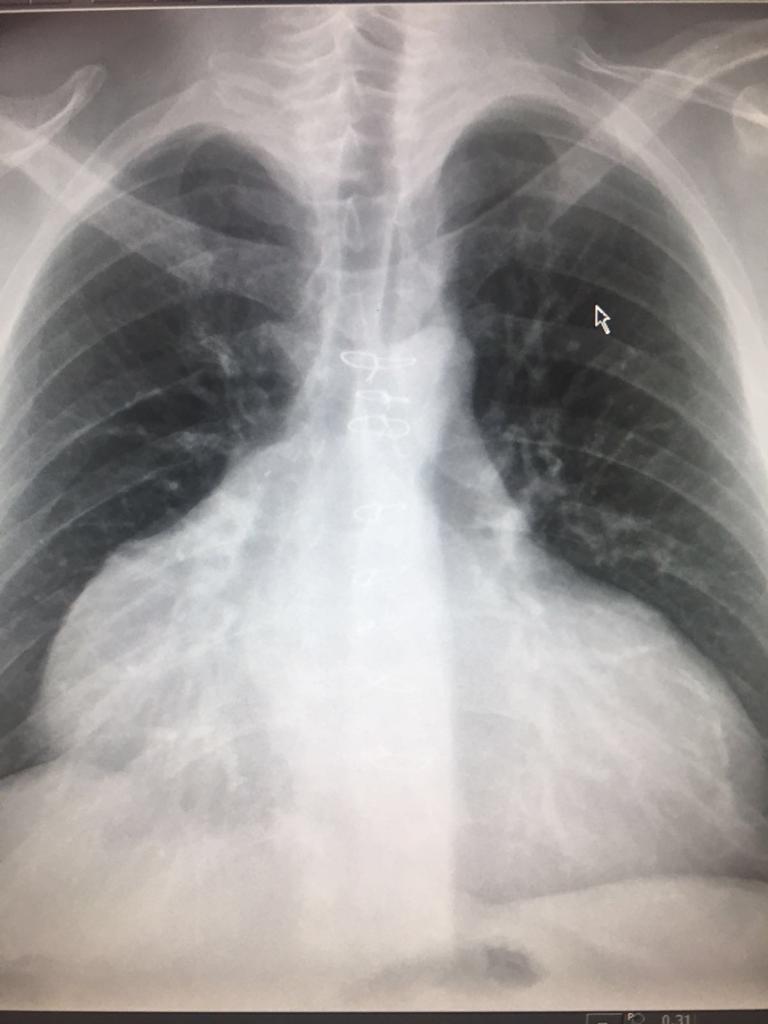
The initial management is very typical:
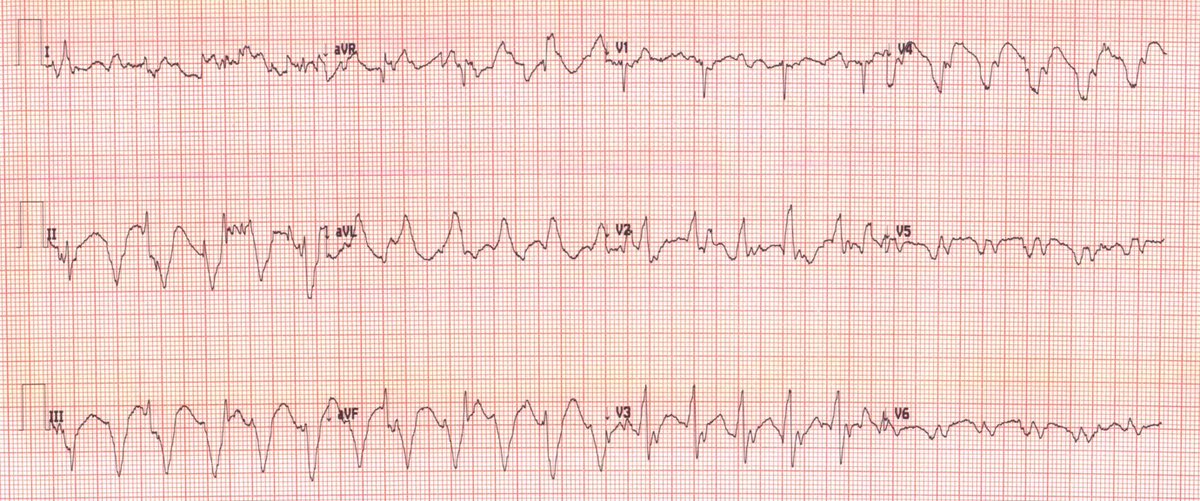
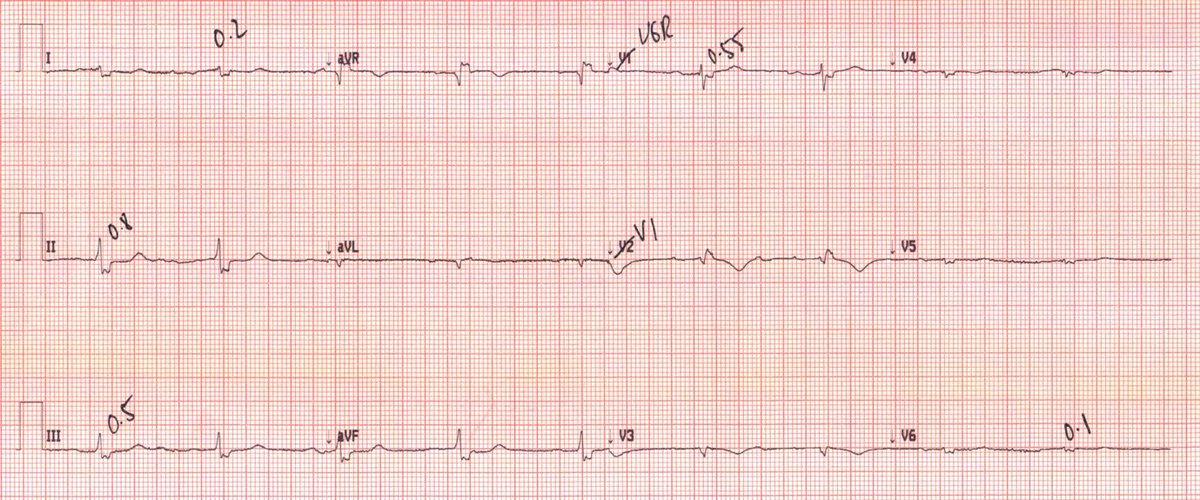
- Anti-arrhythmics is HD ok
- DCCV if not or failure to pharmacological options
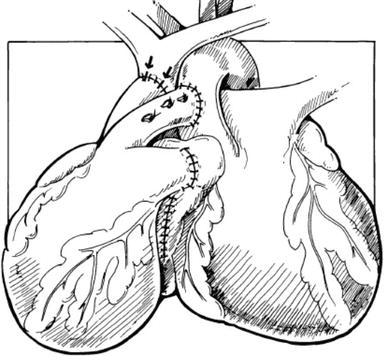
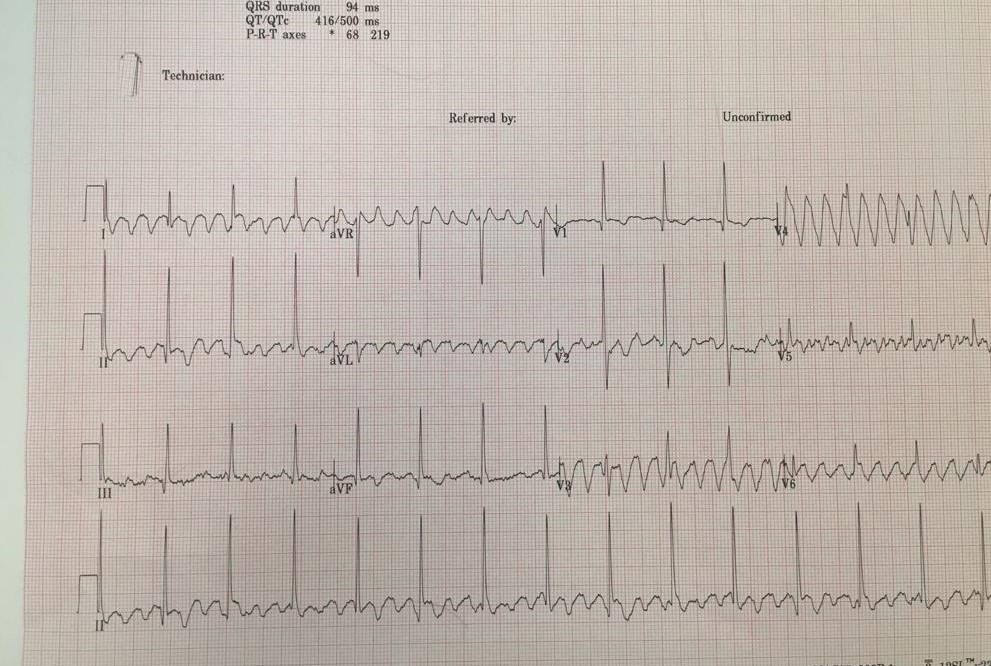
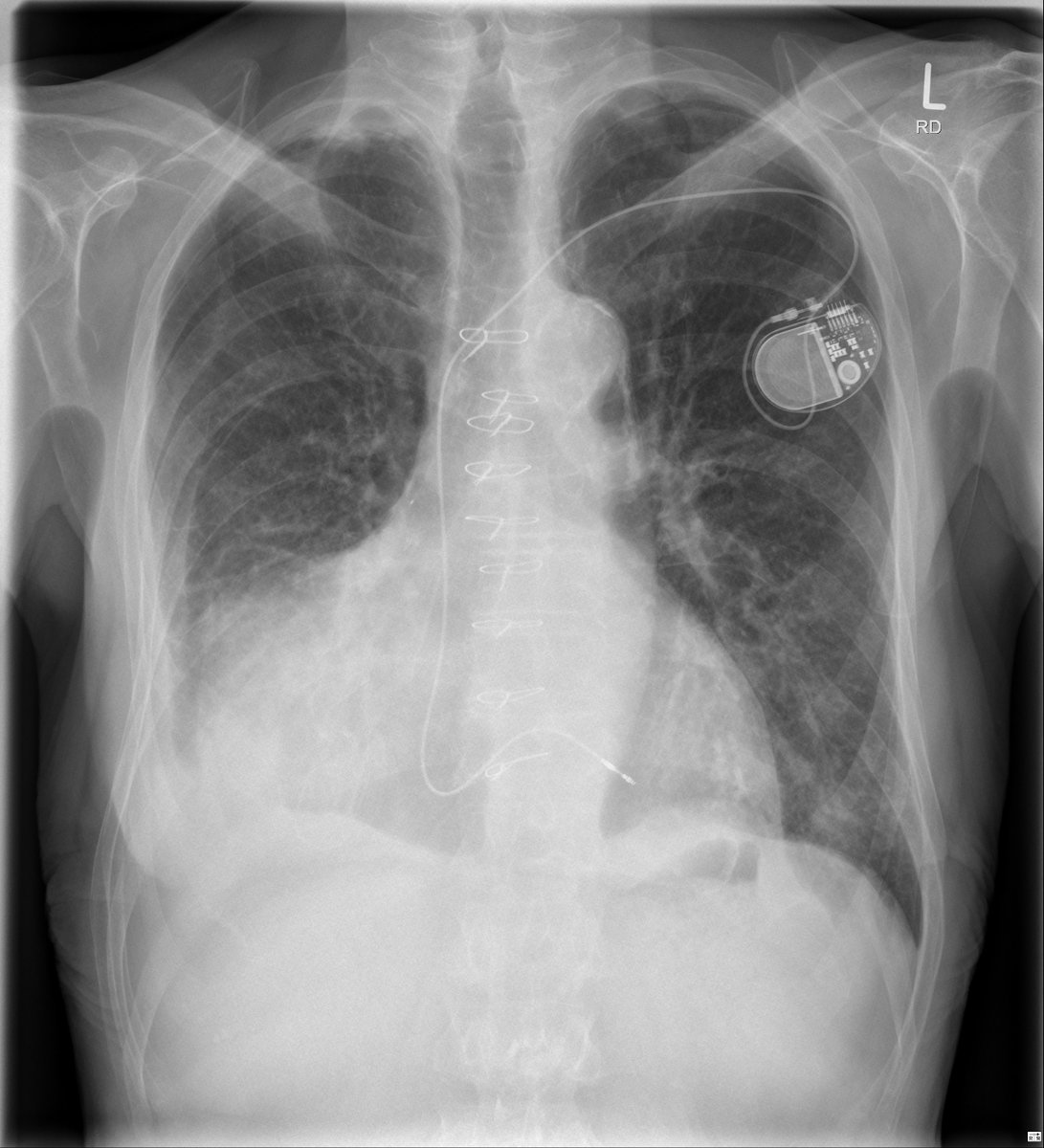
Interestingly, you need to synchronize the shock to donor's heart rhythm.
- Anti-arrhythmics is HD ok
- DCCV if not or failure to pharmacological options
Interestingly, you need to synchronize the shock to donor's heart rhythm.
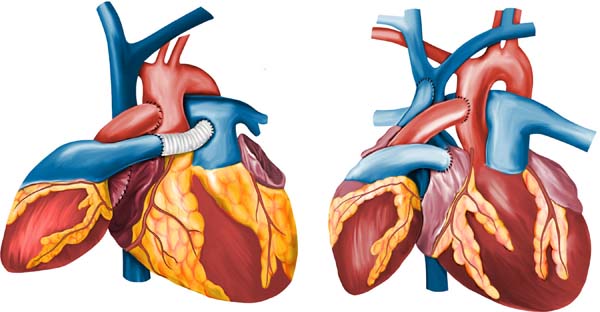
You shouldn't forget the donor's heart can have VT too, like in the traditional way of transplantation: CAV, rejection, scar, etc, so make sure you got right what ventricle it is!
What would you do then:
Can't even start with what lessons we learnt, it was a whole compendium of cardiology and physiology!
But happy to hear your comments and questions!
But happy to hear your comments and questions!
I hoped you liked this case and enjoyed this week as much as I did. It’s time to disconnect, too much cardiology!
But before I leave and handover the account to one of my pals, take the time to enjoy this song from my favorite band in the world.
open.spotify.com
But before I leave and handover the account to one of my pals, take the time to enjoy this song from my favorite band in the world.
open.spotify.com
Loading suggestions...