1/
A 68 yo woman collapses at a Braves game. Bystander CPR is initiated. AED demonstrates a shockable rhythm, ROSC is achieved after 6 rounds of CPR. She’s found to have a STEMI and the LAD is stented.
4 days after arrest she is in coma. MRI is completed.
A #continuumcase
A 68 yo woman collapses at a Braves game. Bystander CPR is initiated. AED demonstrates a shockable rhythm, ROSC is achieved after 6 rounds of CPR. She’s found to have a STEMI and the LAD is stented.
4 days after arrest she is in coma. MRI is completed.
A #continuumcase
2/
Much has been written about TTM and neuroprognostication.
TTM is not the focus of this thread, but vibe check – what temp are you targeting?
Much has been written about TTM and neuroprognostication.
TTM is not the focus of this thread, but vibe check – what temp are you targeting?
3/
My favorite review of the history and evidence of TTM is here.
@PulmCrit
emcrit.org
Highly suggested reading for anyone seeing these patients in consultation or as the primary team.
My favorite review of the history and evidence of TTM is here.
@PulmCrit
emcrit.org
Highly suggested reading for anyone seeing these patients in consultation or as the primary team.
5/
Ischemic damage is most notable in areas with high metabolic demands:
🧠CA1 neurons in the hippocampus
🧠Cerebellar purkinje cells
🧠Thalamic reticular neurons
🧠Striatal neurons
🧠Pyramidal neurons in the neocortex
Ischemic damage is most notable in areas with high metabolic demands:
🧠CA1 neurons in the hippocampus
🧠Cerebellar purkinje cells
🧠Thalamic reticular neurons
🧠Striatal neurons
🧠Pyramidal neurons in the neocortex
8/
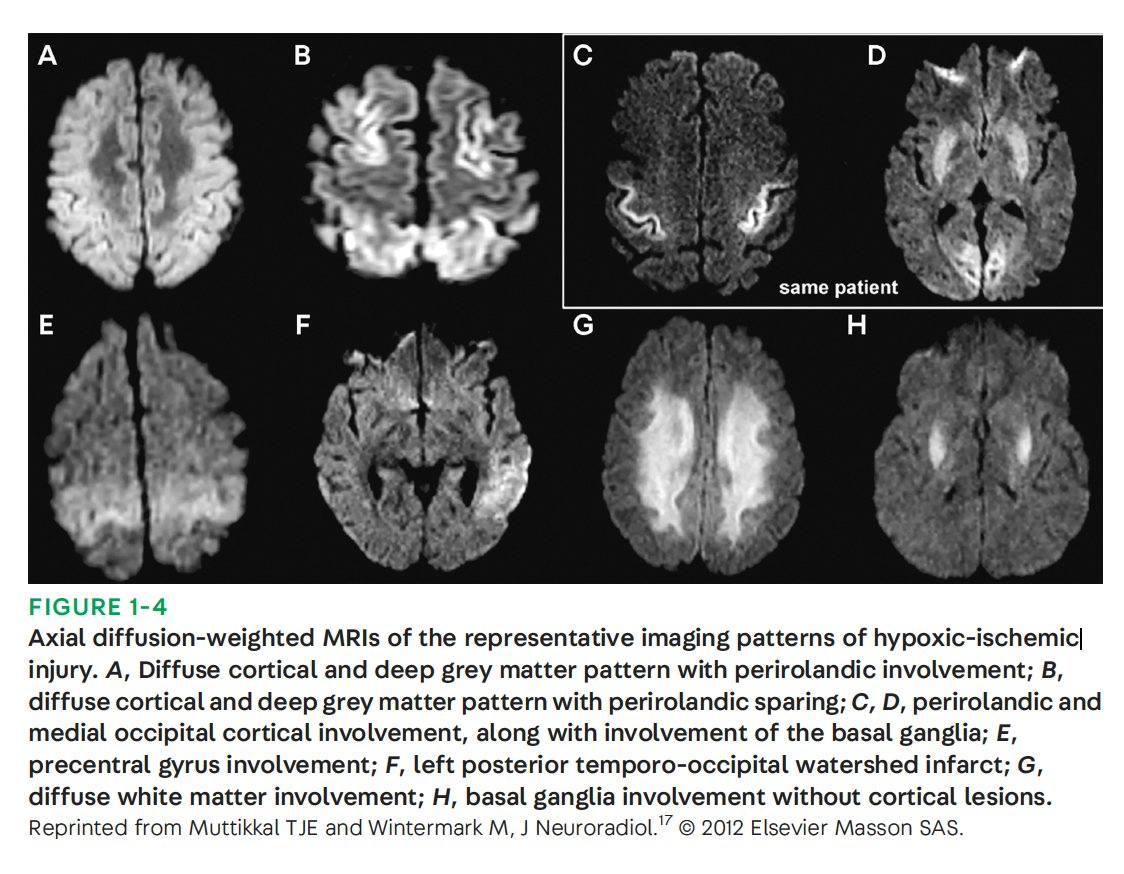
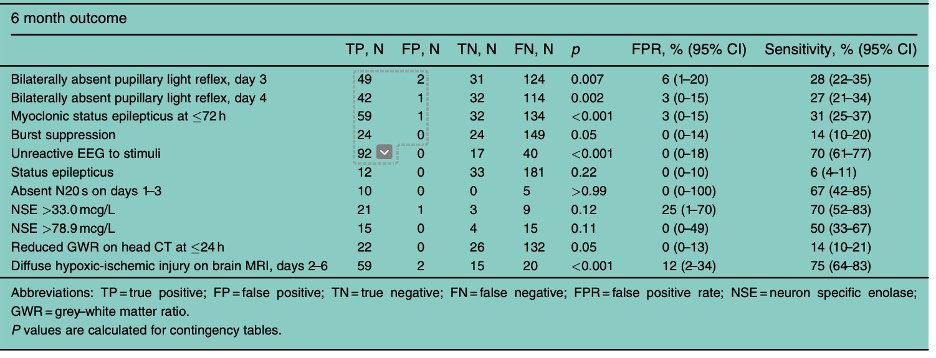
ESICM and AHA discuss “*diffuse* hypoxic-ischemic injury on brain MRI” (AHA specifies done on day 2-6).
However a single-center assessment of patients with this pattern found that 2 patients (of 62) still had a “good” outcome (CPC 1-2).
pubmed.ncbi.nlm.nih.gov
ESICM and AHA discuss “*diffuse* hypoxic-ischemic injury on brain MRI” (AHA specifies done on day 2-6).
However a single-center assessment of patients with this pattern found that 2 patients (of 62) still had a “good” outcome (CPC 1-2).
pubmed.ncbi.nlm.nih.gov
9/
This results in a False Positive Rate of 12% (95 CI 2-34)
This center allowed WLST due to perceived poor neurologic outcome, meaning this FPR is a best case scenario and may underestimate the true FPR.
pubmed.ncbi.nlm.nih.gov
This results in a False Positive Rate of 12% (95 CI 2-34)
This center allowed WLST due to perceived poor neurologic outcome, meaning this FPR is a best case scenario and may underestimate the true FPR.
pubmed.ncbi.nlm.nih.gov
10/
Look at the first scan... I know you can't see the whole thing, but would this count as "diffuse?"
Look at the first scan... I know you can't see the whole thing, but would this count as "diffuse?"
11/
Lol, I know. you need more info. But I think it should emphasize just how objective a measurement "diffuse" is.
Lol, I know. you need more info. But I think it should emphasize just how objective a measurement "diffuse" is.
10/
So. Room for improvement.
One way may be in assessing the minimum or mean ADC for regional or global aspect of the scan.
This would make MRI grading more objective, and may better differentiate pts that could have good outcomes from those w/ poor
sciencedirect.com
So. Room for improvement.
One way may be in assessing the minimum or mean ADC for regional or global aspect of the scan.
This would make MRI grading more objective, and may better differentiate pts that could have good outcomes from those w/ poor
sciencedirect.com
12/
Neuroprognostication is hard. the more information and the more time you give the better.
The neurologic complications of cardiopulmonary disease is a fascinating and rapidly evolving.
For an up to date review:
journals.lww.com
Neuroprognostication is hard. the more information and the more time you give the better.
The neurologic complications of cardiopulmonary disease is a fascinating and rapidly evolving.
For an up to date review:
journals.lww.com
Loading suggestions...