1/ Another challenging case-based discussion. Help me manage this patient #medtwitter #neurotwitter #stroke. A #tweetorial 🧵. 🙏 to the great @sudhakar_satti for reviewing this case with me and sending me insights and pictures! Amazing team-work @NeuroChristiana @christianacare
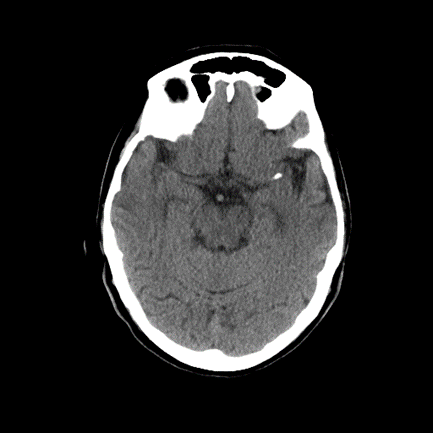
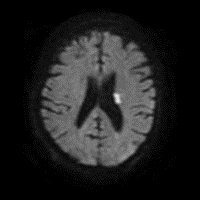
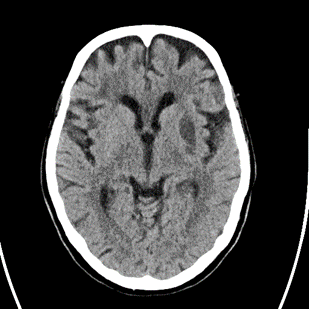
2/ Elderly person with #HTN #HLD 🚬 who wakes up with R-sided weakness, mild aphasia, NIHSS 8 at outside 🏥. 🚫 lytics as wake-up, but CT with #denseMCA and CTA with a left M1 non occlusive thrombus. Transferred for #thrombectomy evaluation. Imaging as follows:
4/ How do you manage the patient?
6/ ⚠⚠⚠ The patient now develops worsening right sided weakness, aphasia, dysarthria, NIHSS = 8. #strokealert ⏳=🧠 reactivated, but upon evaluation, NIHSS returns to 3. How would you manage now?
7/ Patient is transferred to the #NeuroCriticalCare unit for close monitoring, layed flat, started on fluids. CT head with 🚫 new infarct, unchanged calcification distal left M1 and Sx improve. We keep DAPT + HOB flat and IVF
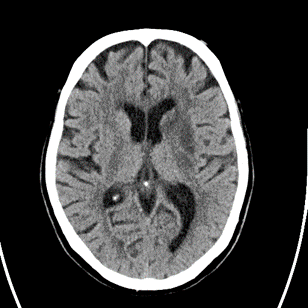
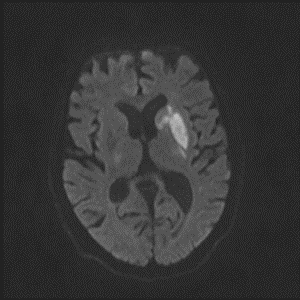
8/ Next evening, patient does the same thing, NIHSS=8, word-🥗, worsening right hemiparesis. #Strokealert again and CT with new stroke noted. BP at this time 110s:
10/ What do you do now??
11/ Because we felt this was ruptured plaque, managed with IVF and HOB flat w/ plan to start pressors, but BP ⬆ and symptoms resolved. #PRU was therapeutic too. ⚠ Next evening (at same⌚), patient does the same thing again! SBP 140s this time. What do you think is going on?
12/ Patient now on continuous #EEG, event captured and without evidence of seizures on EEG. How do you manage the patient?
13/ By now we are considering stent placement, but #WEAVE data suggests waiting 7 days is best to ⬇ periprocedural complications: ahajournals.org
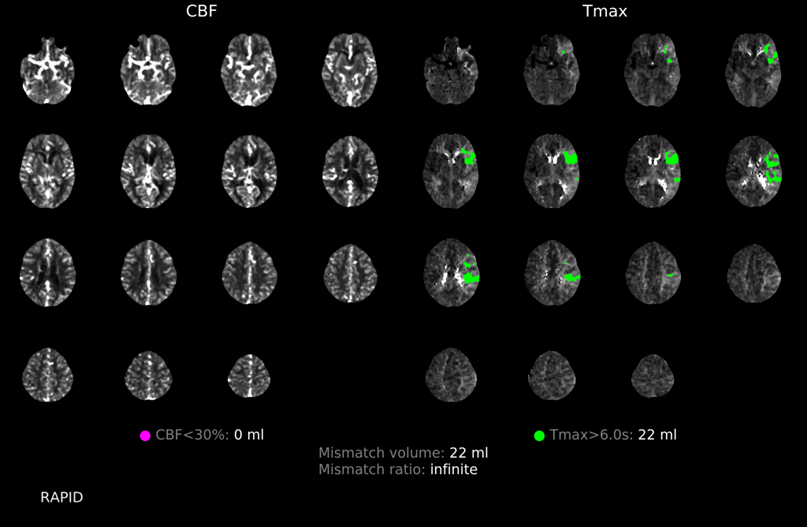
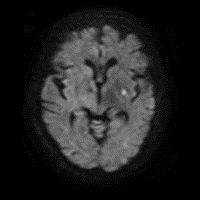
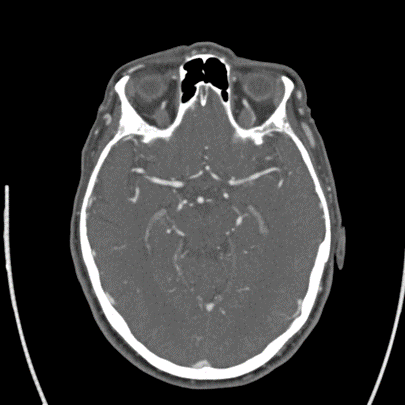
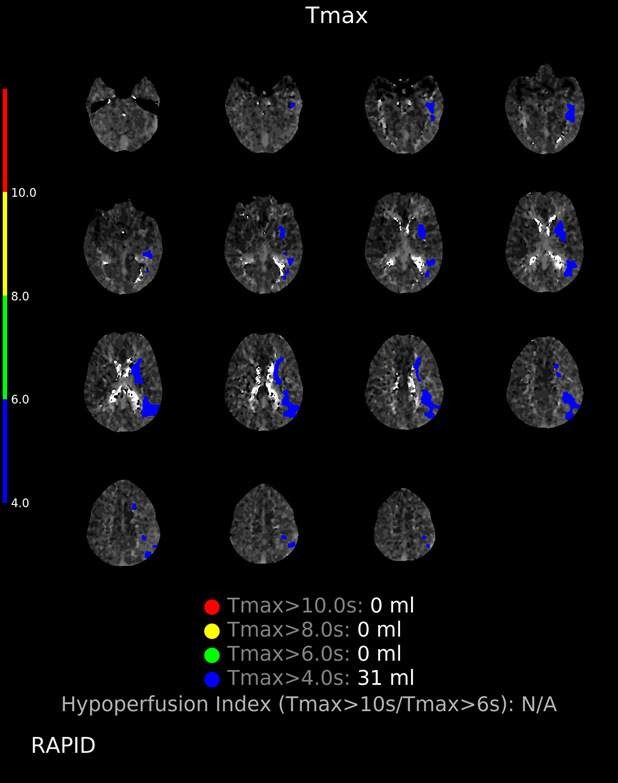
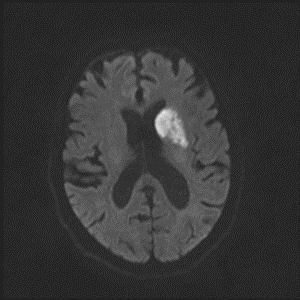
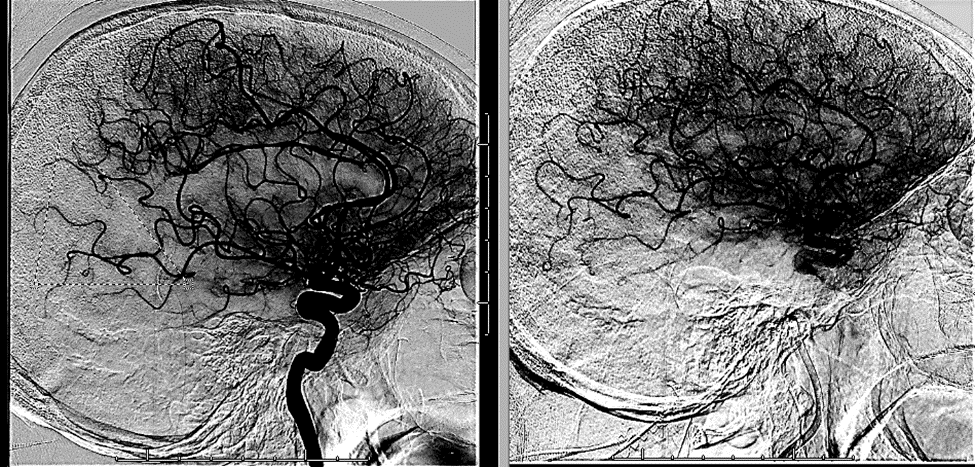
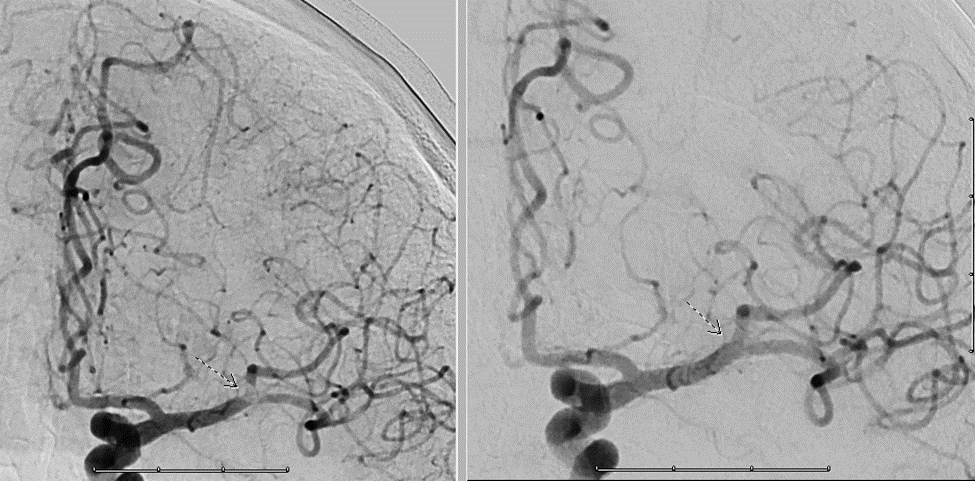
15/ The patient is kept in the ICU and ultimately undergoes #angiogram. Notice the area of perfusional deficit along the posterior MCA division:
16/ With some mild suction, @sudhakar_satti is able to suction a rubbery clot and the MCA looks much better post-procedure 😎
18/ What is the etiology of this lesion?
20/ Take 🏡 points:
👉 Recurrent events with no EEG correlate and with prolonged TMax make us think it was perfusional
👉 Stent placement in acute setting associated with hemorrhagic conversion – delay x 1-2 weeks is prudent
👉 Recurrent events with no EEG correlate and with prolonged TMax make us think it was perfusional
👉 Stent placement in acute setting associated with hemorrhagic conversion – delay x 1-2 weeks is prudent
21/ 👉 No matter how long you practice, patients will always surprise you!
👉 It takes a village to care for our patients!
👉 It takes a village to care for our patients!
22/ Other ideas? Comments? I'd love to hear from you! @caseyalbin @JimmySuhMD @JimSiegler @MicieliA_MD @a_charidimou @EricLawson90 @CajalButterfly @Capt_Ammonia @DrAtulRamesh1 @RamaniBalu1 @DSandsmarkMDPhD @PennNeurology @TJUHNeuroCrit @namorrismd
Loading suggestions...