2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: @JACCJournals
Guidelines are detailed: reading it slowly.
Please, read full doc!
Thread #10:
Lipid management and chronic coronary disease?
🥸
Guidelines are detailed: reading it slowly.
Please, read full doc!
Thread #10:
Lipid management and chronic coronary disease?
🥸
2. 🥸 For those where high-intensity statin therapy isn't suitable, moderate-intensity therapy is recommended for a 30% to 49% reduction in LDL-C levels to reduce MACE risk.
3. 🥸 In CCD patients, adherence and effects of medication should be assessed by measuring fasting lipids in 4 to 12 weeks after statin initiation or adjustment, then every 3 to 12 months.
4. 🥸 The use of generic formulations of maximally tolerated statin therapy in CCD patients is projected to be cost-saving.
6. 🥸 The addition of generic ezetimibe to maximally tolerated statin therapy in selected CCD patients is projected to be of high economic value at US prices.
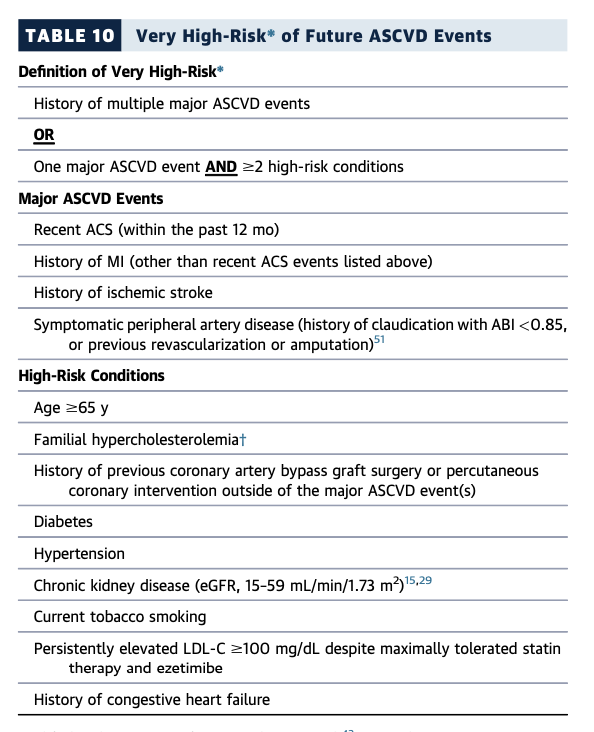
7. 🥸 In very high-risk CCD patients with an LDL-C level >=70 mg/dL or non-HDL-C level >=100 mg/dL on statin and ezetimibe, a PCSK9 monoclonal antibody can reduce MACE risk.
This is 2a!
This is 2a!
8. 🥸 The use of PCSK9 monoclonal antibodies in very high-risk CCD patients is projected to be of uncertain economic value at US prices.
*** Uncertainty should be address :)
*** Uncertainty should be address :)
9. 🥸 In CCD patients with LDL-C <100 mg/dL and persistent fasting triglyceride level of 150 to 499 mg/dL, icosapent ethyl may reduce the risk of MACE and cardiovascular death.
👇👇👇
accessdata.fda.gov
👇👇👇
accessdata.fda.gov
10. 🥸 In CCD patients not at very high risk and with LDL-C >70 mg/dL on statin therapy, adding ezetimibe may further reduce MACE risk.
This is 2b
This is 2b
11. 🥸 If ezetimibe and PCSK9 monoclonal antibody are insufficient in CCD patients with LDL-C >=70 mg/dL, adding bempedoic acid or inclisiran may further reduce LDL-C levels.
👇👇👇
nejm.org
jamanetwork.com
nejm.org
👇👇👇
nejm.org
jamanetwork.com
nejm.org

nejm.org/doi/10.1056/NE…
Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol | NEJM
Original Article from The New England Journal of Medicine — Two Phase 3 Trials of Inclisiran in Pati...

nejm.org/doi/10.1056/NE…
Safety and Efficacy of Bempedoic Acid to Reduce LDL Cholesterol | NEJM
Original Article from The New England Journal of Medicine — Safety and Efficacy of Bempedoic Acid to...
jamanetwork.com/journals/jama/…
Effect of Bempedoic Acid vs Placebo Added to Statins on LDL-C in Patients at High Risk for CVD
This randomized clinical trial compares the efficacy of bempedoic acid, an experimental drug that in...
12. 🥸 In CCD patients on statin therapy, adding niacin, fenofibrate, or omega-3 fatty acids are not beneficial in reducing cardiovascular risk.
*** So, these are class III no harm! 😱
*** So, these are class III no harm! 😱
13🥸: LDL-C is identified as a main cause of atherosclerotic disease and a key target of lipid management. It's central to heart health.
14.🥸 Several RCTs established the efficacy & safety of high-intensity statin therapy to reduce LDL-C levels by >50% and reduce MACE risk
15🥸: Despite maximally tolerated statin therapy, residual cardiovascular risk persists, especially among patients with CCD and high-risk factors.
*** See list above.
*** See list above.
16. 🥸: Other non statins didn't same benefit; but ezetimibe, PCSK9 monoclonal antibodies & icosapent ethyl reduce cardiovascular risk with statin therapy.
17.🥸: New drugs are available; clinicians should prioritize ezetimibe & PCSK9 antibodies when extra LDL-C lowering is necessary in CCD patients.
18🥸: Regular lipid monitoring is necessary to assess individual response to lipid-lowering therapy and keep track of adherence over time.
20🥸: High-intensity statin therapy may not be for all; if intolerant, a moderate-intensity statin may be used. Clinicians may consider alternatives.
21.🥸: The goal for LDL-C lowering is defined by % responses relative to baseline. Individual response can vary; serial monitoring is critical.
22.🥸: Economic value of lipid-lowering depends on the absolute benefit and cost. Use of generic statins in the US is projected to be cost-saving.
23.🥸: In IMPROVE-IT, adding ezetimibe to moderate-intensity statin among patients with ACS reduced ASCVD risk. Generic ezetimibe is high value.
24.🥸: The FOURIER & ODYSSEY trials showed efficacy of alirocumab & evolocumab. US cost of PCSK9 antibodies has declined by 60% since entry.
😱😱😱: From approximately $14,000 per year to $5,850 per year.
😱😱😱: From approximately $14,000 per year to $5,850 per year.
25. 🥸: Cost-effectiveness of PCSK9 inhibitors depends on many factors. They may be intermediate value in patients at higher risk, low in others.
26🥸 REDUCE-IT trial randomized patients to icosapent ethyl or placebo. Significant 25% reduction in MACE, 20% in cardiovascular death.
***Benefit driven by higher EPA levels, not triglyceride reduction of 17%.
***Benefit driven by higher EPA levels, not triglyceride reduction of 17%.
27🥸 RESPECT-EPA showed a borderline reduction in MACE with icosapent ethyl in Japan on background statin therapy. Limited by lack of placebo control, under-powered.
28🥸 STRENGTH trial found no benefit with omega-3 fatty acids (EPA and DHA) vs. corn oil placebo.
29🥸 Unclear if further LDL-C lowering or adding icosapent ethyl is more effective for LDL-C between 70-100 mg/dL. Consider patient preference, secondary causes of elevated triglycerides.
30.🥸 Bempedoic acid, a first-in-class therapy, reduces LDL-C by 15-25%. Combined with ezetimibe, it may reduce LDL-C by 35%. Caution with simvastatin >20 mg or pravastatin 40 mg.
31. 🥸 Dietary supplements with omega-3 fatty acids are not recommended for MACE reduction in CCD. Only icosapent ethyl (EPA only) may be beneficial. Trials like AIM-HIGH found no benefit with niacin.
32/🥸 ACCORD-LIPID found no benefit with fenofibrate in background statin therapy, even in CVD patients. Pemafibrate in PROMINENT trial stopped early for futility. Fenofibrate only for severe hypertriglyceridemia.
Ending here - sorry, it was long, but I did not want to break it in smaller threads.
All lipids are in one chapter/thread.
Next Thread #11 is BP Mx.
🥸🥸: thank you for reading :)
All lipids are in one chapter/thread.
Next Thread #11 is BP Mx.
🥸🥸: thank you for reading :)
Loading suggestions...