mediastinal mass, B-symptoms (<20% if stage I/II, ~50% if stage III/IV)
🦉 Uncommon: diffuse pruritis (10-15%), ETOH-associated bone/ LN pain (<10%)
What?
🦉 Reed-Sternberg B-cells
🦉 Contiguous LN spread
🦉 Excellent prognosis
Presentation?
🦉 Common: LAD, Mediastinal mass, B-symptoms (<20% if stage I/II, ~50% if stage III/IV)
🦉 Uncommon: diffuse pruritis (10-15%), ETOH-associated bone/ LN pain (<10%)
Non-Hodgkin Lymphomas (NHL) are where things always got confusing for me.
NHLs are confusing because they encompass neoplasms of numerous cellular origins, namely:
🦀 Progenitors of B/T-cells
🦀 Mature B/T/NK-cells
What do they have in common?
Non-contiguous spread
NHLs are confusing because they encompass neoplasms of numerous cellular origins, namely:
🦀 Progenitors of B/T-cells
🦀 Mature B/T/NK-cells
What do they have in common?
Non-contiguous spread
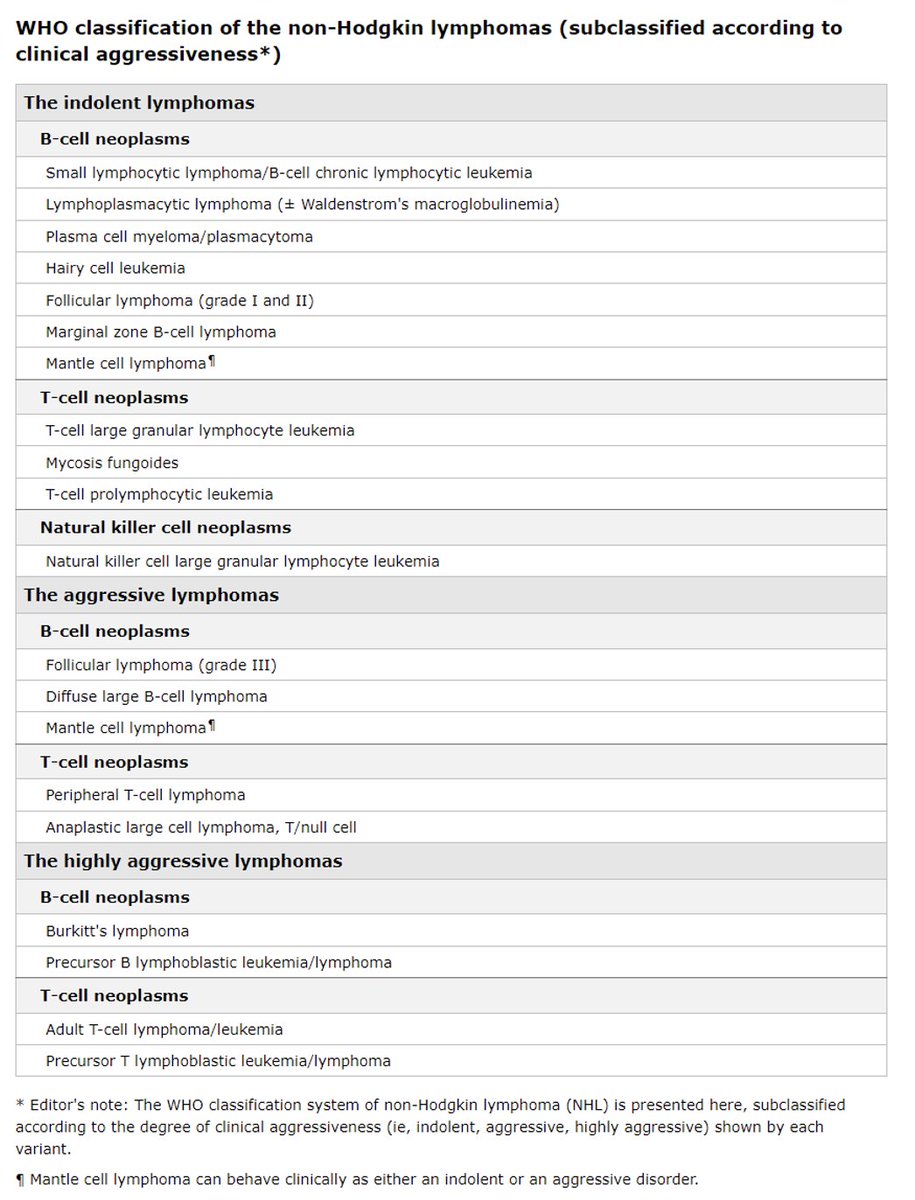
In a med school review of NHLs, this is when the lecturer would group the NHLs by degree of aggressiveness, PTLD vs. non-PTLD (@MatthewHoMD), or some other way.
Signs & symptoms can be broken down into those related to LN dissemination vs. Extra-nodal dissemination.
Extra-nodal signs & symptoms varies by site of involvement, which varies by subtype of NHL.
📚 Note: DLBCL is most common subtype to cause Extra-nodal disease.
Extra-nodal signs & symptoms varies by site of involvement, which varies by subtype of NHL.
📚 Note: DLBCL is most common subtype to cause Extra-nodal disease.
LN dissemination leads to:
🟢 Diffuse LAD → B-symptoms
🟢 Mediastinal LAD → SVC syndrome
🟢 Retroperitoneal, Mesenteric, & Pelvic LAD → chylous ascites, obstructions (ureteral, bowel)
🟢 Diffuse LAD → B-symptoms
🟢 Mediastinal LAD → SVC syndrome
🟢 Retroperitoneal, Mesenteric, & Pelvic LAD → chylous ascites, obstructions (ureteral, bowel)
Extra-nodal signs & symptoms:
🫁 Chest: pleural & pericardial effusions, lung infiltrates (variable patterns)
🤮 GI tract: inflammation → perforation (stomach > small intestine eg colitis)
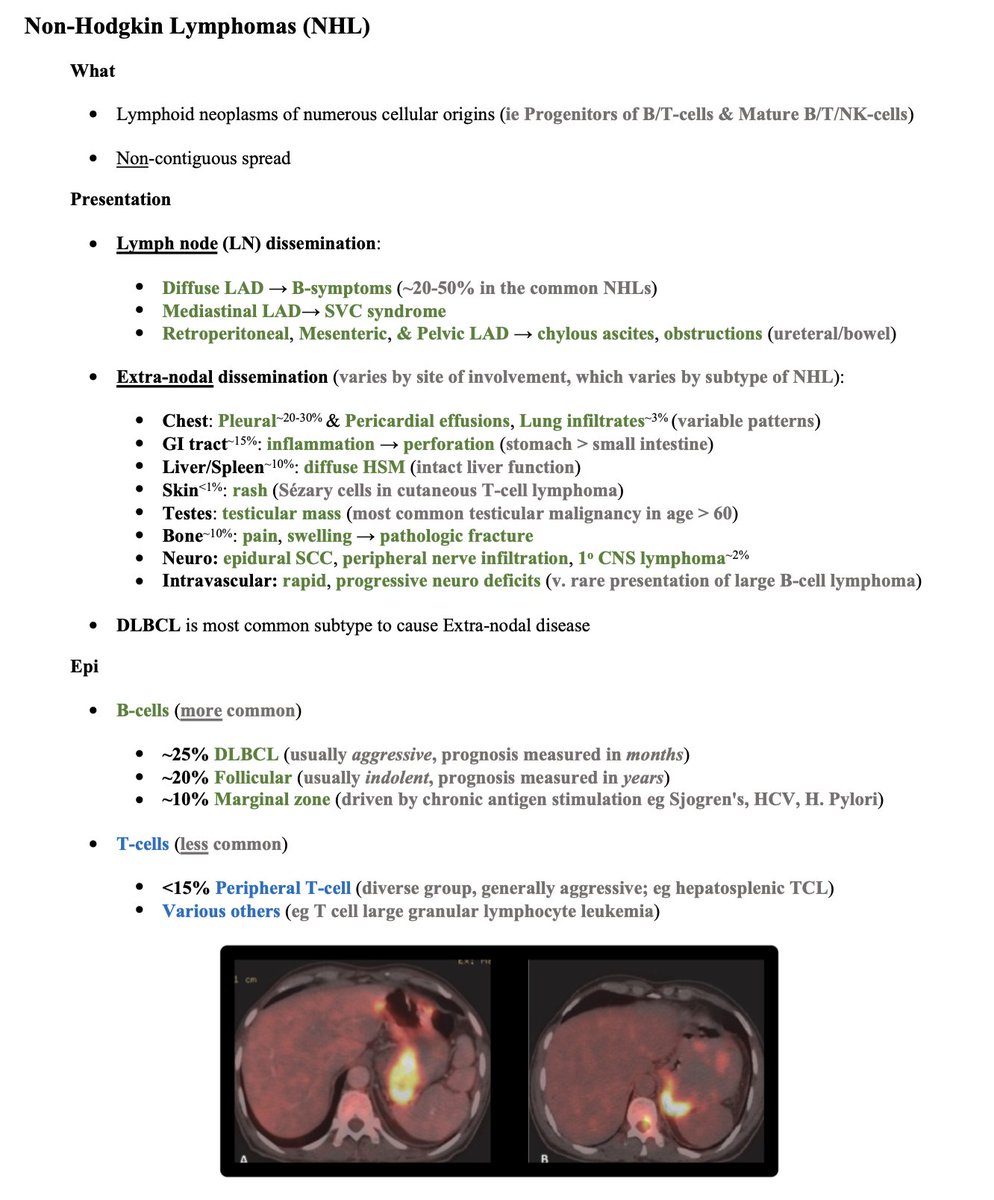
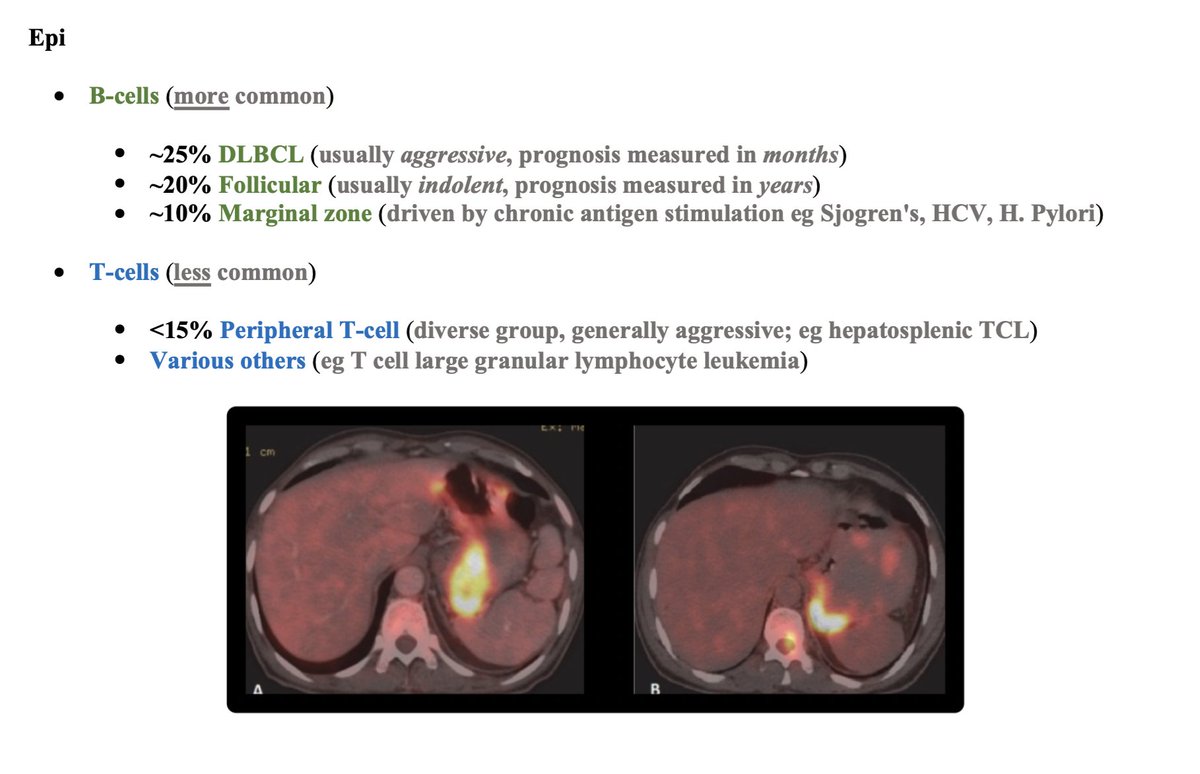
🟩 Liver/Spleen: diffuse hepatosplenomegaly (intact liver function)
🫁 Chest: pleural & pericardial effusions, lung infiltrates (variable patterns)
🤮 GI tract: inflammation → perforation (stomach > small intestine eg colitis)
🟩 Liver/Spleen: diffuse hepatosplenomegaly (intact liver function)
🧗 Skin: rash (Sezary cells in cutaneous T-cell lymphoma)
🍒 Testes: testicular mass (most common testicular malignancy in age > 60)
🦴 Bone: pain, swelling → pathologic fracture
🧠 Neuro: epidural SCC, peripheral nerve infiltration, primary CNS lymphoma
🍒 Testes: testicular mass (most common testicular malignancy in age > 60)
🦴 Bone: pain, swelling → pathologic fracture
🧠 Neuro: epidural SCC, peripheral nerve infiltration, primary CNS lymphoma
🩸 Intravascular: rapid, progressive neuro deficits (very rare presentation of large B-cell lymphoma)
🟢 B-cell subtypes = more common (~25% DLBCL, ~20% follicular, ~10% marginal)
🔵 T-cell subtypes = less common (<15% peripheral T cell, which is a diverse group of generally aggressive neoplasms)
🔵 T-cell subtypes = less common (<15% peripheral T cell, which is a diverse group of generally aggressive neoplasms)
References:
1) nature.com
2) ncbi.nlm.nih.gov
3) #H2" target="_blank" rel="noopener" onclick="event.stopPropagation()">uptodate.com
4) #H8" target="_blank" rel="noopener" onclick="event.stopPropagation()">uptodate.com
5) ashpublications.org
1) nature.com
2) ncbi.nlm.nih.gov
3) #H2" target="_blank" rel="noopener" onclick="event.stopPropagation()">uptodate.com
4) #H8" target="_blank" rel="noopener" onclick="event.stopPropagation()">uptodate.com
5) ashpublications.org
Review of SVC Syndrome here:
@CharlesMilrod
@CharlesMilrod
Loading suggestions...