1/ #CHEST2022 was fantastic! Here are some of my big take away points from this week’s sessions. @accpchest @VCU_PCCM @crit_caring_MD @lkbrath @DanckersMD @aggie07girl @DrMeganConroy @subanichandra
11/ There is an overestimation of arterial oxygenation saturation levels by pulse oximetry in patients of racial and ethnic minorities. It is important for healthcare providers to recognize this issue and to advocate for a solution. jamanetwork.com
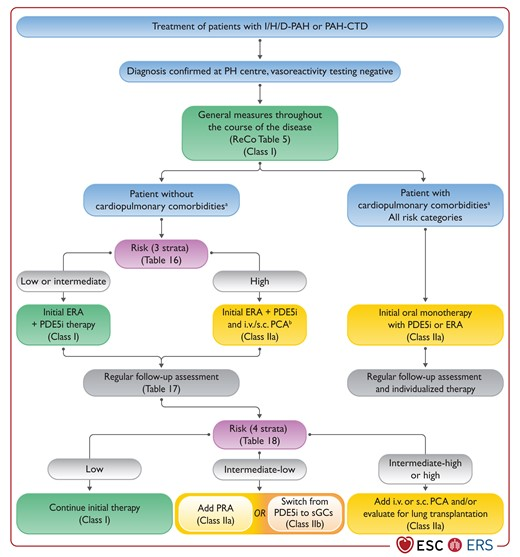
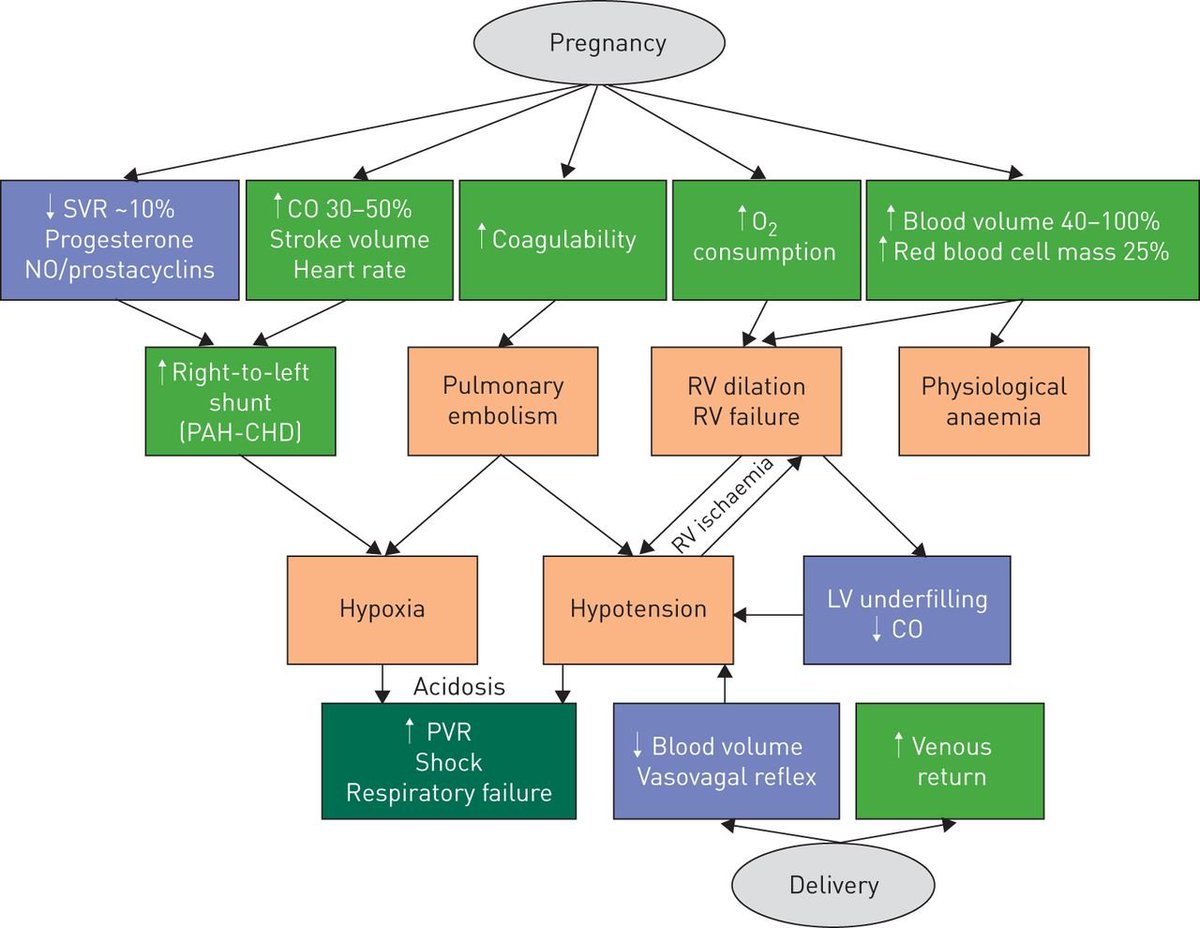
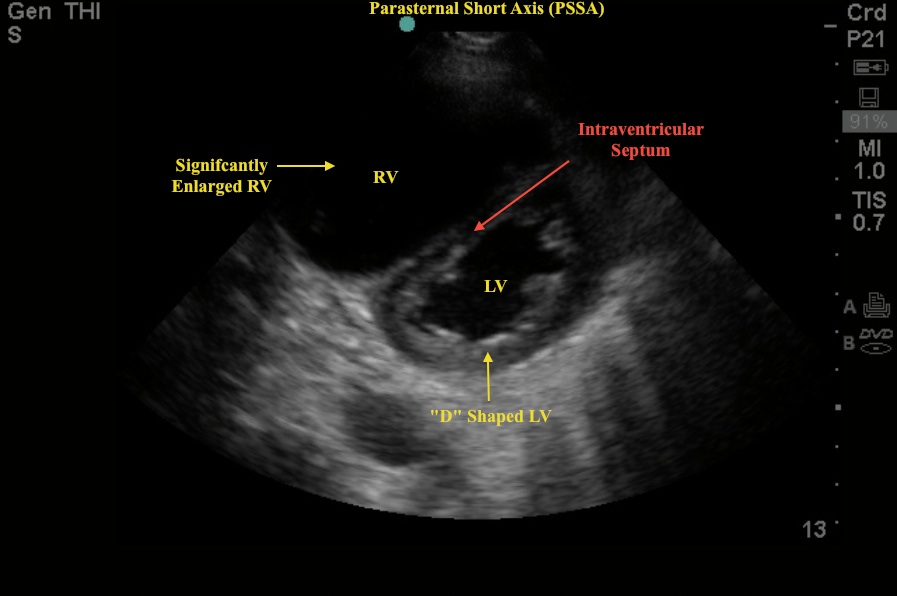
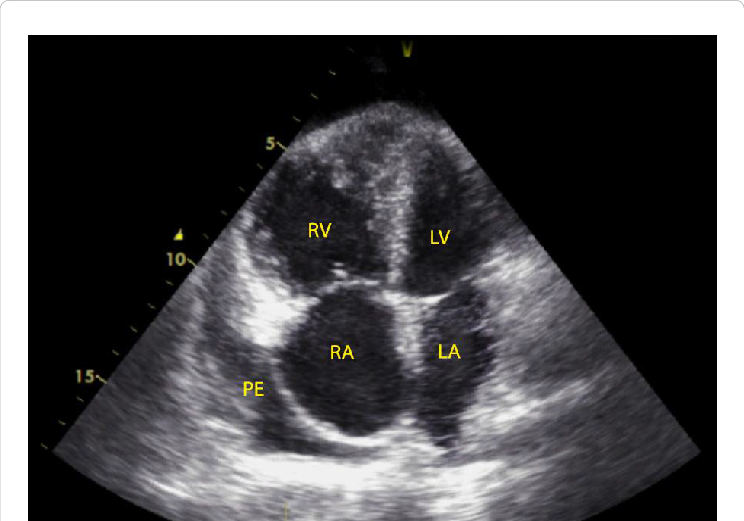
13/ Principles in the management of RV failure include the following:
1⃣Optimize Preload – DIURESE!
2⃣Reduce Afterload
3⃣Optimize Contractility
1⃣Optimize Preload – DIURESE!
2⃣Reduce Afterload
3⃣Optimize Contractility
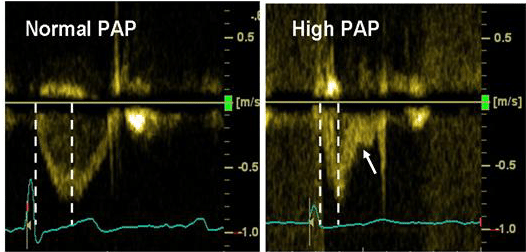
14/ Other good practice measures in management of RV failure:
1⃣Target SaO2 > 95% to avoid hypoxic pulmonary vasoconstriction
2⃣Avoid acidosis
3⃣Avoid dynamic hyperinflation in MV
4⃣Try to keep PEEP <10
5⃣May benefit from higher hemoglobin goal >10 g/dL
1⃣Target SaO2 > 95% to avoid hypoxic pulmonary vasoconstriction
2⃣Avoid acidosis
3⃣Avoid dynamic hyperinflation in MV
4⃣Try to keep PEEP <10
5⃣May benefit from higher hemoglobin goal >10 g/dL
Loading suggestions...