1/ Step 1 - Don’t
👉Shut anything off
👉Touch the vent
👉Remove restraints
👉Pause sedation
if you have not explicitly asked permission to do so.
[This is a survival thing! For the pt… (and you 😉)]
A #tweetorial @medtweetorial about critical care things for #neurologists
👉Shut anything off
👉Touch the vent
👉Remove restraints
👉Pause sedation
if you have not explicitly asked permission to do so.
[This is a survival thing! For the pt… (and you 😉)]
A #tweetorial @medtweetorial about critical care things for #neurologists
2/
Vibe check for the #neurologists out there. Do you like doing ICU consults?
#MedEd #NeuroTwitter #NeuroTwitterNetwork #EmoryNCCTweetorials
Vibe check for the #neurologists out there. Do you like doing ICU consults?
#MedEd #NeuroTwitter #NeuroTwitterNetwork #EmoryNCCTweetorials
4/
Tip 2⃣: many EDs are comfortable w/ peripheral pressors.
If an ischemic stroke patient drops their blood pressure & exam worsens in the ED: ask for pressor.
Don’t wait for a central line to start it.
Reasonable to target the BP they came in with or a 20% increase.
Tip 2⃣: many EDs are comfortable w/ peripheral pressors.
If an ischemic stroke patient drops their blood pressure & exam worsens in the ED: ask for pressor.
Don’t wait for a central line to start it.
Reasonable to target the BP they came in with or a 20% increase.
5/
Thinking:can that cause vasoconstriction of the cerebral arteries and maybe worsen CBF?
Is this dangerous?
Old (but a paper I love) suggests not: ahajournals.org
Small trial: pubmed.ncbi.nlm.nih.gov
Thinking:can that cause vasoconstriction of the cerebral arteries and maybe worsen CBF?
Is this dangerous?
Old (but a paper I love) suggests not: ahajournals.org
Small trial: pubmed.ncbi.nlm.nih.gov
6/
The 🗝️ here is that this only works for patients who would depend on collaterals. Often, these patients just need temporizing until they get a thrombectomy.
I get that this is trickier to do on floors.
So…HOB flat & bolus fluids?
⚠️There is not great evidence for this
The 🗝️ here is that this only works for patients who would depend on collaterals. Often, these patients just need temporizing until they get a thrombectomy.
I get that this is trickier to do on floors.
So…HOB flat & bolus fluids?
⚠️There is not great evidence for this
7/
*Some* patients may augment CBF with a flat trial: pubmed.ncbi.nlm.nih.gov
But, there is an aspiration risk.
Trial has some flaws, I think it is convincing enough that we should *not* routinely lay patients flat “just because” that’s a protocol:
pubmed.ncbi.nlm.nih.gov
*Some* patients may augment CBF with a flat trial: pubmed.ncbi.nlm.nih.gov
But, there is an aspiration risk.
Trial has some flaws, I think it is convincing enough that we should *not* routinely lay patients flat “just because” that’s a protocol:
pubmed.ncbi.nlm.nih.gov
8/
Bolus then? Interestingly, some lit suggest that the hemodynamic effect of a fluid bolus may be due to the temperature❄️!
From @pulmcrit 🙏about how blousing fluids is not the solution to all hemodynamic problems: emcrit.org
Cooling blanket anyone? 🤔🤷♀️
Bolus then? Interestingly, some lit suggest that the hemodynamic effect of a fluid bolus may be due to the temperature❄️!
From @pulmcrit 🙏about how blousing fluids is not the solution to all hemodynamic problems: emcrit.org
Cooling blanket anyone? 🤔🤷♀️
9/
That said all, there may be pts that do respond to fluid challenge so it’s not an unreasonable thing to try.
What is unreasonable? “Maintenance fluids”
Tip 3⃣: Maintenance fluids can have all kinds of deleterious side effects!
@neuro_intensive begs you to
That said all, there may be pts that do respond to fluid challenge so it’s not an unreasonable thing to try.
What is unreasonable? “Maintenance fluids”
Tip 3⃣: Maintenance fluids can have all kinds of deleterious side effects!
@neuro_intensive begs you to
10/
Quick summary of hemodynamic tips:
🗣️Communicate BP goals
💉Pressors are a more reliable way to achieve a hemodynamic target than fluids & HOB: ie perfusion dependent pts deserve a unit bed and very close monitoring!
🛑Stop maintenance fluids 🙏
Quick summary of hemodynamic tips:
🗣️Communicate BP goals
💉Pressors are a more reliable way to achieve a hemodynamic target than fluids & HOB: ie perfusion dependent pts deserve a unit bed and very close monitoring!
🛑Stop maintenance fluids 🙏
11/
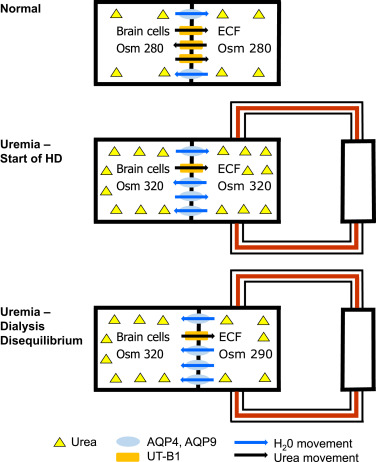
Tip 4⃣: Hemodialysis can kill people with brain pathology ! ☠️
Hemodialysis causes fluid shift (check out @ericlawso and thus can cause cerebral edema.
w/ an ICP problem this can be enough to result in herniation 😱 pubmed.ncbi.nlm.nih.gov
Tip 4⃣: Hemodialysis can kill people with brain pathology ! ☠️
Hemodialysis causes fluid shift (check out @ericlawso and thus can cause cerebral edema.
w/ an ICP problem this can be enough to result in herniation 😱 pubmed.ncbi.nlm.nih.gov
13/
Tip 5⃣: If you do get into an ICP crisis issue, a 3% infusion is not the solution🙏
Hyperosmolar therapy works by rapidly “dehydrating” the brain.
This depends on the fast creation of a gradient. An infusion will not create said gradient.
More: emcrit.org
Tip 5⃣: If you do get into an ICP crisis issue, a 3% infusion is not the solution🙏
Hyperosmolar therapy works by rapidly “dehydrating” the brain.
This depends on the fast creation of a gradient. An infusion will not create said gradient.
More: emcrit.org
14/
Mannitol can go through a filtered peripheral IV. New evidence that 23% HTS can too. If you want to use 3%, give as a bolus (250cc). You can even use code-cart hypertonic bicarb!
Whatever the solution, the goal is the rapid creation of a gradient.
Mannitol can go through a filtered peripheral IV. New evidence that 23% HTS can too. If you want to use 3%, give as a bolus (250cc). You can even use code-cart hypertonic bicarb!
Whatever the solution, the goal is the rapid creation of a gradient.
15/
Tip 6⃣: PLEX and CRRT are not mutually exclusive. If a patient needs CRRT but also needs PLEX, have a conversation with the critical care team about when it’s appropriate to alternate in the PLEX.
Or use a different induction immunotherapy if it’s a ½ dozen or the other.
Tip 6⃣: PLEX and CRRT are not mutually exclusive. If a patient needs CRRT but also needs PLEX, have a conversation with the critical care team about when it’s appropriate to alternate in the PLEX.
Or use a different induction immunotherapy if it’s a ½ dozen or the other.
16/
Bonus PLEX can be run through a peripheral line! Ask your PLEX team.
More about my love of PLEX here:
emcrit.org
Bonus PLEX can be run through a peripheral line! Ask your PLEX team.
More about my love of PLEX here:
emcrit.org
19/
Tip 9⃣: Weaning infusions:
It’s a pain to titrate down a small amount every hour.
Unless this is a very delicate patient, pick a more moderate dose change and adjust every 4-6 hours
(ie. asking to go down on Midazolam by 1mg q1hour creates extra work; consider 4q4)
Tip 9⃣: Weaning infusions:
It’s a pain to titrate down a small amount every hour.
Unless this is a very delicate patient, pick a more moderate dose change and adjust every 4-6 hours
(ie. asking to go down on Midazolam by 1mg q1hour creates extra work; consider 4q4)
21/
Tip 🔟: The ICU is probably more comfortable with ketamine than most neurologists are. This is a great drug for refractory status!
Mostly well tolerated although can lead to metabolic acidosis & hemodynamic instability w/ prolonged, high dose use (+sometimes lots of saliva)
Tip 🔟: The ICU is probably more comfortable with ketamine than most neurologists are. This is a great drug for refractory status!
Mostly well tolerated although can lead to metabolic acidosis & hemodynamic instability w/ prolonged, high dose use (+sometimes lots of saliva)
Thank you to @CajalButterfly @sigman_md and @feras_akbik who chipped in tips and peer reviewed! 🙏 love to hear other tips that people find helpful!😄 @namorrismd @drdangayach @aartisarwal @rkchoi @MicieliA_MD @a_charidimou @andrewyu8 @ShadiYaghi2 @SubinMatthews @bobvarkey
Oops @MedTweetorials didn’t link you in the first tweet cause I forgot the s… 🤦♀️
Loading suggestions...