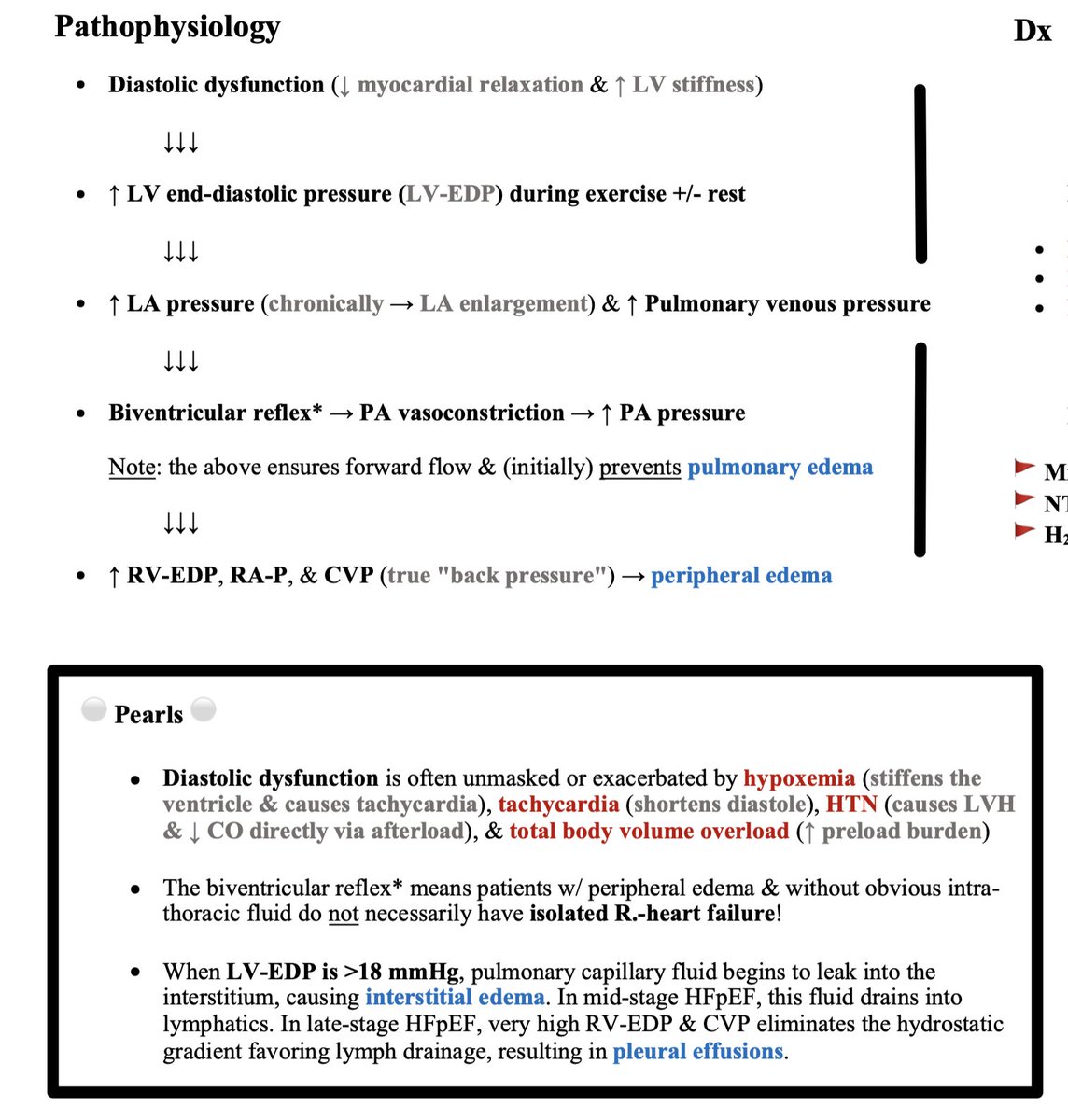
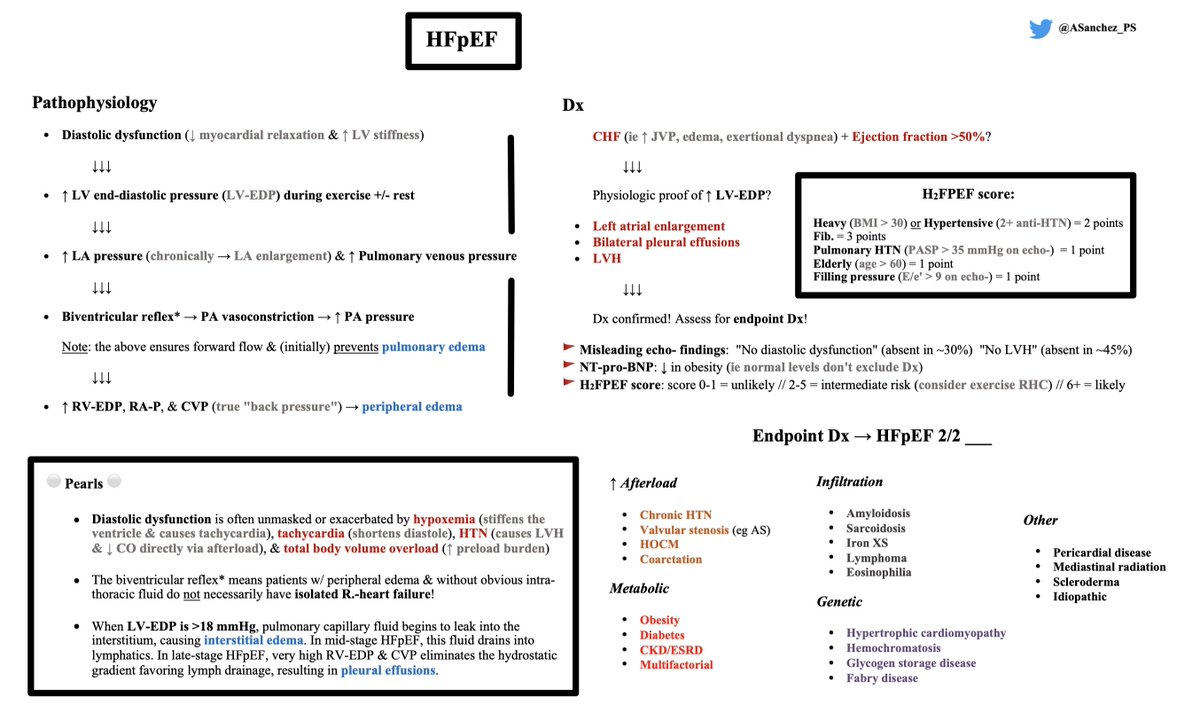
The pathophys of HFpEF first involves diastolic dysfunction.
(This may or may not be visualized on TTE; more on this in a second.)
With an expected ↑ LV-EDP during exercise (+/- at rest), LA pressure then ↑.
This will, chronically, lead to LA enlargement.
(This may or may not be visualized on TTE; more on this in a second.)
With an expected ↑ LV-EDP during exercise (+/- at rest), LA pressure then ↑.
This will, chronically, lead to LA enlargement.
Pulmonary venous pressure then ↑. In order for forward blood flow to be maintained in the face of this increased pressure, what can be called the "biventricular reflex" ensues, leading to PA vasoconstriction.
Of note, this process (initially) *prevents* pulmonary edema.
Of note, this process (initially) *prevents* pulmonary edema.
However, resultant ↑ RV-EDP, RA-P, & CVP (true "back pressure") *does* lead to peripheral edema 💧🦿
Why is this pathophys important? It means patients w/ peripheral edema & without obvious intra-thoracic fluid do *not* necessarily have isolated R.-heart failure! ❌
Why is this pathophys important? It means patients w/ peripheral edema & without obvious intra-thoracic fluid do *not* necessarily have isolated R.-heart failure! ❌
When LV-EDP is >18, pulmonary capillary fluid leaks into the interstitium → interstitial edema. In mid-stage HFpEF, this fluid drains into lymphatics ✔️
In late-stages, very high RV-EDP & CVP eliminates the hydrostatic gradient favoring lymph drainage → pleural effusions 😔
In late-stages, very high RV-EDP & CVP eliminates the hydrostatic gradient favoring lymph drainage → pleural effusions 😔
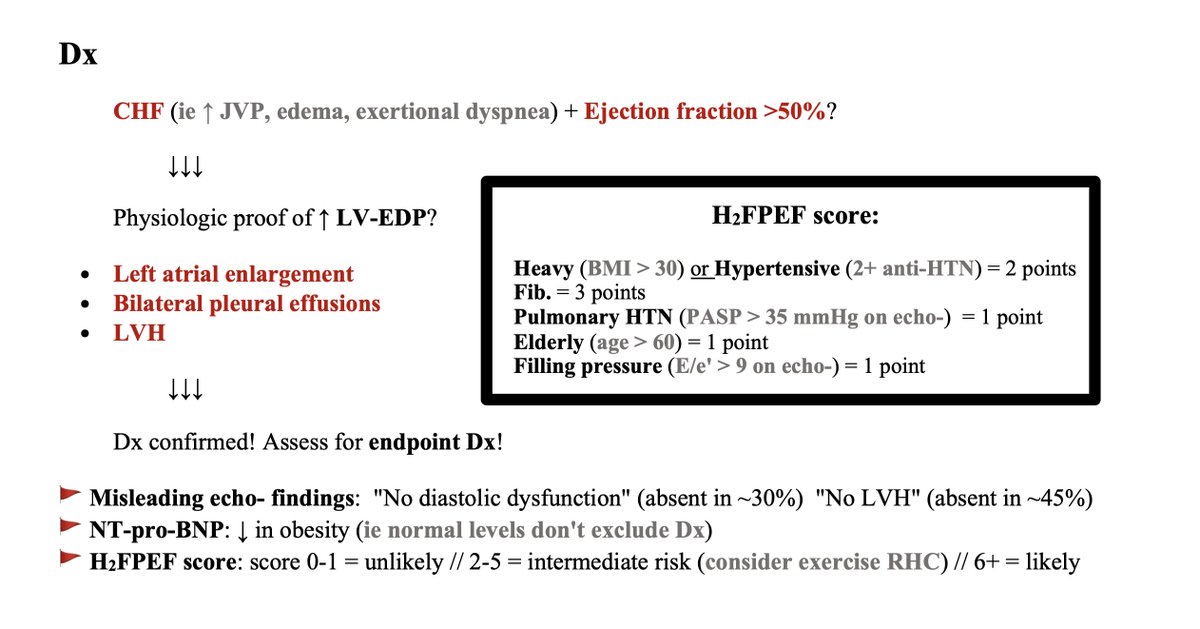
As promised, let's go through my birds'-eye view approach to how to clinch this Dx 🔍
You see a patient with CHF (ie ↑ JVP, edema, exertional dyspnea) & see a TTE with EF >50%...
You see a patient with CHF (ie ↑ JVP, edema, exertional dyspnea) & see a TTE with EF >50%...
Step 1: is there physiologic proof of ↑ LV-EDP on imaging?
- Left atrial enlargement?
- Bilateral pleural effusions?
- LVH?
Yes = Dx confirmed! ✅
These findings are *proof*: remember the pathophys!
- Left atrial enlargement?
- Bilateral pleural effusions?
- LVH?
Yes = Dx confirmed! ✅
These findings are *proof*: remember the pathophys!
That's it. It's that simple!
The real key is to not be fooled by the following 🔑 :
- "No diastolic dysfunction" on TTE (absent in ~30%)
- "No LVH" on TTE (absent in ~45%)
If you see b/l pleural effusions (even if *small*), you're *very* likely dealing with HFpEF.
The real key is to not be fooled by the following 🔑 :
- "No diastolic dysfunction" on TTE (absent in ~30%)
- "No LVH" on TTE (absent in ~45%)
If you see b/l pleural effusions (even if *small*), you're *very* likely dealing with HFpEF.
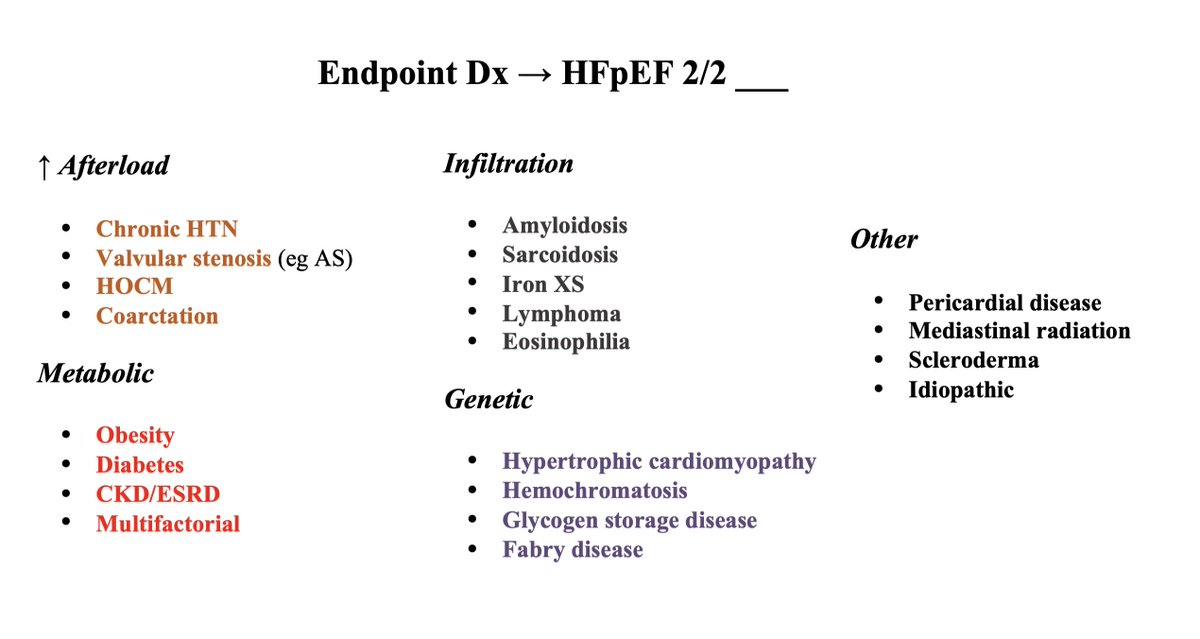
Finally, don't forget your patient with HFpEF needs an Endpoint Dx: could they have amyloidosis (increasingly recognized), or do they simply have multiple metabolic risk factors?
Framework below adapted from @AndreMansoor.
Reference: amazon.com
Framework below adapted from @AndreMansoor.
Reference: amazon.com
🏁 That completes my overview of an approach to HFpEF Dx!
I hope this is viewed as a helpful framework for medicine residents & internists. More nuanced takes definitely available in the @CardioNerds world 🌎
I hope this is viewed as a helpful framework for medicine residents & internists. More nuanced takes definitely available in the @CardioNerds world 🌎
Loading suggestions...