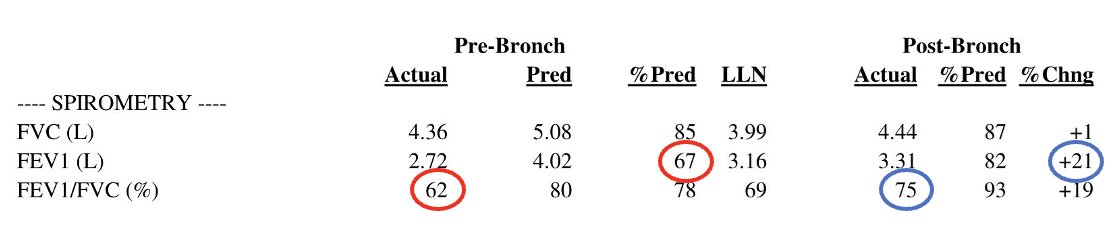
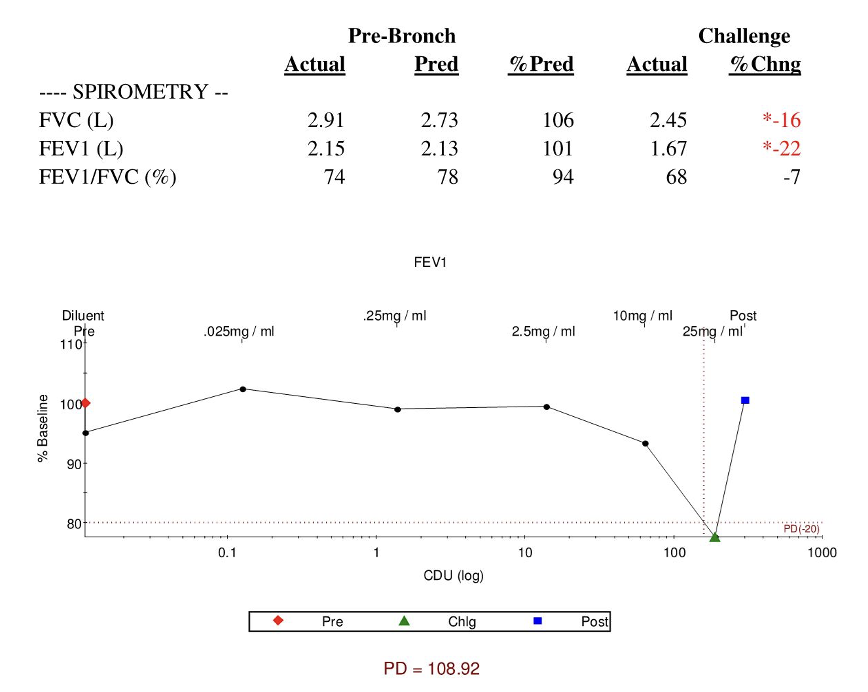
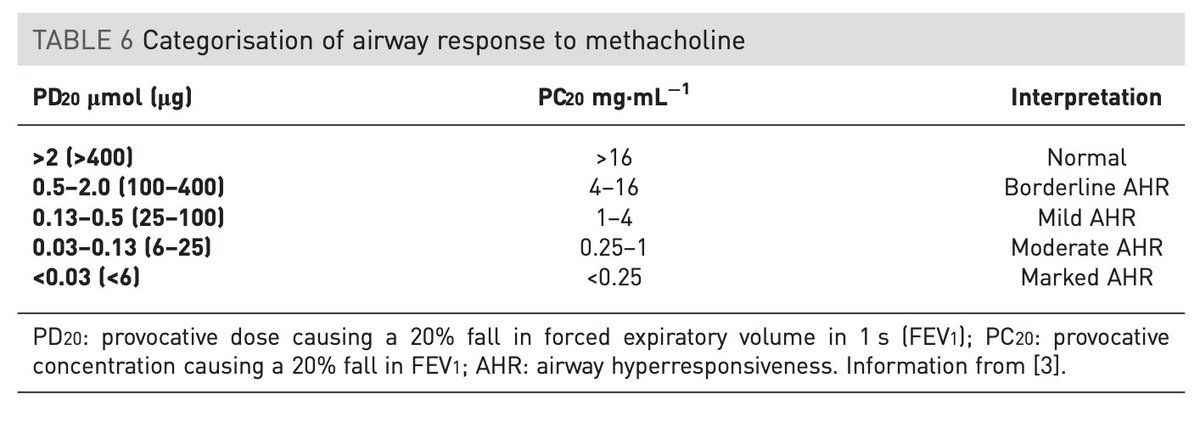
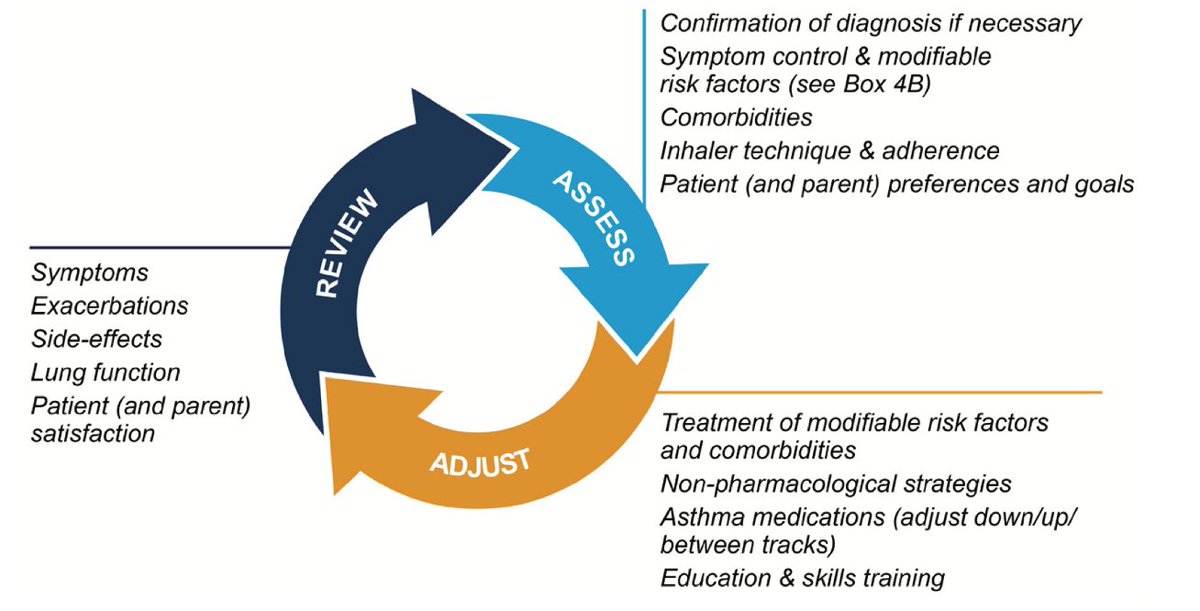
Asthma is characterized by chronic airway inflammation, VARIABLE symptoms, and VARIABLE airflow limitation/airway hyperresponsiveness.
It is a clinical diagnosis, not a spirometric one as spiro findings are “not necessary or sufficient to make the diagnosis.”
It is a clinical diagnosis, not a spirometric one as spiro findings are “not necessary or sufficient to make the diagnosis.”
For a primer on obstruction (airflow limitation), start here with the beginning of this thread on COPD.
Now this emphasis on VARIABLE symptoms and VARIABLE airflow limitation can make asthma tricky to diagnose.
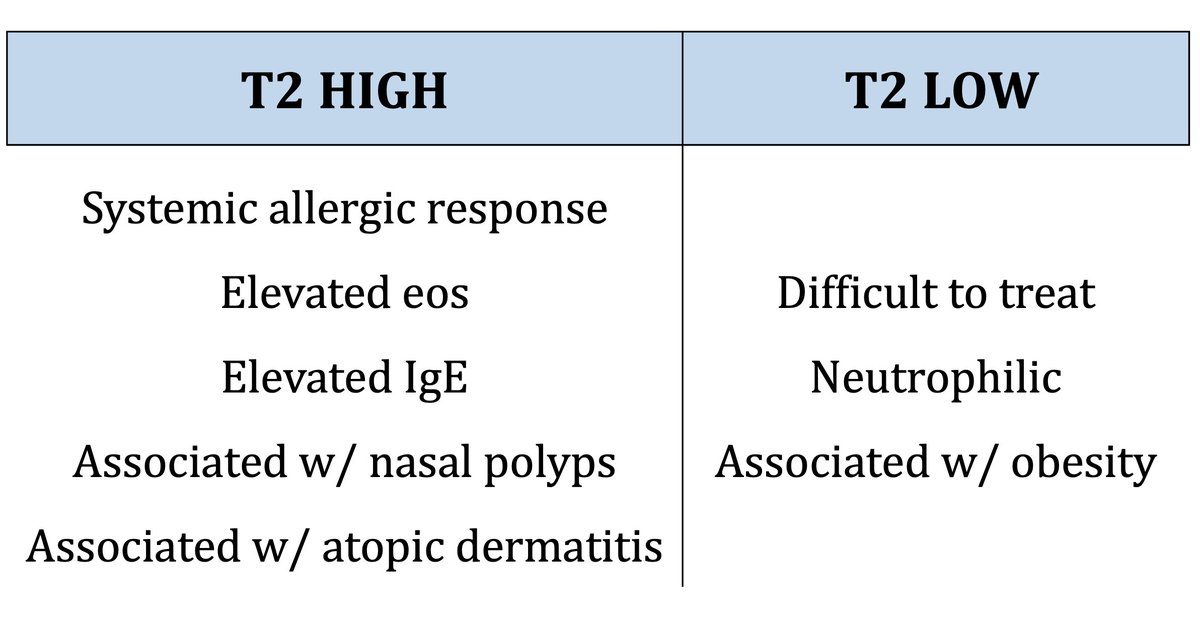
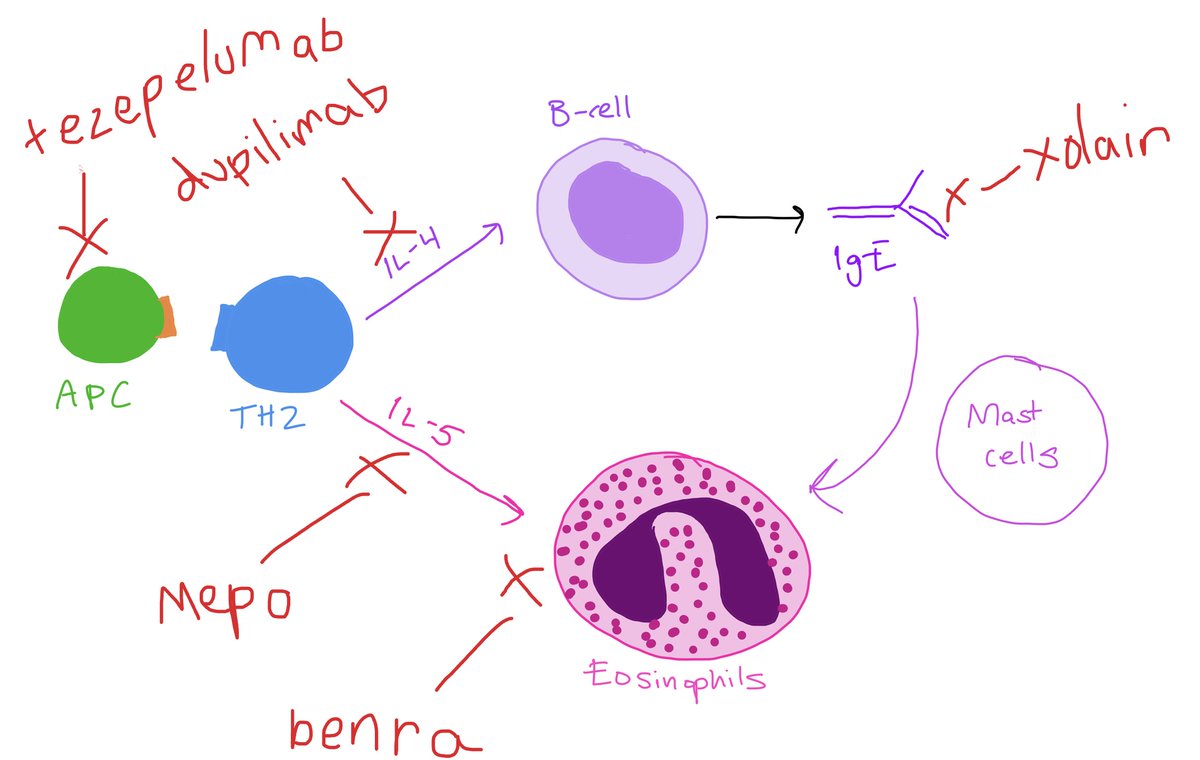
Whereas an initial COPD history can sometimes feel straightforward, an asthma history requires a lot of digging: family history, childhood history, environmental allergies, eczema, GERD, nasal polyps, sinus history, NSAIDs, triggers, etc.
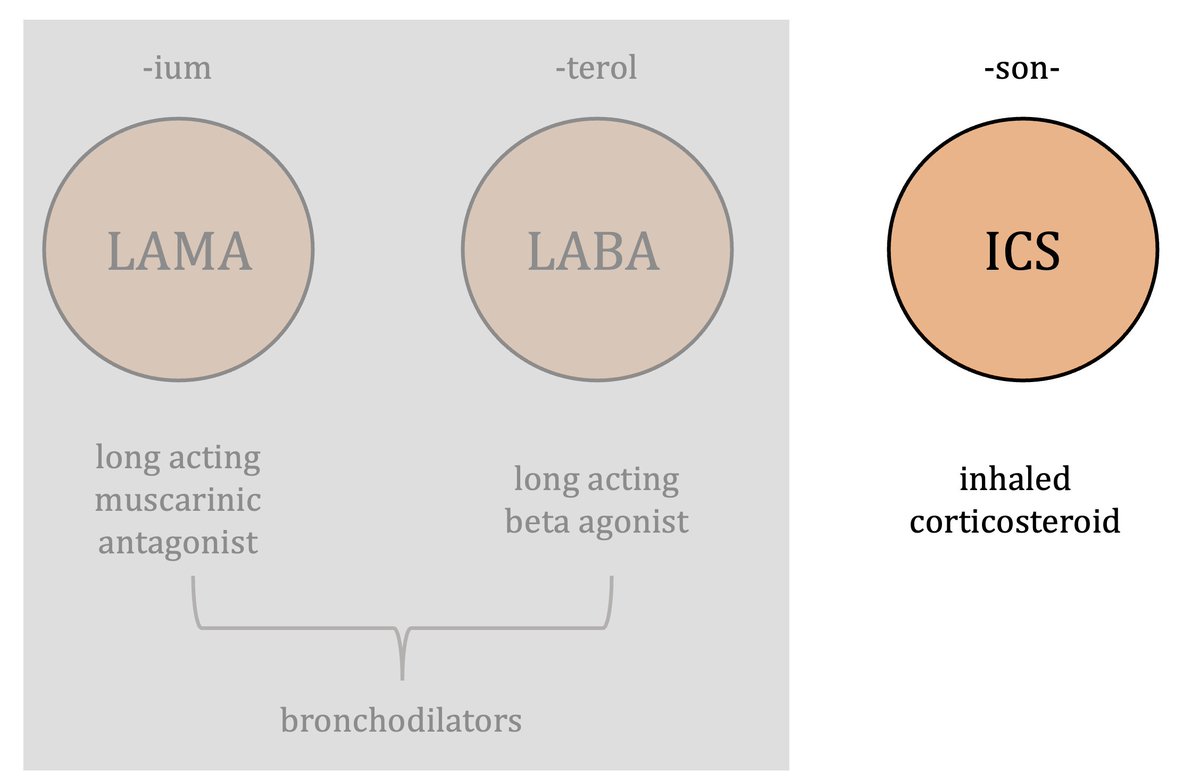
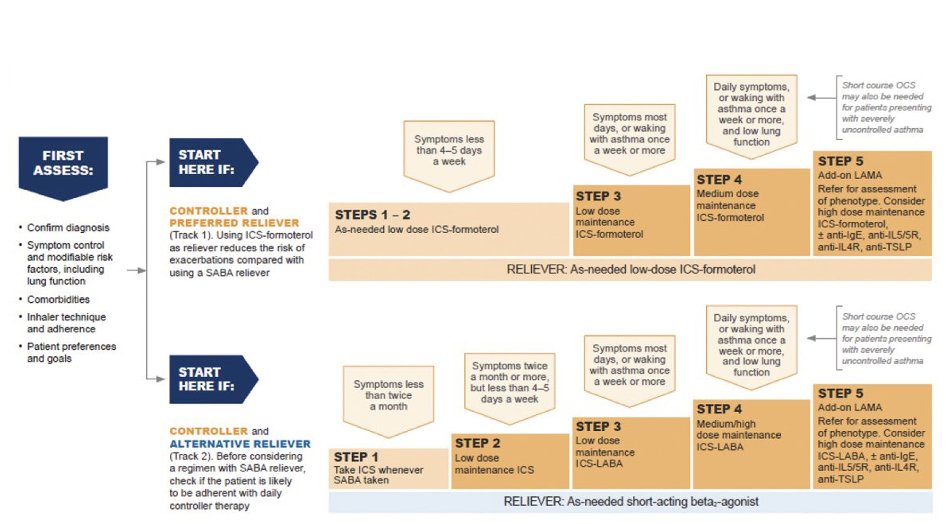
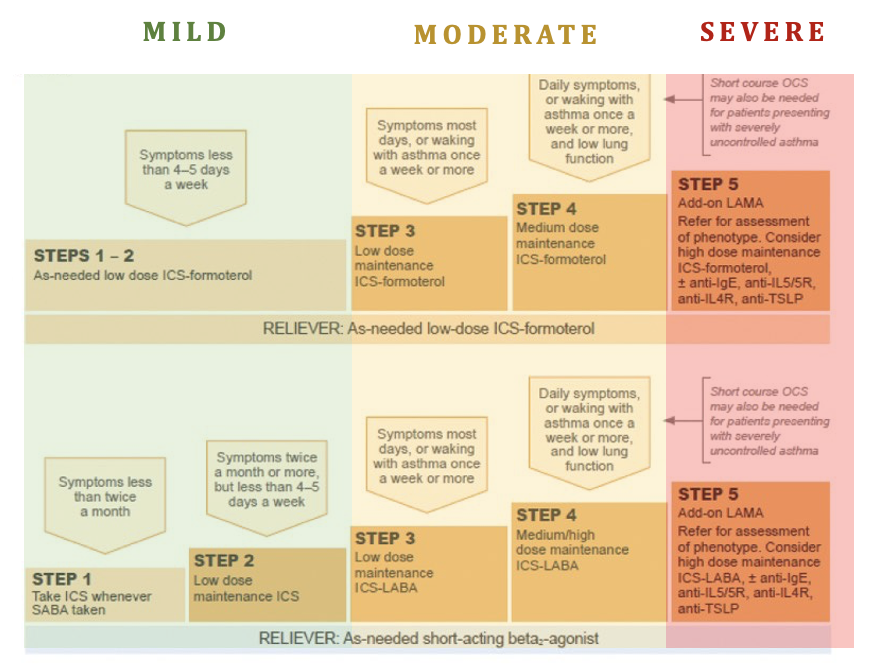
🚨KEY POINT: NO ONE with asthma should be on just a bronchodilator!
Every patient with a diagnosis of asthma should be getting an inhaled steroid, whether daily or just PRN (steps 1-2).
SABA alone increases risk of severe exacerbation/hospitalization compared with LABA/ICS.
Every patient with a diagnosis of asthma should be getting an inhaled steroid, whether daily or just PRN (steps 1-2).
SABA alone increases risk of severe exacerbation/hospitalization compared with LABA/ICS.
Notice that the different steps involve different doses of ICS. This means you have to know which ICS and how much you’re using. The # of puffs for these inhalers matter.
This chart from @pyrlsapp is a thing of beauty. Use it to ensure you're RXing what you say you're RXing.
This chart from @pyrlsapp is a thing of beauty. Use it to ensure you're RXing what you say you're RXing.
Asthma can be tricky to diagnose and tricky to manage, but if you are attentive and thorough (and you make sure they’re on an ICS) you can make a big difference in quality of life for your asthma patients (26 million in the US)!
Loading suggestions...