#JustAnOtherDayOnICU
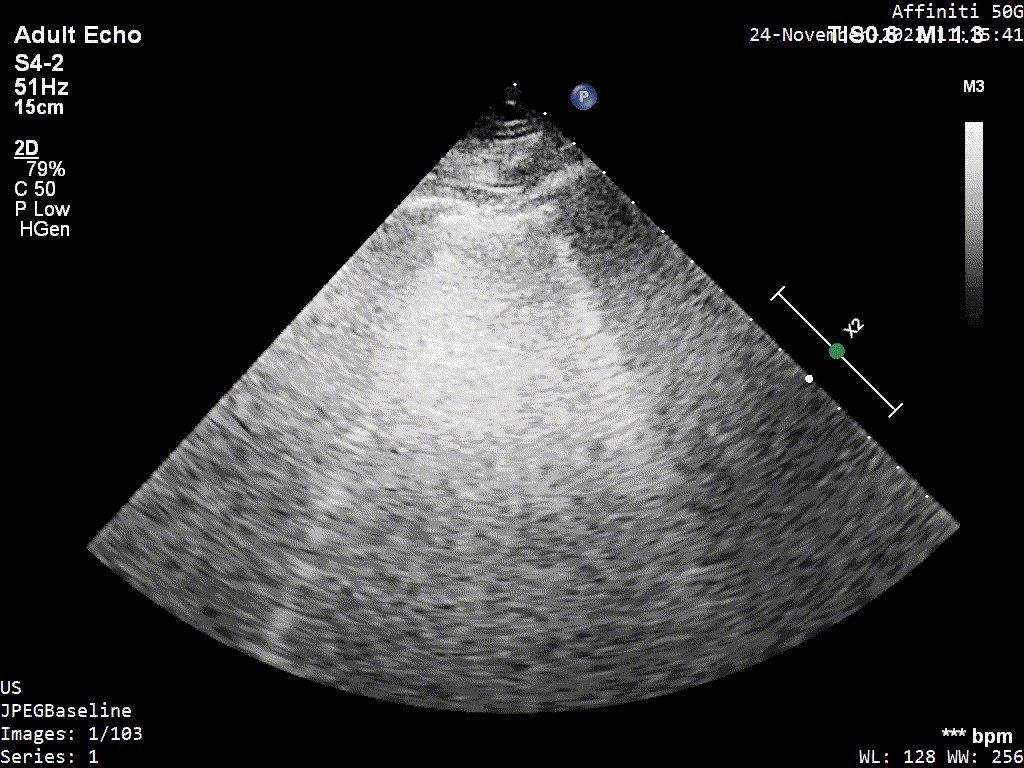
You are asked to do POCUS on a 72 y/o lady with increasing norepinephrine requirements (0.4 mcg/kg/min) and lactate second day post total pancreatectomy and splenectomy for ca.
Clips, questions and 'what happened' in the long thread below.
#POCUS #EchoFirst
You are asked to do POCUS on a 72 y/o lady with increasing norepinephrine requirements (0.4 mcg/kg/min) and lactate second day post total pancreatectomy and splenectomy for ca.
Clips, questions and 'what happened' in the long thread below.
#POCUS #EchoFirst
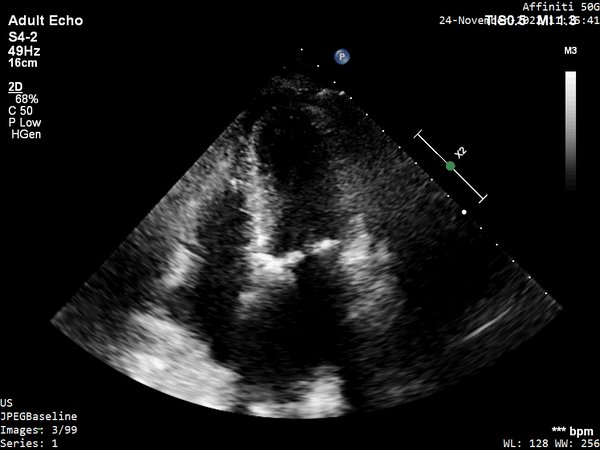
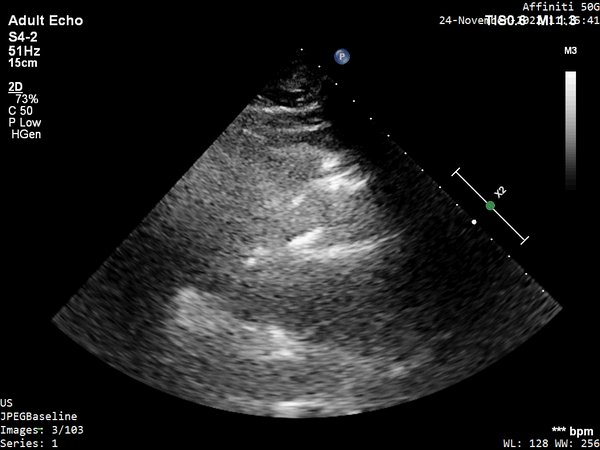
11/ So what's the probelm and haemodynamic intervention you suggest?
1) Fluid challenge
2) Beta blockers
3) Vasopressin
4) Something else
1) Fluid challenge
2) Beta blockers
3) Vasopressin
4) Something else
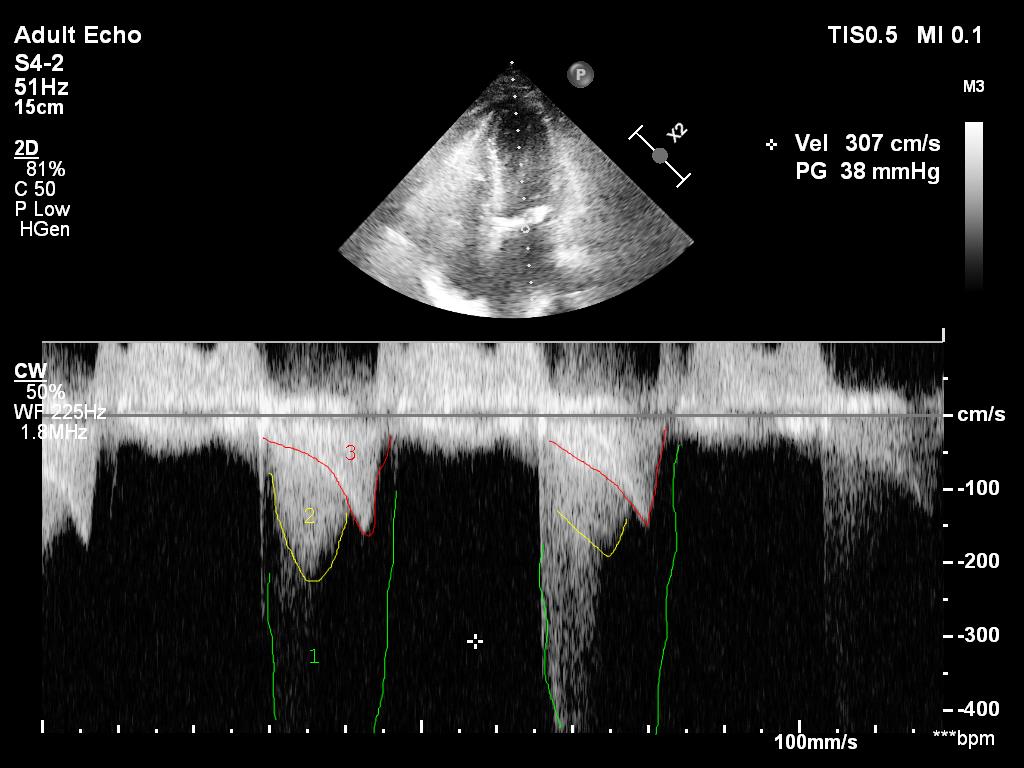
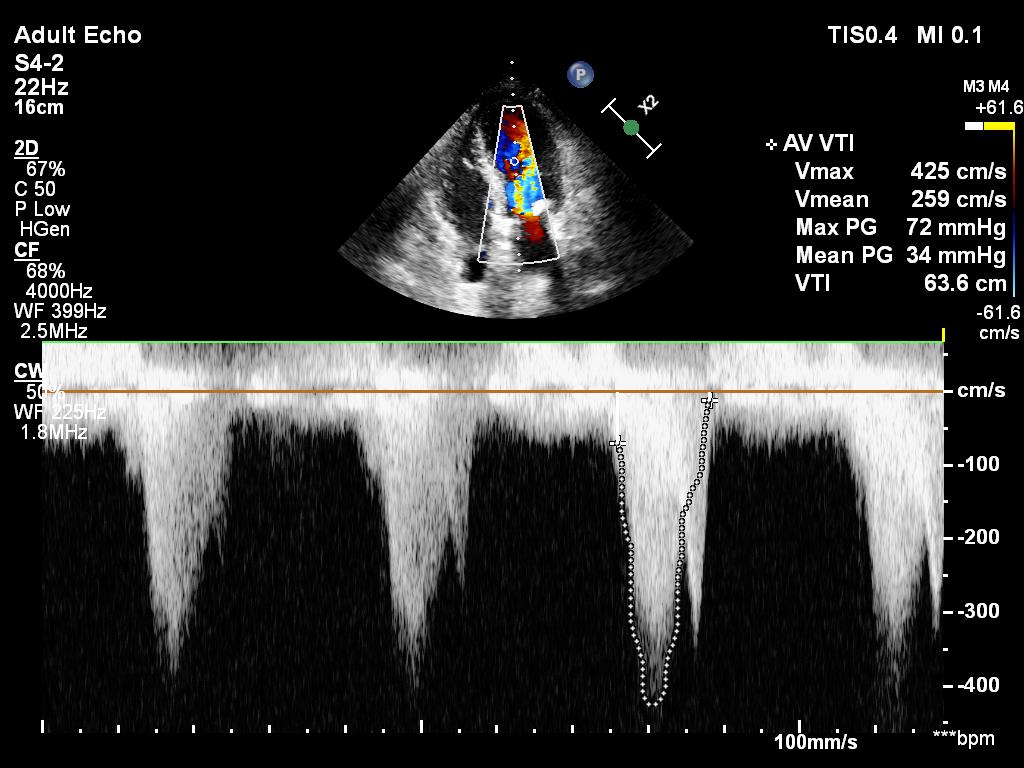
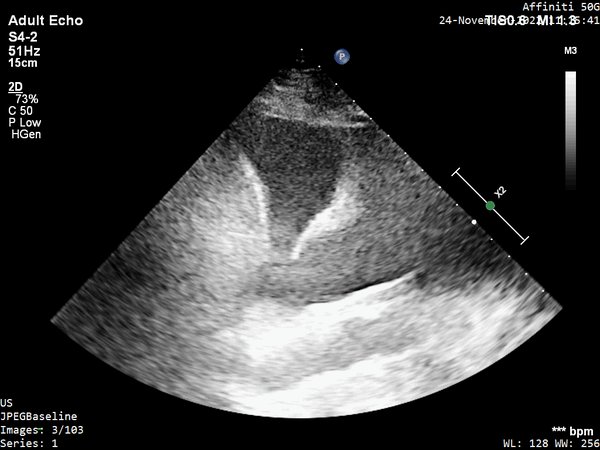
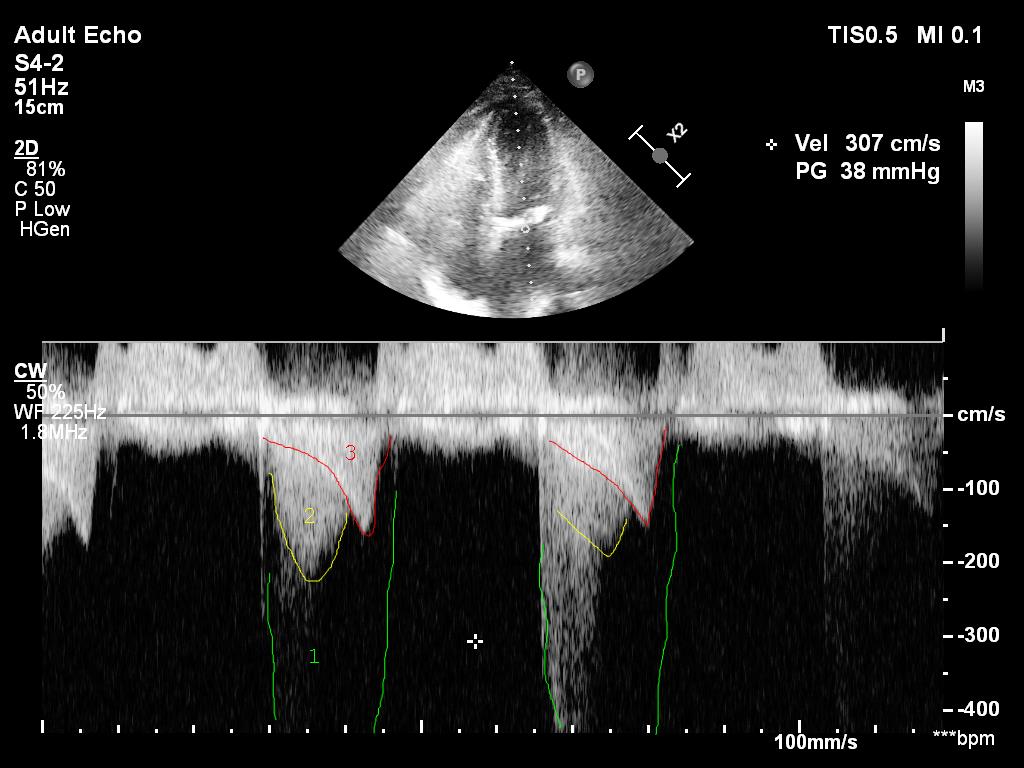
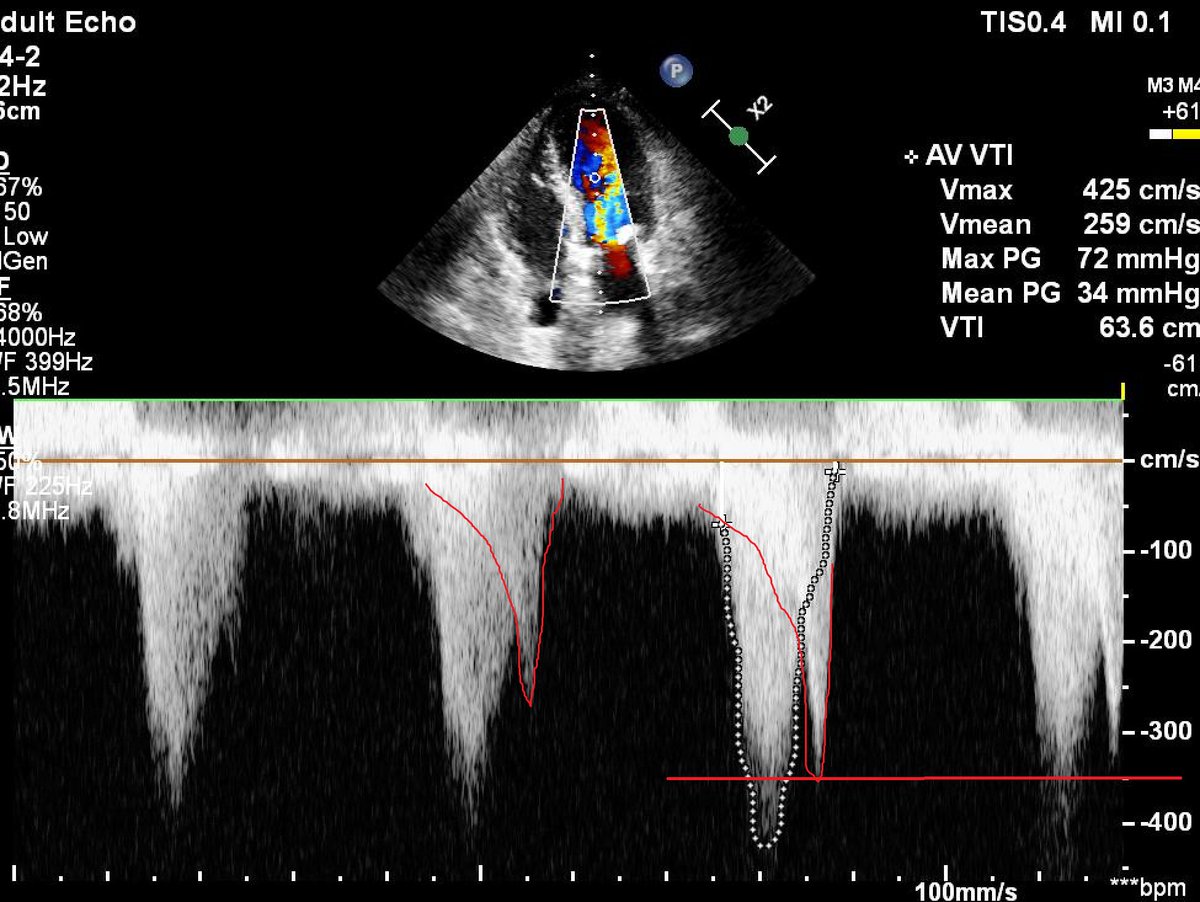
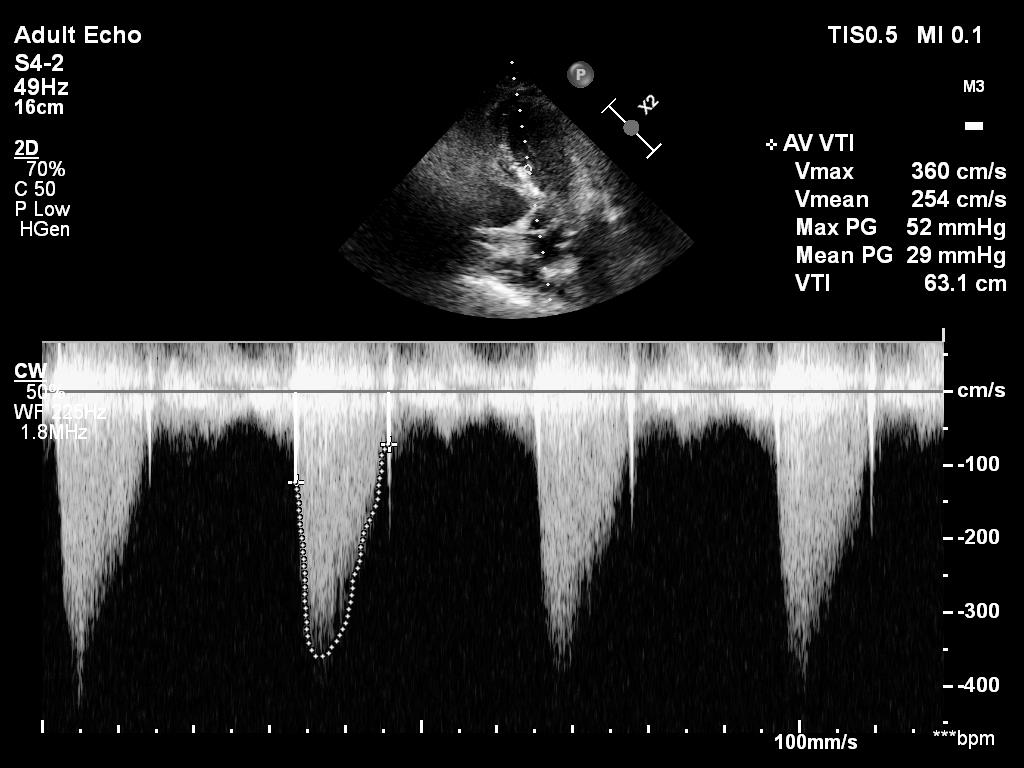
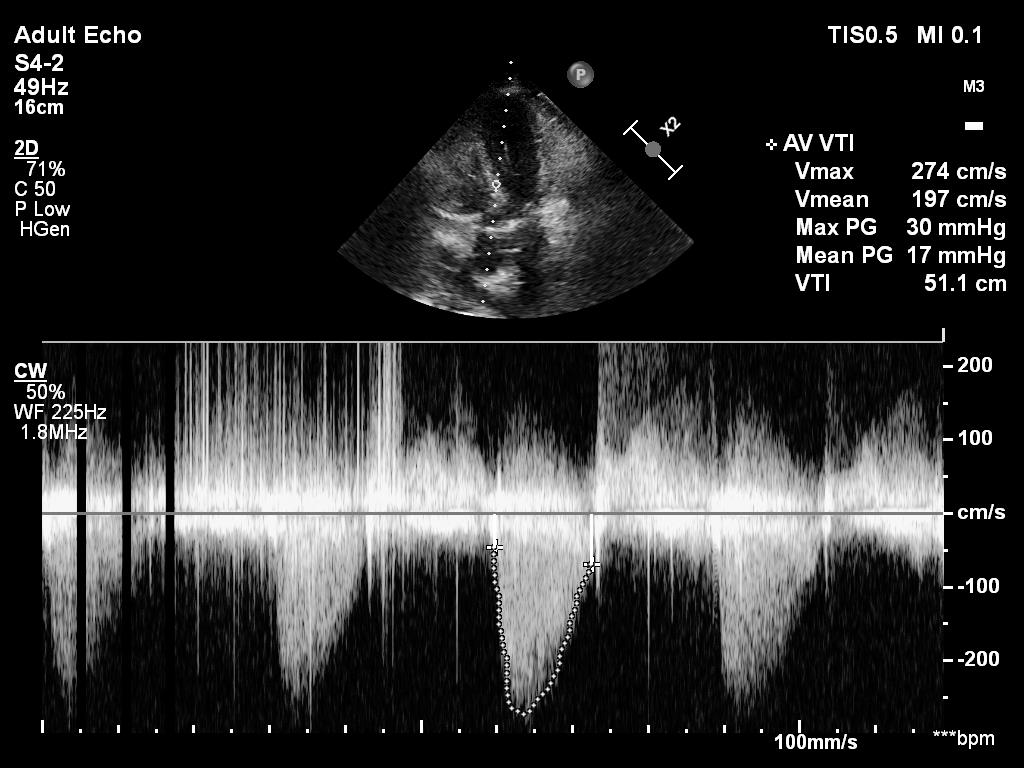
14/ If I just look at the mean gradient on the previous clip (34hgmm), there is. However, it is impossible to calculate the true gradient if there is an intraventricular obstruction.
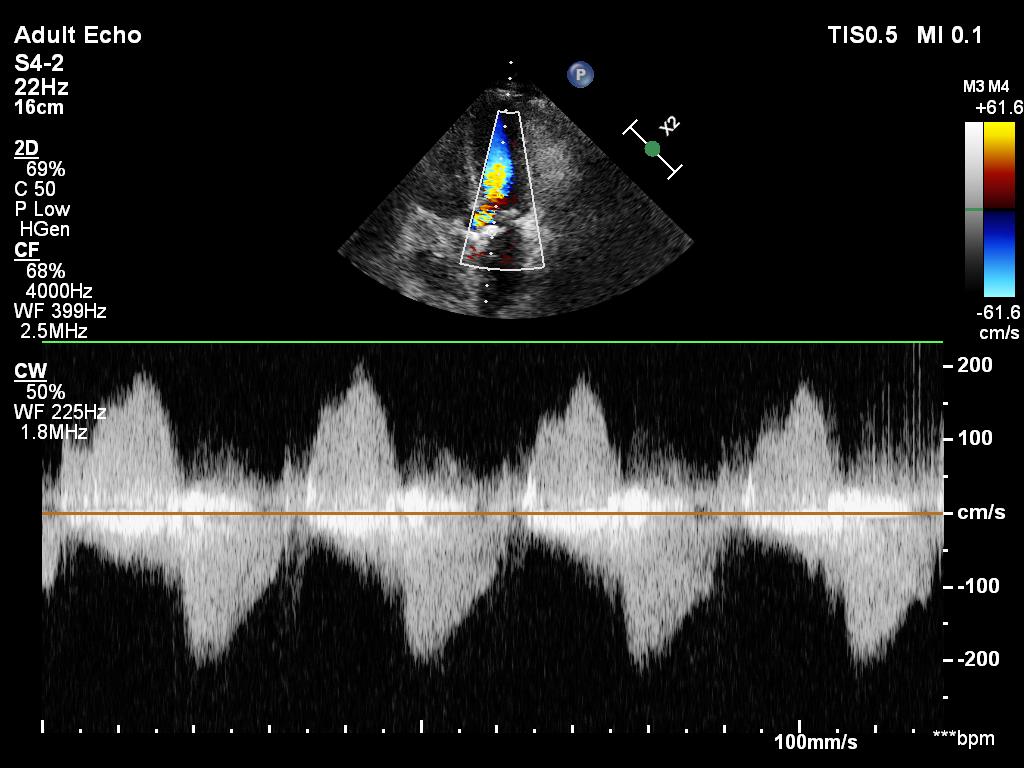
16/ Intraventricular obstruction can be caused by:
1) reduced LV filling du to hypovolemia or vasodilatation
2) reduced afterload due to vasodilatation
3) LV hypertrophy secondary to a sclerotic aortic valve/hypertension (this case)
1) reduced LV filling du to hypovolemia or vasodilatation
2) reduced afterload due to vasodilatation
3) LV hypertrophy secondary to a sclerotic aortic valve/hypertension (this case)
17/ 4) hypercontractile LV due to endogenous or exogenous cathecolamines
5) HCM or other structural abnormalities not present in this case
5) HCM or other structural abnormalities not present in this case
18/ Treatment is logical:
1) fluids
2) avoid cathecolamines especially dobutamine, but vasopressin is best
3) beta-blockers
More on this @PulmCrit emcrit.org though this is not a classic LVOTO with SAM, the obstruction is intra/midventricular.
1) fluids
2) avoid cathecolamines especially dobutamine, but vasopressin is best
3) beta-blockers
More on this @PulmCrit emcrit.org though this is not a classic LVOTO with SAM, the obstruction is intra/midventricular.
19/ In this case I advised starting vasopressin but holding fluids and Also beta blockers for now.
My rationale behind fluids was that the patient was already net positive 3000ml in 24 hrs, urine output was low.
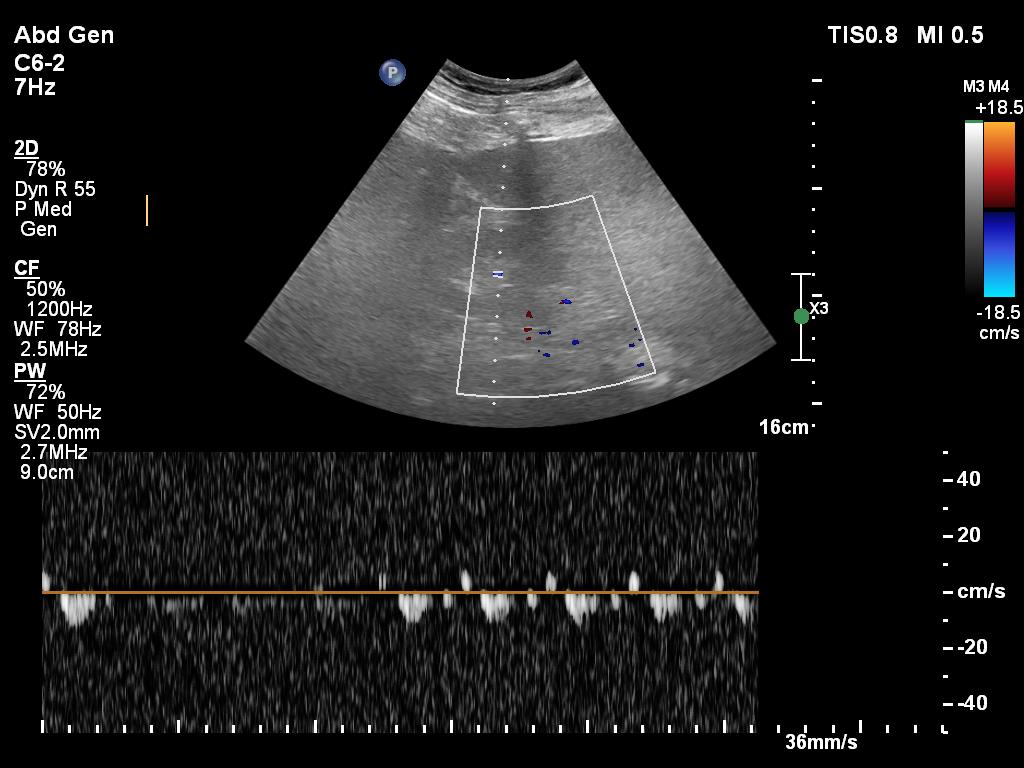
POCUS showed 'fluids' in the lungs (B profile, pleural effusion).
My rationale behind fluids was that the patient was already net positive 3000ml in 24 hrs, urine output was low.
POCUS showed 'fluids' in the lungs (B profile, pleural effusion).
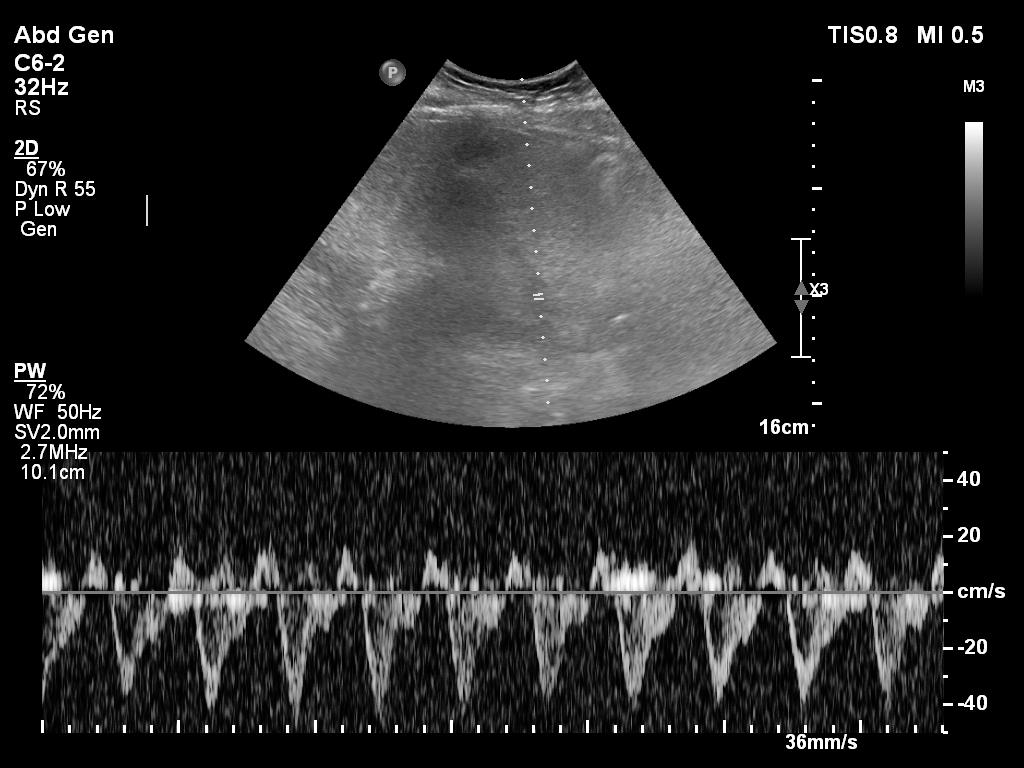
20/ My interpretation of VEXUS is Grade I: normal hepatic vein, mild portal vein pulsatility and biphasic renal vein flow. But pancreatitis is a 'leaky' state, so VEXUS is often not very abnormal as fluid readily leaks to the tissues.
21/ What happened?
After starting vasopressin with 2U/h noradrenaline could be reduced and intraventricular obstruction improved from 43hgmm to 9 hgmm. Urine output picked up. Pt was discharged 2 days later.
After starting vasopressin with 2U/h noradrenaline could be reduced and intraventricular obstruction improved from 43hgmm to 9 hgmm. Urine output picked up. Pt was discharged 2 days later.
24/
Lastly a theoretical haemodynamic question:
Can reduction of afterload lead to intraventricular obstruction if there is a sclerotic aortic valve? Does it not provide a 'fixed obstruction' that overrides reduction of afterload due to vasodilatation?
Lastly a theoretical haemodynamic question:
Can reduction of afterload lead to intraventricular obstruction if there is a sclerotic aortic valve? Does it not provide a 'fixed obstruction' that overrides reduction of afterload due to vasodilatation?
Was intraventricular gradient mediated more via venodilatation and preload reduction?
What do you think @msiuba @NephroP @ArgaizR @ThinkingCC @drmarcogarrone @khaycock2 ?
What do you think @msiuba @NephroP @ArgaizR @ThinkingCC @drmarcogarrone @khaycock2 ?
Loading suggestions...