5 cognitive fallacies in hemodynamic management 🧵
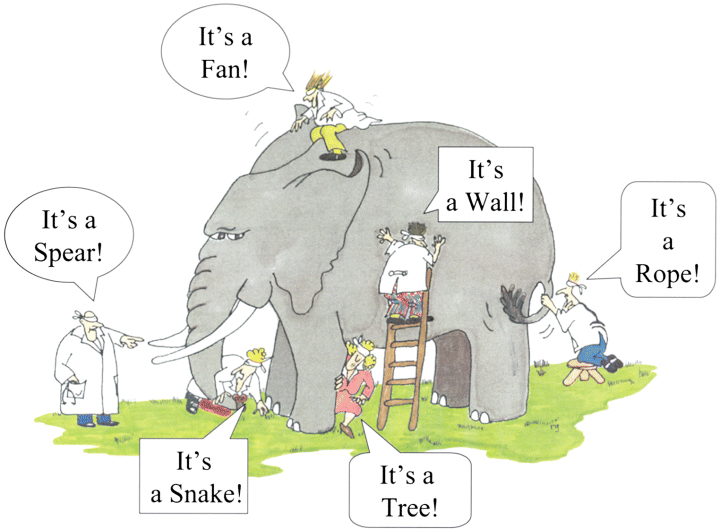
1⃣We think there are 4 categories of shock
2⃣We see only norepi-doses and BP
3⃣We think ⬆️norepi 🟰shock
4⃣We stop after diagnosing the shock syndrome
5⃣We're lazy and shortsighted
#FOAMcc #FOAMed #IntensiveCare #CriticalCare
1⃣We think there are 4 categories of shock
2⃣We see only norepi-doses and BP
3⃣We think ⬆️norepi 🟰shock
4⃣We stop after diagnosing the shock syndrome
5⃣We're lazy and shortsighted
#FOAMcc #FOAMed #IntensiveCare #CriticalCare
No monitoring device will cause patient benefit if it is interpreted wrongly or not coupled with correct therapy; Our minds are the connection between the findings and the therapy.
Unfortunately, the mind often erroneously applied. Worse: only the patient pays the price.
1/n
Unfortunately, the mind often erroneously applied. Worse: only the patient pays the price.
1/n
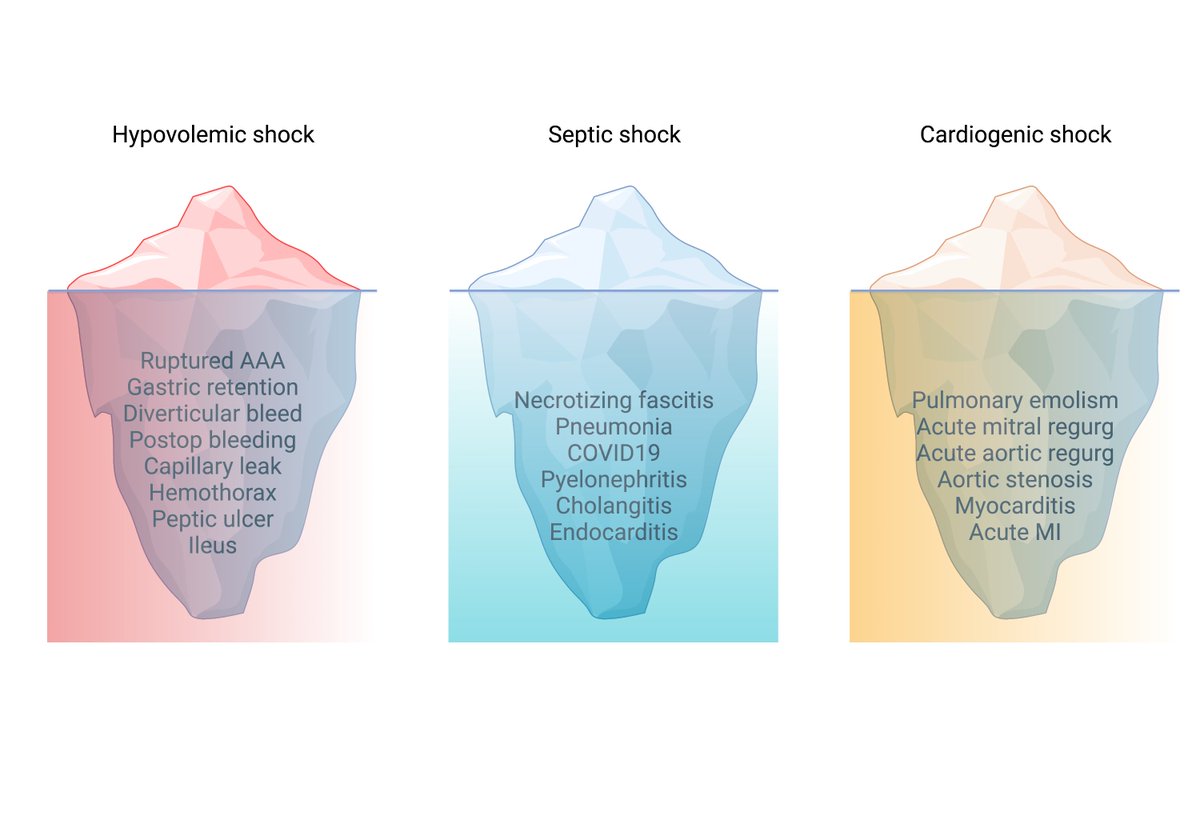
1⃣Fitting the patient into the 4 categories of shock (2/2).
The categorical approach is too simplistic. Traumapatients ("hypovolemic" category) can be vasodilated AND hypovolemic. When treating them ONLY as hypovolemic, we will overtransfuse them.
Shock is never categorical.
3/n
The categorical approach is too simplistic. Traumapatients ("hypovolemic" category) can be vasodilated AND hypovolemic. When treating them ONLY as hypovolemic, we will overtransfuse them.
Shock is never categorical.
3/n
3⃣We mistake the map as the territory (1/2)
We think ⬆️norepi requirements🟰shock, and needs correction. But, if the patient is well perfused, this is not shock and does not require correction. In fact, if the cause is arterial dilatation, is the correct therapy.
5/n
We think ⬆️norepi requirements🟰shock, and needs correction. But, if the patient is well perfused, this is not shock and does not require correction. In fact, if the cause is arterial dilatation, is the correct therapy.
5/n
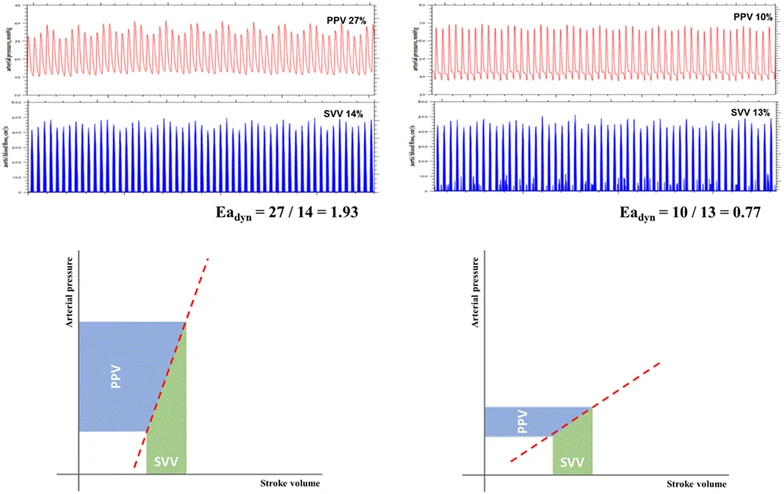
3⃣We mistake the map as the territory (2/2)
Many try to reduce the norepi requirements by giving fluids. Unfortunately, if the cause is arterial dilatation, fluids will not reduce norepi requirements - even if the patient is fluid responsive
link.springer.com
6/n
Many try to reduce the norepi requirements by giving fluids. Unfortunately, if the cause is arterial dilatation, fluids will not reduce norepi requirements - even if the patient is fluid responsive
link.springer.com
6/n
5⃣Laziness and shortsightesness (1/3)
We are, unfortunately, lazy and shortsighted - also when managing hemodynamics. The patient pays the price.
We give fluids instead of examining for fluid responsiveness/tolerance. This leads to fluid overload, and poor outcomes.
8/n
We are, unfortunately, lazy and shortsighted - also when managing hemodynamics. The patient pays the price.
We give fluids instead of examining for fluid responsiveness/tolerance. This leads to fluid overload, and poor outcomes.
8/n
5⃣Laziness and shortsightesness (2/3)
We increasing norepi-doses instead of diagnosing the cause. If the reason isn't arterial vasodilatation, this delays the correct treatment and exposes the patient to organ dysfunction.
9/n
We increasing norepi-doses instead of diagnosing the cause. If the reason isn't arterial vasodilatation, this delays the correct treatment and exposes the patient to organ dysfunction.
9/n
5⃣Laziness and shortsightesness (3/3)
Pushing CO and BP in patients with cardiac failure, forgetting that this increases myocardial O2-demand, ⬆️risk of myocardial injury/ischemia and future decompensation.
10/n
Pushing CO and BP in patients with cardiac failure, forgetting that this increases myocardial O2-demand, ⬆️risk of myocardial injury/ischemia and future decompensation.
10/n
Conclusion:
We are seldom overtly punished for our fallacies. Rather, it is the patient that pays the price. Avoid the fallacies requires daily effort - but what worthy goal doesn't require effort? #Stoicism
11/11 end 🧵
We are seldom overtly punished for our fallacies. Rather, it is the patient that pays the price. Avoid the fallacies requires daily effort - but what worthy goal doesn't require effort? #Stoicism
11/11 end 🧵
Loading suggestions...