1/15
🤔Why do antibiotics reduce the risk of rebleeding after acute variceal hemorrhage?
I understand why antibiotics reduce infections, but the mechanism by which they reduce rebleeding is not immediately apparent.
Let's have a look.
🤔Why do antibiotics reduce the risk of rebleeding after acute variceal hemorrhage?
I understand why antibiotics reduce infections, but the mechanism by which they reduce rebleeding is not immediately apparent.
Let's have a look.
2/
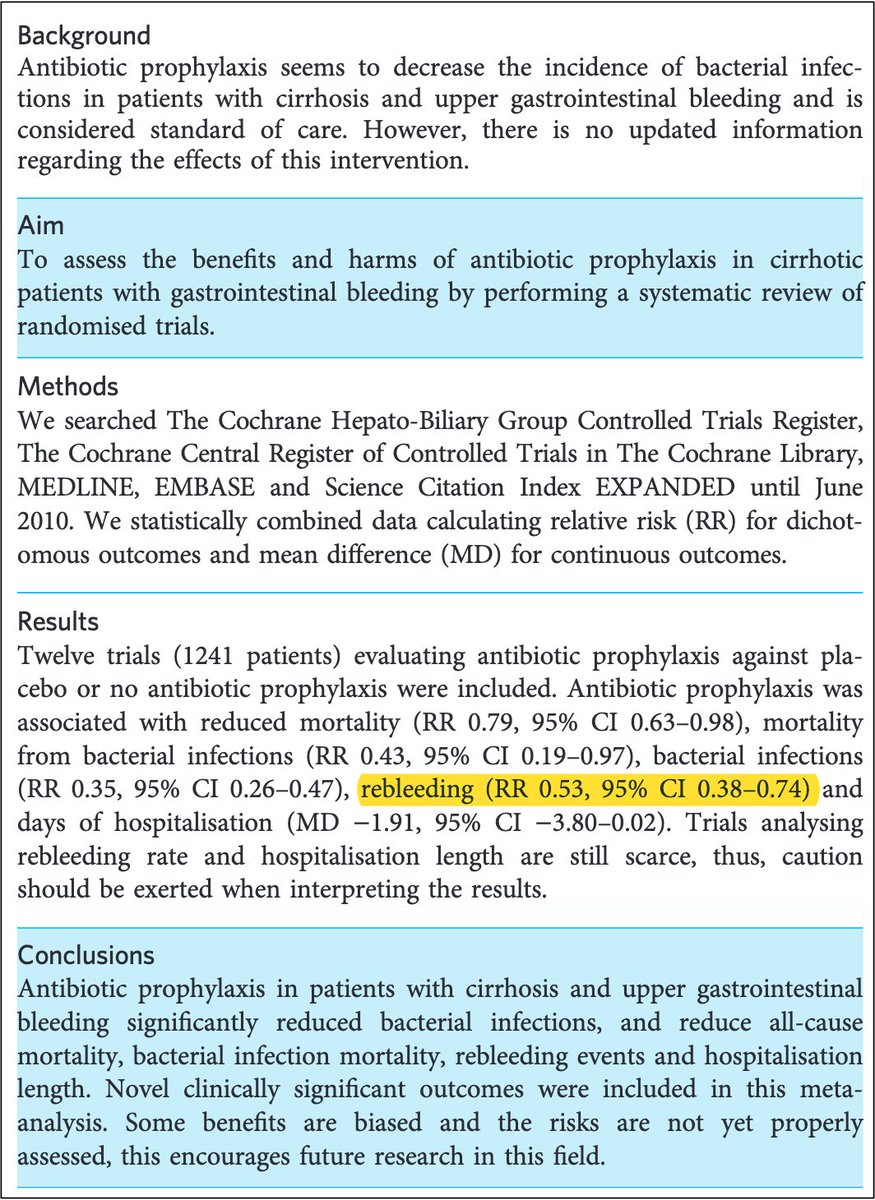
First, let's confirm that antibiotics DO decrease the risk of rebleeding after acute variceal hemorrhage.
A 2011 meta-analysis found that prophylactic antibiotics reduce the following:
➤Rebleeding episodes: RR 0.53
➤Rebleeding at 7 days: RR 0.24
pubmed.ncbi.nlm.nih.gov
First, let's confirm that antibiotics DO decrease the risk of rebleeding after acute variceal hemorrhage.
A 2011 meta-analysis found that prophylactic antibiotics reduce the following:
➤Rebleeding episodes: RR 0.53
➤Rebleeding at 7 days: RR 0.24
pubmed.ncbi.nlm.nih.gov
3/
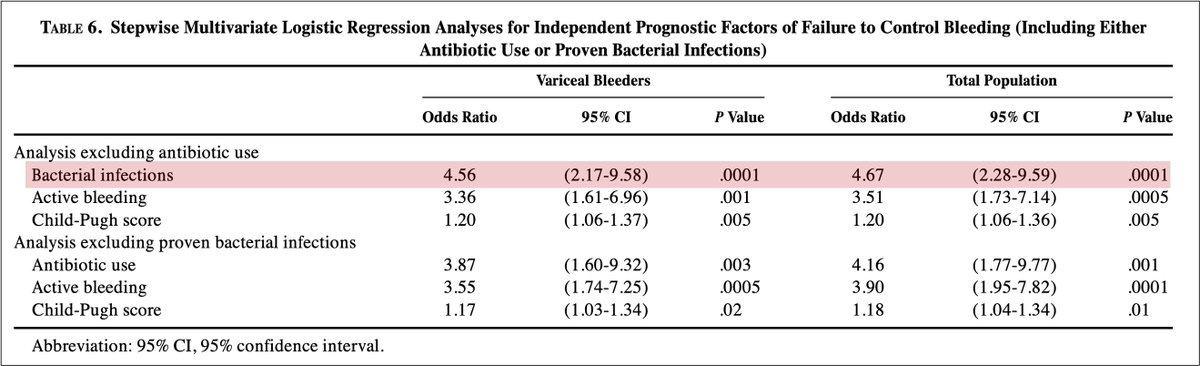
To understand why antibiotics affect bleeding, it is important to recognize that bacterial infections are independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal bleeding.
pubmed.ncbi.nlm.nih.gov
To understand why antibiotics affect bleeding, it is important to recognize that bacterial infections are independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal bleeding.
pubmed.ncbi.nlm.nih.gov
4/
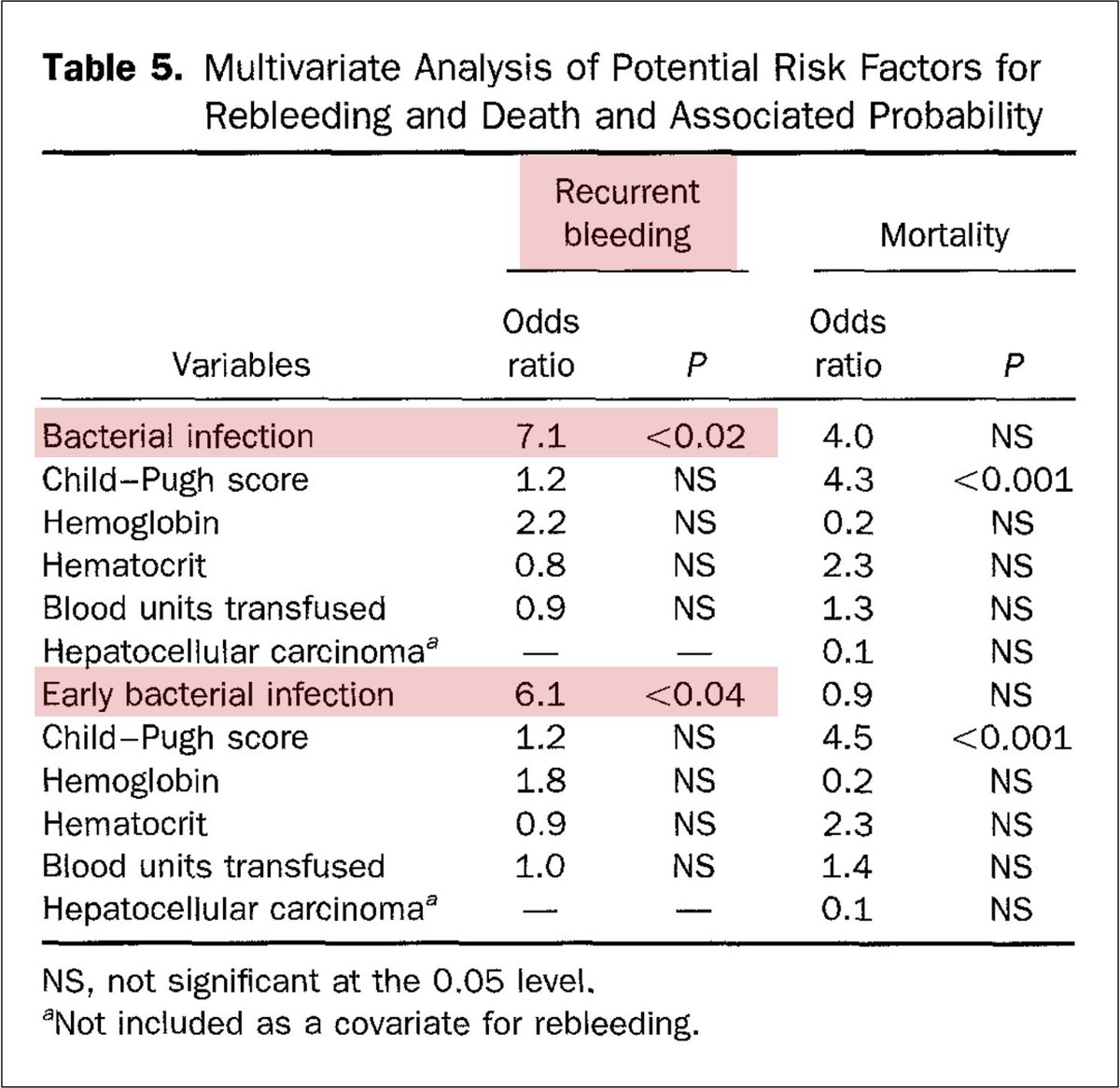
Another study found bacterial infections were associated with more early rebleeding:
💥44% vs. 10% without infection💥
And on a multivariate analysis, ONLY bacterial infections predicted early rebleeding.
pubmed.ncbi.nlm.nih.gov
Another study found bacterial infections were associated with more early rebleeding:
💥44% vs. 10% without infection💥
And on a multivariate analysis, ONLY bacterial infections predicted early rebleeding.
pubmed.ncbi.nlm.nih.gov
5/
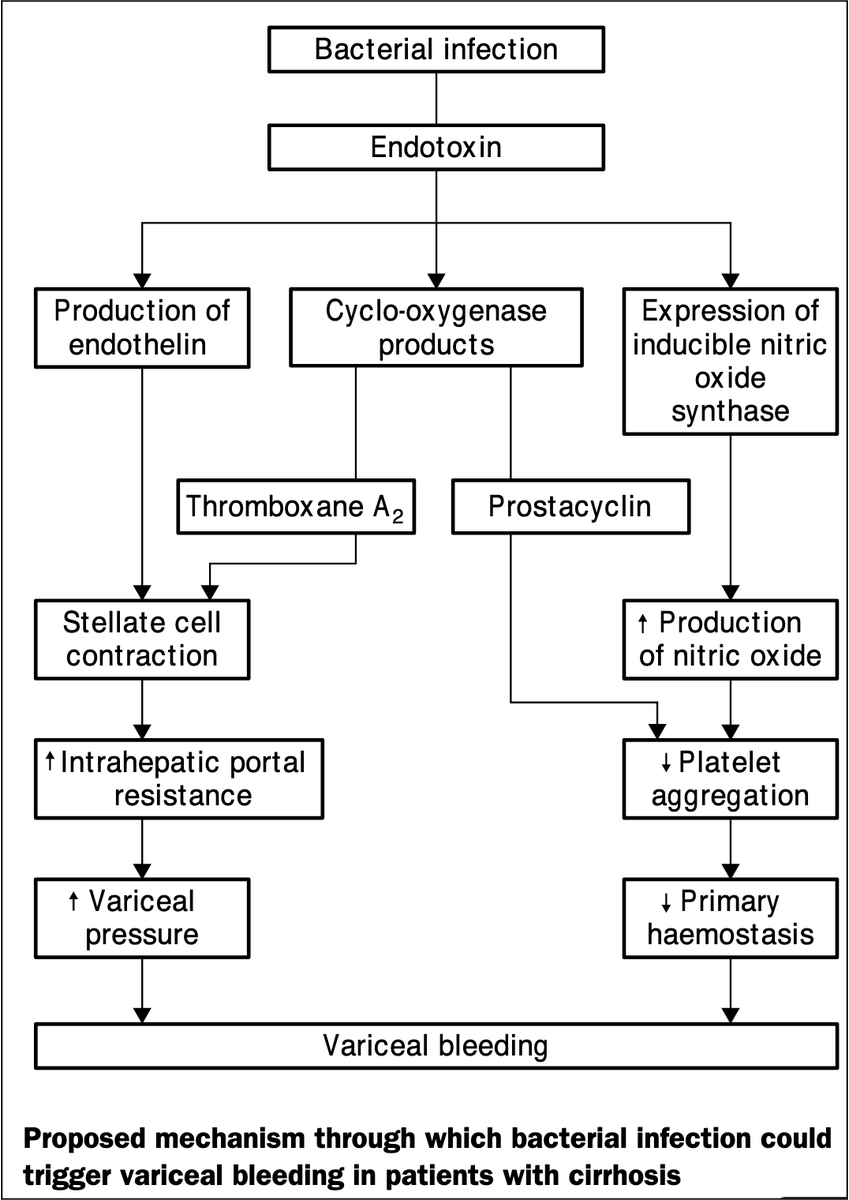
So, bacterial infections are associated with rebleeding, and antibiotic prophylaxis reduces the rates of rebleeding.
At least three factors explain this:
↑Heparin effect
↑Endothelin-1
↓Platelet function
ncbi.nlm.nih.gov
So, bacterial infections are associated with rebleeding, and antibiotic prophylaxis reduces the rates of rebleeding.
At least three factors explain this:
↑Heparin effect
↑Endothelin-1
↓Platelet function
ncbi.nlm.nih.gov
6/
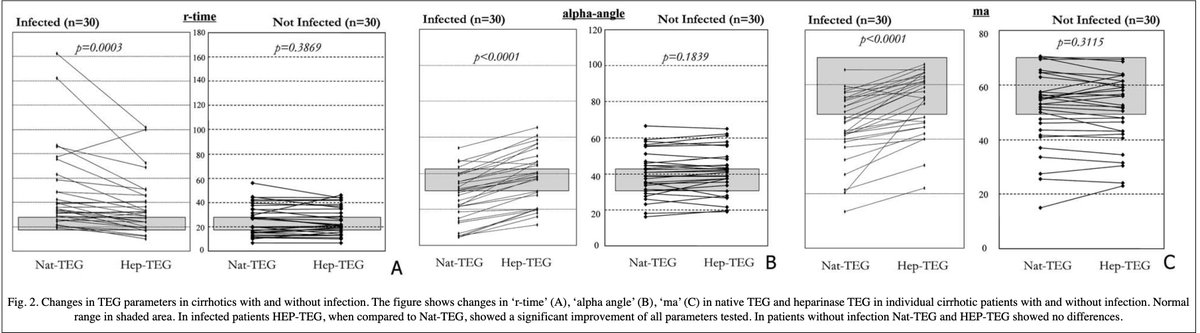
One study found a significant heparin effect in:
➤28/30 with cirrhotics AND infection
➤0/30 with cirrhosis but no infection
➤0/5 with infection but no cirrhosis
The heparin effect completely reversed after the resolution of the infection.
pubmed.ncbi.nlm.nih.gov
One study found a significant heparin effect in:
➤28/30 with cirrhotics AND infection
➤0/30 with cirrhosis but no infection
➤0/5 with infection but no cirrhosis
The heparin effect completely reversed after the resolution of the infection.
pubmed.ncbi.nlm.nih.gov
7/
The increased heparin effect seen in bacterial infection might be due to one or both of the following:
☞Endothelial injury and heparin release
☞Mast cell activation and heparin release
ncbi.nlm.nih.gov
The increased heparin effect seen in bacterial infection might be due to one or both of the following:
☞Endothelial injury and heparin release
☞Mast cell activation and heparin release
ncbi.nlm.nih.gov
8/
But there's more!
Heparin is cleared by the liver. As a result, the half-life of heparin is longer in those with cirrhosis compared to controls.
➤118 minutes in those with cirrhosis and normal renal function
➤74 minutes in controls
pubmed.ncbi.nlm.nih.gov
But there's more!
Heparin is cleared by the liver. As a result, the half-life of heparin is longer in those with cirrhosis compared to controls.
➤118 minutes in those with cirrhosis and normal renal function
➤74 minutes in controls
pubmed.ncbi.nlm.nih.gov
9/
The above studies suggest that in those with cirrhosis, bacterial infections result in an increased release of heparinoids. Once released, they stick around for longer periods of time.
This may contribute to the increased risk of rebleeding.
Let's look at endothelin-1 next.
The above studies suggest that in those with cirrhosis, bacterial infections result in an increased release of heparinoids. Once released, they stick around for longer periods of time.
This may contribute to the increased risk of rebleeding.
Let's look at endothelin-1 next.
10/
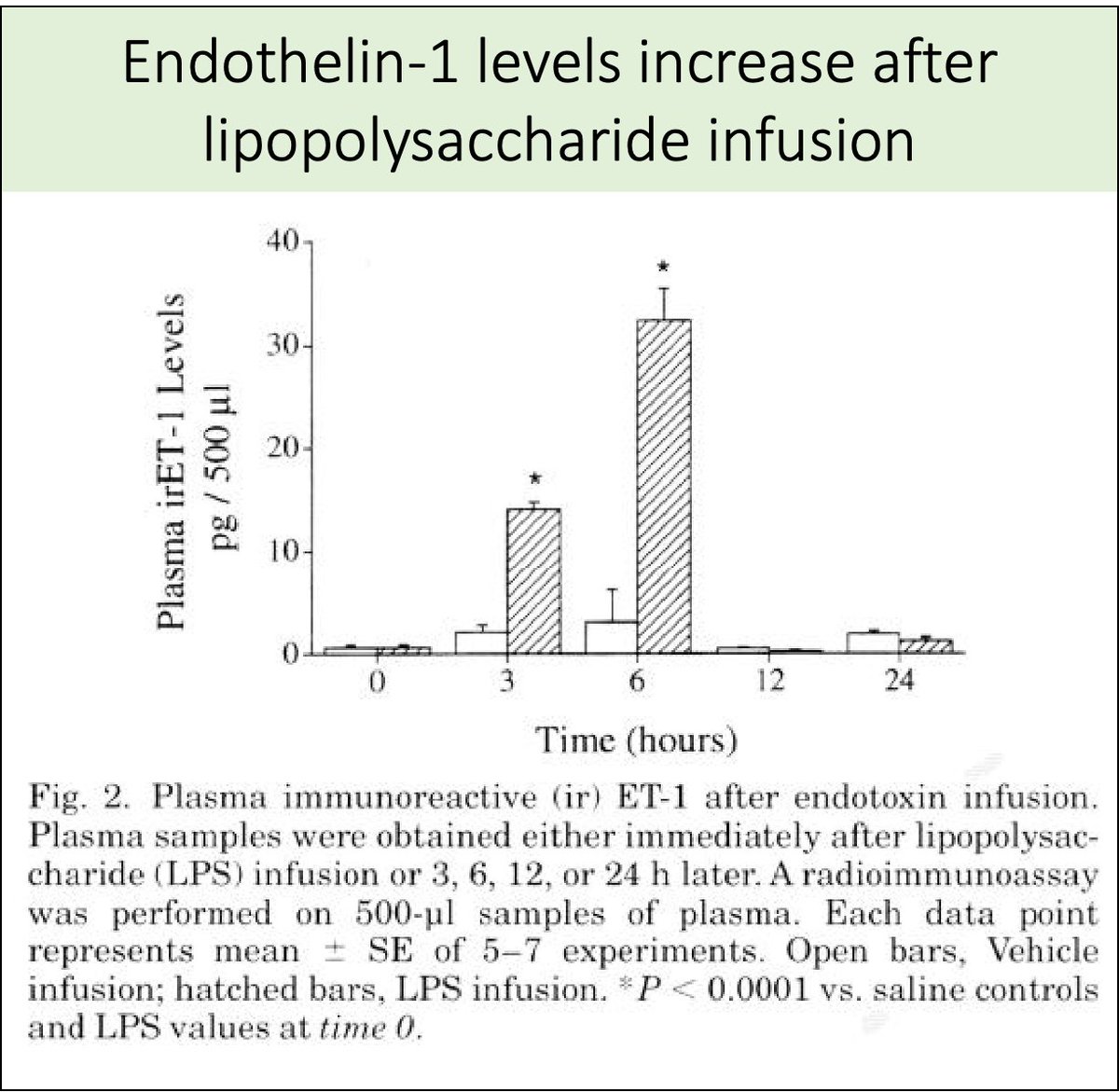
Increased endothelin-1 (ET-1) is another factor that might predispose to variceal rebleeding. How?
🔑First, ET-1 levels are increased by bacterial infections.
pubmed.ncbi.nlm.nih.gov
Increased endothelin-1 (ET-1) is another factor that might predispose to variceal rebleeding. How?
🔑First, ET-1 levels are increased by bacterial infections.
pubmed.ncbi.nlm.nih.gov
11/
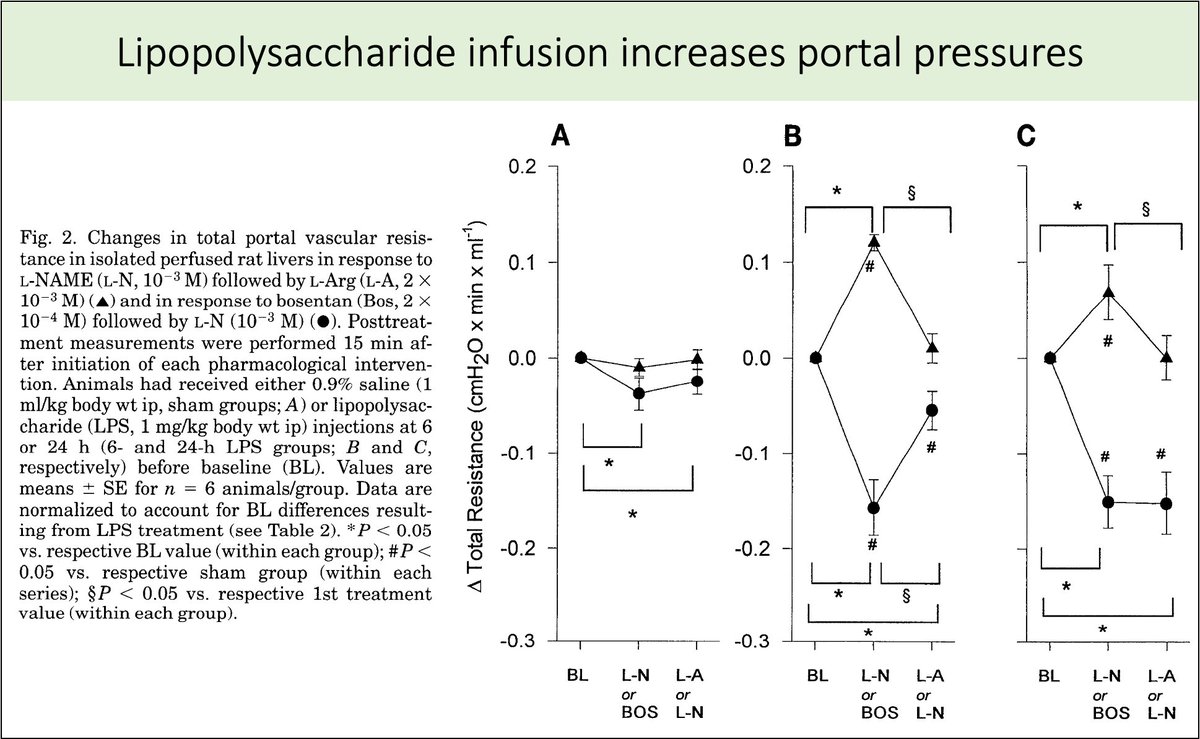
The increased ET-1 levels seen in bacterial infections might lead to worsening portal hypertension.
This was suggested in a study in which lipopolysaccharide infusion resulted in increased portal pressures and bleeding.
pubmed.ncbi.nlm.nih.gov
The increased ET-1 levels seen in bacterial infections might lead to worsening portal hypertension.
This was suggested in a study in which lipopolysaccharide infusion resulted in increased portal pressures and bleeding.
pubmed.ncbi.nlm.nih.gov
12/
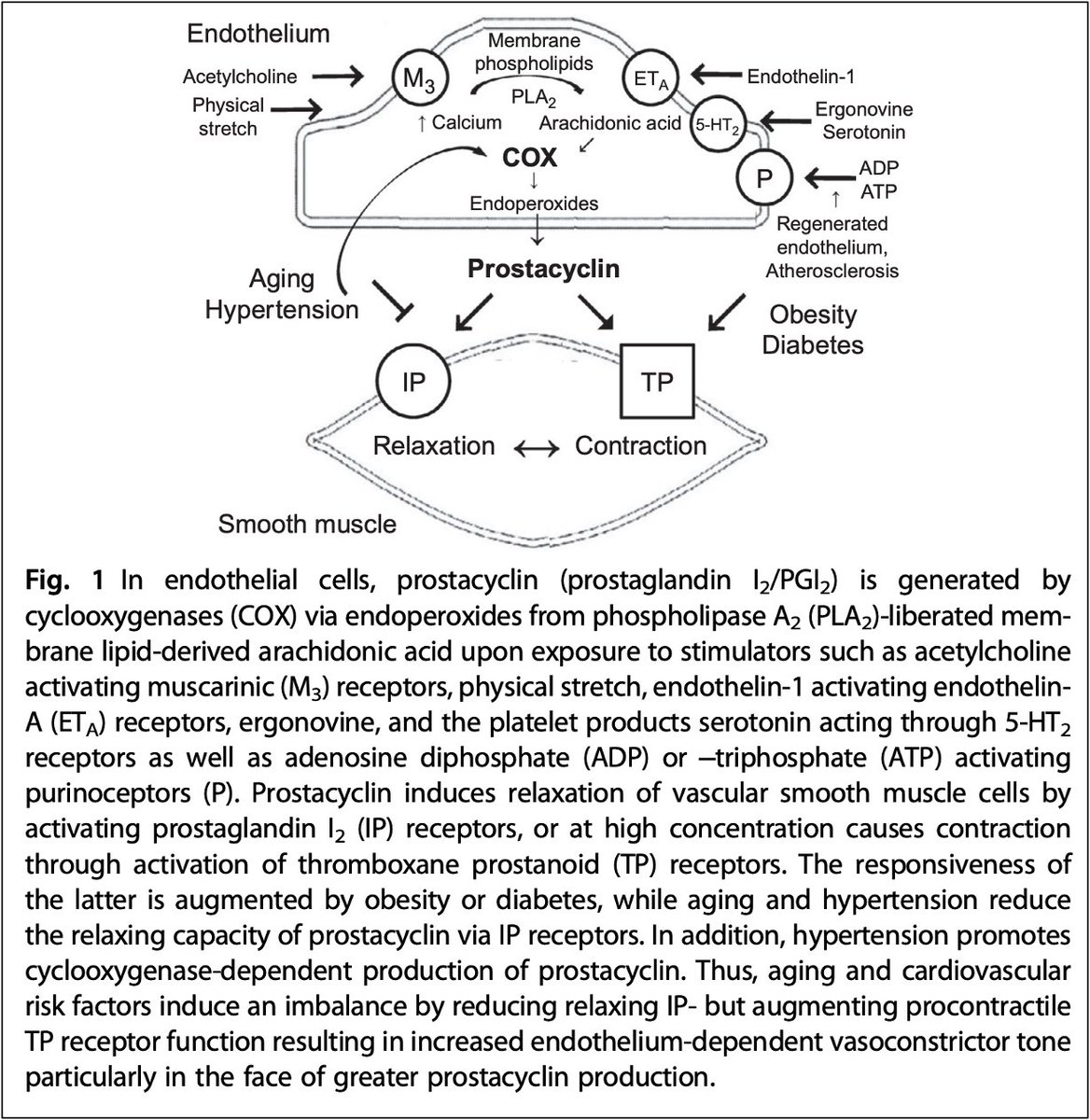
A final factor is platelet dysfunction.
In addition to affecting portal pressures, ET-1 also leads to increased prostacyclin, which decreased platelet aggregation.
pubmed.ncbi.nlm.nih.gov
A final factor is platelet dysfunction.
In addition to affecting portal pressures, ET-1 also leads to increased prostacyclin, which decreased platelet aggregation.
pubmed.ncbi.nlm.nih.gov
13/
Platelet adhesion and aggregation are also inhibited by nitric oxide.
I discussed this in a tweetorial covering uremic platelets.
Platelet adhesion and aggregation are also inhibited by nitric oxide.
I discussed this in a tweetorial covering uremic platelets.
14/
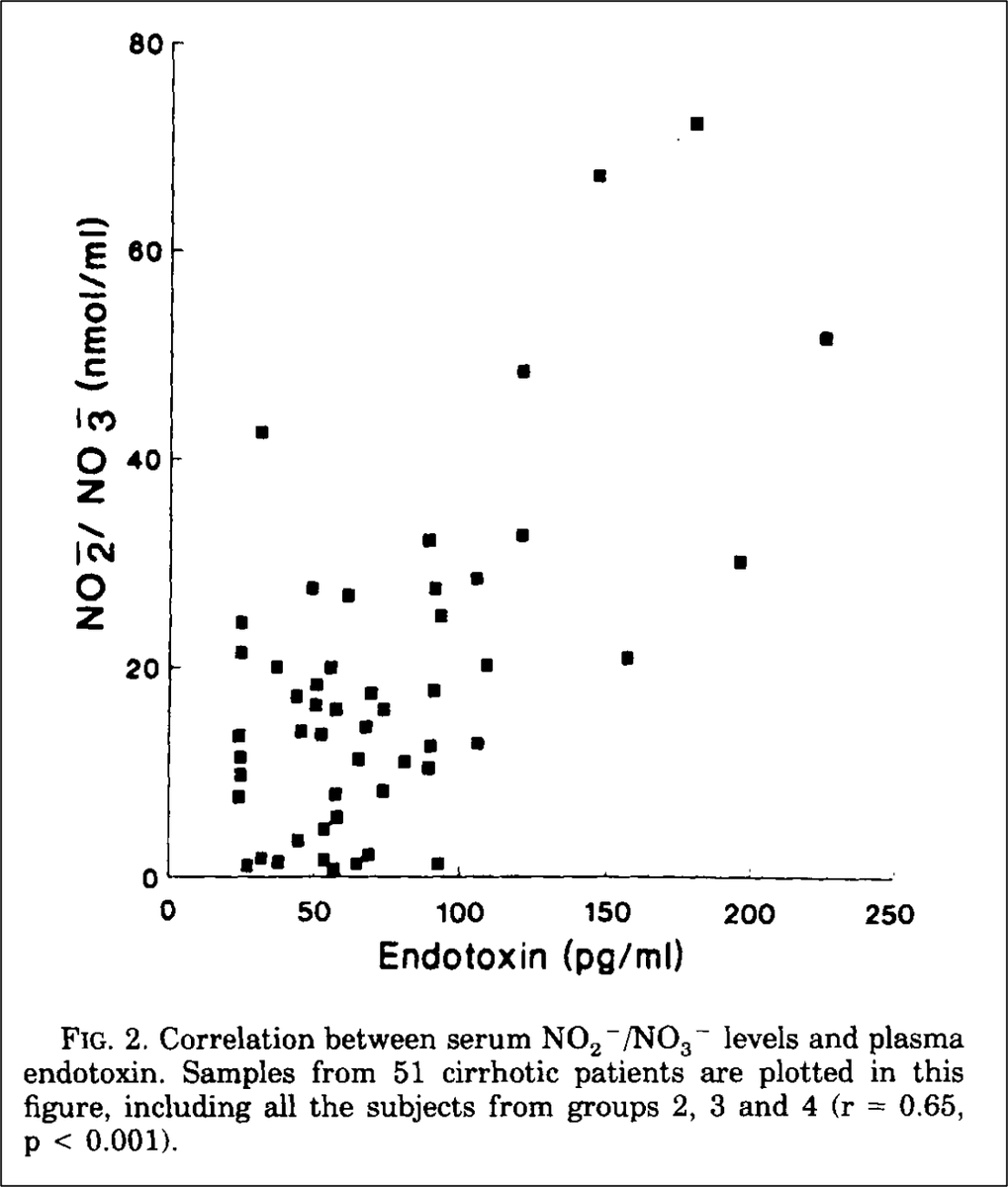
In cirrhosis, endotoxin is one of the causes of increased nitric oxide levels, even in those without bacterial infection.
Once infected, these levels rise further. This further worsens platelet function and predisposes to (re)bleeding.
pubmed.ncbi.nlm.nih.gov
In cirrhosis, endotoxin is one of the causes of increased nitric oxide levels, even in those without bacterial infection.
Once infected, these levels rise further. This further worsens platelet function and predisposes to (re)bleeding.
pubmed.ncbi.nlm.nih.gov
15/15
Collectively, the increased risk of bleeding seen in patients with cirrhosis and bacterial infection is multifactorial.
Regardless of the main mechanism, prophylactic antibiotics are effective at reducing this risk.
Use them wisely!
pubmed.ncbi.nlm.nih.gov
Collectively, the increased risk of bleeding seen in patients with cirrhosis and bacterial infection is multifactorial.
Regardless of the main mechanism, prophylactic antibiotics are effective at reducing this risk.
Use them wisely!
pubmed.ncbi.nlm.nih.gov
Loading suggestions...