Management of Mechanical Prosthetic Heart Valve Thrombosis: @JACCJournals Review Topic of the Week
Fabulous review from the Washington Hospital Center Team...It is dense, but will try to break it down:
👇👇👇
Fabulous review from the Washington Hospital Center Team...It is dense, but will try to break it down:
👇👇👇
1/ 🏥🔄❤️ Mechanical heart valves are durable, outlasting bioprostheses. But, they're more thrombogenic & require lifelong anticoagulation.
2/ 🚧🔄❤️ Mechanical Valve (MV) dysfunction can be caused by 4 phenomena:
🥸thrombosis,
🥸pannus ingrowth,
🥸degeneration,
🥸endocarditis.
It's imp to identify the leading cause for appropriate treatment.
🥸thrombosis,
🥸pannus ingrowth,
🥸degeneration,
🥸endocarditis.
It's imp to identify the leading cause for appropriate treatment.
3/ 🔄❤️🤔 Sometimes, these issues occur simultaneously, making the diagnosis more complex.
Correctly identifying the predominant cause is imp for effective Mx. 🩺
💡#CardioTwitter
Correctly identifying the predominant cause is imp for effective Mx. 🩺
💡#CardioTwitter
4/ ⚠️🔄❤️ Mechanical valve thrombosis (MVT) symptoms can vary widely - from unnoticed findings on imaging to life-threatening cardiogenic shock or massive stroke.
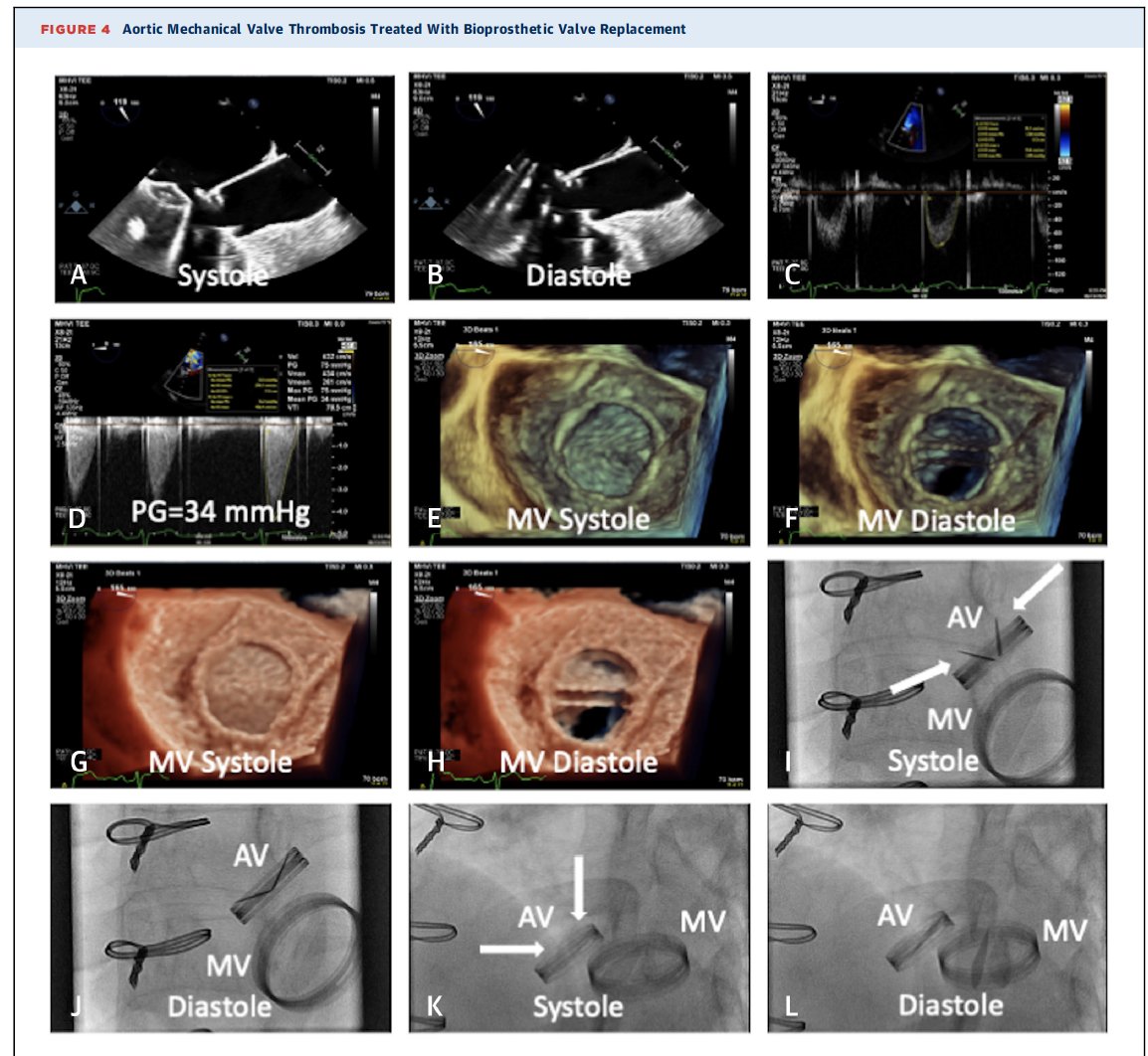
5/ 📊🔄❤️ Diagnosing MVT involves several imaging modalities, which help in confirming the condition.
6/ 💉🔧🔄❤️ Treatment options for obstructive MVT include
🥸surgery,
🥸heparin/anticoagulation
🥸thrombolysis, and
🥸transcatheter interventional techniques.
See below - will break it down under management.
🥸surgery,
🥸heparin/anticoagulation
🥸thrombolysis, and
🥸transcatheter interventional techniques.
See below - will break it down under management.
7/ 🔄❤️👨⚕️ The choice of treatment for MVT is influenced by:
🥸degree of obstruction,
🥸valve location,
🥸patient's stability, surgical risk, and
🥸local expertise.
🥸degree of obstruction,
🥸valve location,
🥸patient's stability, surgical risk, and
🥸local expertise.
8/ 📈🔄❤️ The estimated yearly rate of MVT ranges from 0.1% to 5.7%. Certain valve designs, recent implantation, and mitral or tricuspid valve location are associated with higher rates.
9/ 🔄❤️👩⚕️ Routine imaging of mechanical valves isn't typically done after an initial post-implantation echocardiogram.
Current ACC/AHA guidelines only recommend further imaging if there are clinical signs of valve dysfunction.
Current ACC/AHA guidelines only recommend further imaging if there are clinical signs of valve dysfunction.
10/ 🔄❤️🔧 Mechanical valves historically come in three designs:
🥸caged-ball,
🥸tilting disk, and
🥸bileaflet valves.
While bileaflet is the modern standard, older designs are still found in older patients, carrying higher thrombotic risks.
🥸caged-ball,
🥸tilting disk, and
🥸bileaflet valves.
While bileaflet is the modern standard, older designs are still found in older patients, carrying higher thrombotic risks.
11/ 🔄❤️🧪 Areas of stagnation and blood flow disturbance in the valve can trigger thrombus formation, tissue overgrowth, and calcification.
High shear stress may lead to blood cell damage and platelet activation.
High shear stress may lead to blood cell damage and platelet activation.
12/ 🔄❤️🏥 Symptoms of MVT vary widely, depending largely on the acuity and degree of resulting valvular obstruction or regurgitation.
🥸Obstructive MVT often manifests as heart failure or cardiogenic shock, particularly if diagnosis is delayed.
🥸Obstructive MVT often manifests as heart failure or cardiogenic shock, particularly if diagnosis is delayed.
13/ 🔄❤️🔬 Some common causes for MV dysfunction include poor anticoagulation adherence, early dysfunction due to surgical complications or infection, and late dysfunction related to prosthesis type, thrombogenicity, and patient-related factors.
14/ 🔄❤️👨⚕️ During physical examination, absent valve clicking, a new murmur, signs of pulmonary edema, heart failure, and symptoms of pulmonary or systemic thromboembolism may be noticed.
🥸Acute ischemic strokes are a common complication.
Call @RezaEmaminia & image first
🥸Acute ischemic strokes are a common complication.
Call @RezaEmaminia & image first
15/ 📸 MULTIMODALITY IMAGING: 🔍 The diagnosis and management of Mechanical Valve Thrombosis (MVT) often necessitate a multimodality imaging approach.
Use multimodalities to address:
🥸etiology
🥸location
🥸severity
🥸hemodynamic changes associated with MVT
Use multimodalities to address:
🥸etiology
🥸location
🥸severity
🥸hemodynamic changes associated with MVT
16/ 🎯 Relevant findings include:
🥸increased valvular gradients
🥸impaired mobility,
🥸regurgitation
🥸visualization of thrombus.
TTE and cinefluoroscopy are common, but TEE and cardiac CT also come into play.
🥸increased valvular gradients
🥸impaired mobility,
🥸regurgitation
🥸visualization of thrombus.
TTE and cinefluoroscopy are common, but TEE and cardiac CT also come into play.
17/ ❤️ ECHOCARDIOGRAPHY: Both 2D and 3D echocardiography focus on valve appearance, leaflet mobility, and presence of thrombus. Mitral mechanical valves can be viewed as echogenic structures with varying shadowing artifact, depending on the valve position and imaging plane.
18/ 🔬 Thrombus identification depends on size and location; shadowing artifact is a major limitation.
🥸Deviations from expected opening/closing angles of MVs, predetermined by the manufacturer, may also be observed.
🥸Deviations from expected opening/closing angles of MVs, predetermined by the manufacturer, may also be observed.
19/ 🌊 Color Doppler assesses valve obstruction, manifesting as elevated blood velocity and flow acceleration.
🥸Lack of or limited flow visualization across the valve is an indicator of leaflet restriction and probable thrombosis.
🥸Lack of or limited flow visualization across the valve is an indicator of leaflet restriction and probable thrombosis.
20/ 📉 Abnormal regurgitation may occur with inadequate valve closure, either transvalvular or paravalvular.
🥸Differentiating between the two is important as it informs the potential cause of valve dysfunction and therapeutic options.
🥸Differentiating between the two is important as it informs the potential cause of valve dysfunction and therapeutic options.
21/ 💉 Spectral Doppler aids in determining the transvalvular gradient across a prosthetic valve.
🥸Influenced by multiple factors, including the size of the effective orifice area (EOA), blood volume, and the increment of time in which the blood is displaced.
🥸Influenced by multiple factors, including the size of the effective orifice area (EOA), blood volume, and the increment of time in which the blood is displaced.
22/ 🤔 Differentiating between THROMBUS and PANNUS is imp to ascertain as thrombolytic therapy can be used for the former but is contraindicated in the latter.
🥸Pathological analysis of a surgically explanted valve remains the gold standard.
🥸Pathological analysis of a surgically explanted valve remains the gold standard.
23/ 🎥 CINE-FLUOROSCOPY is noninvasive method that can assess MV leaflet motion, especially when TTE visualization of the valve is suboptimal or inconclusive.
24/ 🧲CARDIAC CT AND MAGNETIC RESONANCE can provide additional insights when echocardiography or cine-fluoroscopy are inconclusive.
🥸Attenuation values can help differentiate thrombus from pannus. However, MV artifacts can affect image quality: improved w intravenous contrast
🥸Attenuation values can help differentiate thrombus from pannus. However, MV artifacts can affect image quality: improved w intravenous contrast
25/ MANAGEMENT 📚
NONOBSTRUCTIVE VS OBSTRUCTIVE THROMBUS ⚖️
🥸Anticoagulation in small, nonobstructive thrombi (<5 mm)
🥸Larger thrombi (>5 mm) have a higher risk of embolization
🥸Optimization of anticoagulation and repeat imaging
NONOBSTRUCTIVE VS OBSTRUCTIVE THROMBUS ⚖️
🥸Anticoagulation in small, nonobstructive thrombi (<5 mm)
🥸Larger thrombi (>5 mm) have a higher risk of embolization
🥸Optimization of anticoagulation and repeat imaging
26/ For obstructive MVT:
🥸Anticoagulation
🥸Thrombolysis
🥸Transcatheter manipulation
🥸Surgery
🥸Anticoagulation
🥸Thrombolysis
🥸Transcatheter manipulation
🥸Surgery
27/ ANTICOAGULATION 💊
Anticoagulation options:
🥸Oral anticoagulation with warfarin
🥸Parenteral heparinoid agents
🥸Treatment with unfractionated heparin (UFH) plus warfarin reported successful.
🥸A higher INR (>3.0) reduced the incidence of thromboembolism.
Anticoagulation options:
🥸Oral anticoagulation with warfarin
🥸Parenteral heparinoid agents
🥸Treatment with unfractionated heparin (UFH) plus warfarin reported successful.
🥸A higher INR (>3.0) reduced the incidence of thromboembolism.
28/ LMWH, compared to UFH, has several advantages:
🥸Less thrombocytopenia
🥸Lower bleeding risk
🥸More predictable pharmacokinetics
🥸Lower hospital stay
---
🥸There have been reports of complications with LMWH.
🥸DOAC are presently contraindicated for use with MVs.
🥸Less thrombocytopenia
🥸Lower bleeding risk
🥸More predictable pharmacokinetics
🥸Lower hospital stay
---
🥸There have been reports of complications with LMWH.
🥸DOAC are presently contraindicated for use with MVs.
29/ THROMBOLYSIS 🧪
Several trials have explored thrombolytic therapy with varying results.
Important contraindications include:
🥸Left atrial thrombus
🥸Recent ischemic stroke
🥸Hemorrhagic stroke history
🥸Bleeding diathesis
Several trials have explored thrombolytic therapy with varying results.
Important contraindications include:
🥸Left atrial thrombus
🥸Recent ischemic stroke
🥸Hemorrhagic stroke history
🥸Bleeding diathesis
30/ TRANSCATHETER INTERVENTIONS 🚑
Transcatheter interventions for stuck MV leaflets has emerged as an option for those who fail thrombolysis, present with cardiogenic shock, or have a high risk for redo surgery.
Transcatheter interventions for stuck MV leaflets has emerged as an option for those who fail thrombolysis, present with cardiogenic shock, or have a high risk for redo surgery.
31/ REDO SURGERY 🏥
🥸An advantage of surgery is definitive diagnosis and treatment in cases of unclear etiology.
🥸Patients treated with thrombolytic therapy, compared with surgery, had a lower rate of major and minor complications and a lower 3-month mortality.
🥸An advantage of surgery is definitive diagnosis and treatment in cases of unclear etiology.
🥸Patients treated with thrombolytic therapy, compared with surgery, had a lower rate of major and minor complications and a lower 3-month mortality.
32/ Fresh thrombus is more likely to respond to thrombolytics or transcatheter release, whereas mature, organized thrombus is more likely to require surgery.
🥸When redo surgery is pursued for MVT, the valve must be replaced and not simply declotted.
🥸When redo surgery is pursued for MVT, the valve must be replaced and not simply declotted.
34/ CONCLUSIONS 😷🏥
🥸Prosthetic valve thrombosis is a known MV complication.⚠️❗️
🥸clinicians must keep a high index of suspicion for MVT in patients who present with signs and symptoms of heart failure or cardiogenic shock.
👀💔🚨
🥸Prosthetic valve thrombosis is a known MV complication.⚠️❗️
🥸clinicians must keep a high index of suspicion for MVT in patients who present with signs and symptoms of heart failure or cardiogenic shock.
👀💔🚨
35/ Multimodality imaging with echocardiography, cinefluoroscopy, and CT is critical for prompt diagnosis and to guide management. 📊🔬💡
36/ and LAST tweet (so sorry)
🥸The optimal strategy—anticoagulation, thrombolysis, transcatheter intervention, or redo surgery—depends on the degree of obstruction and the patient’s hemodynamic status on presentation.
I learned a lot from this guy 🥸 - thank you for reading!
🥸The optimal strategy—anticoagulation, thrombolysis, transcatheter intervention, or redo surgery—depends on the degree of obstruction and the patient’s hemodynamic status on presentation.
I learned a lot from this guy 🥸 - thank you for reading!
Loading suggestions...