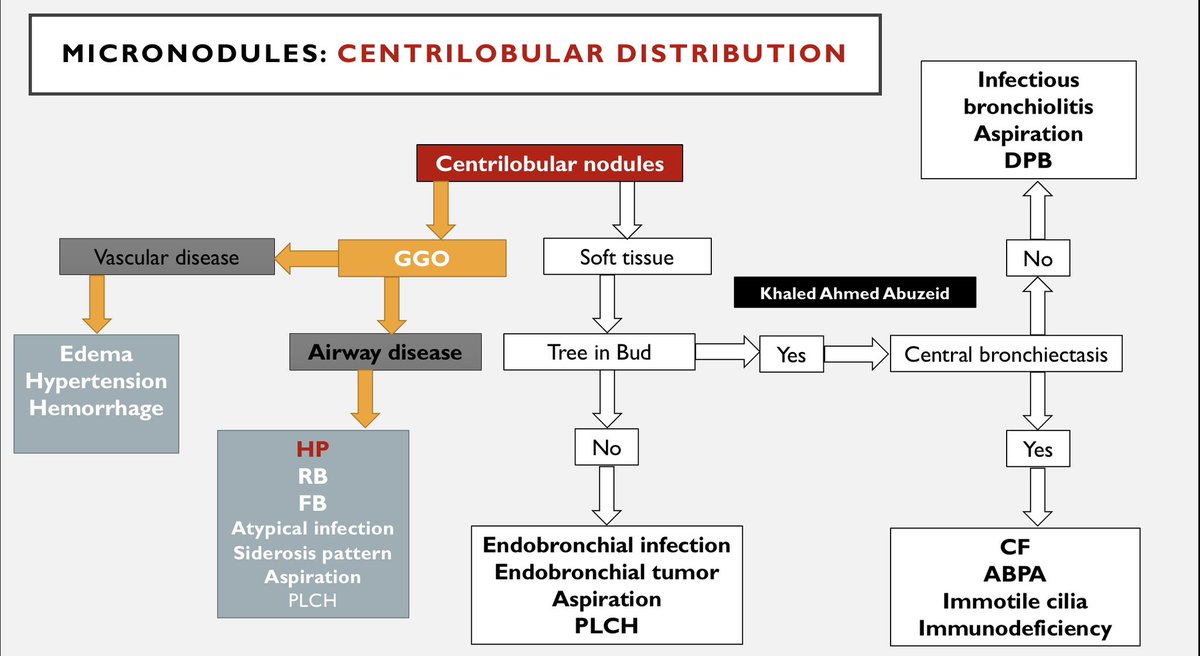
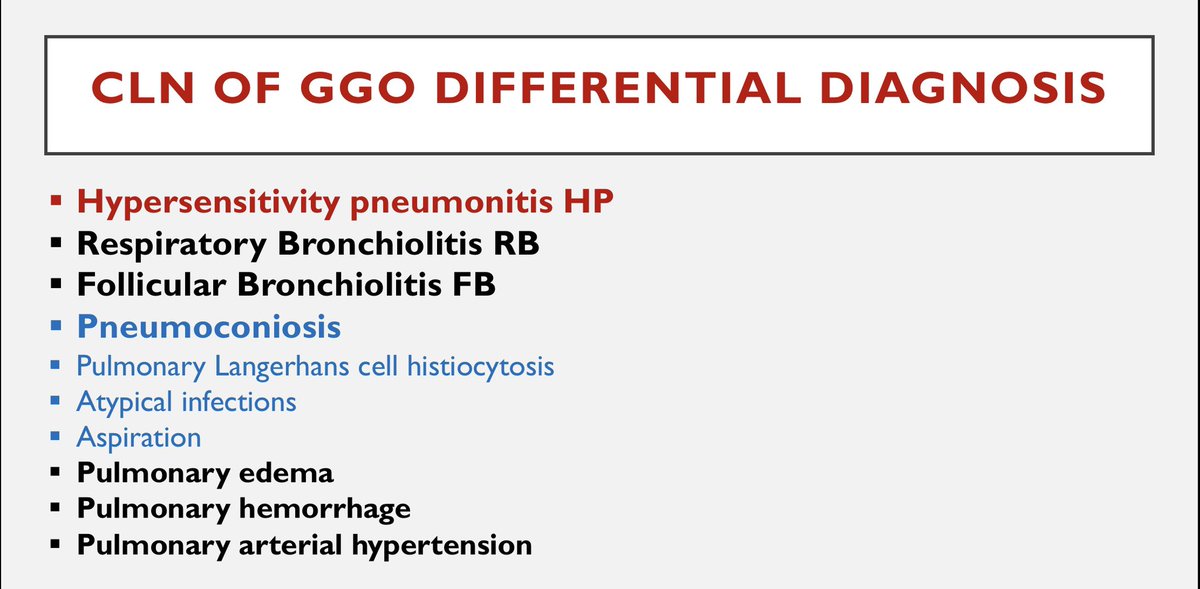
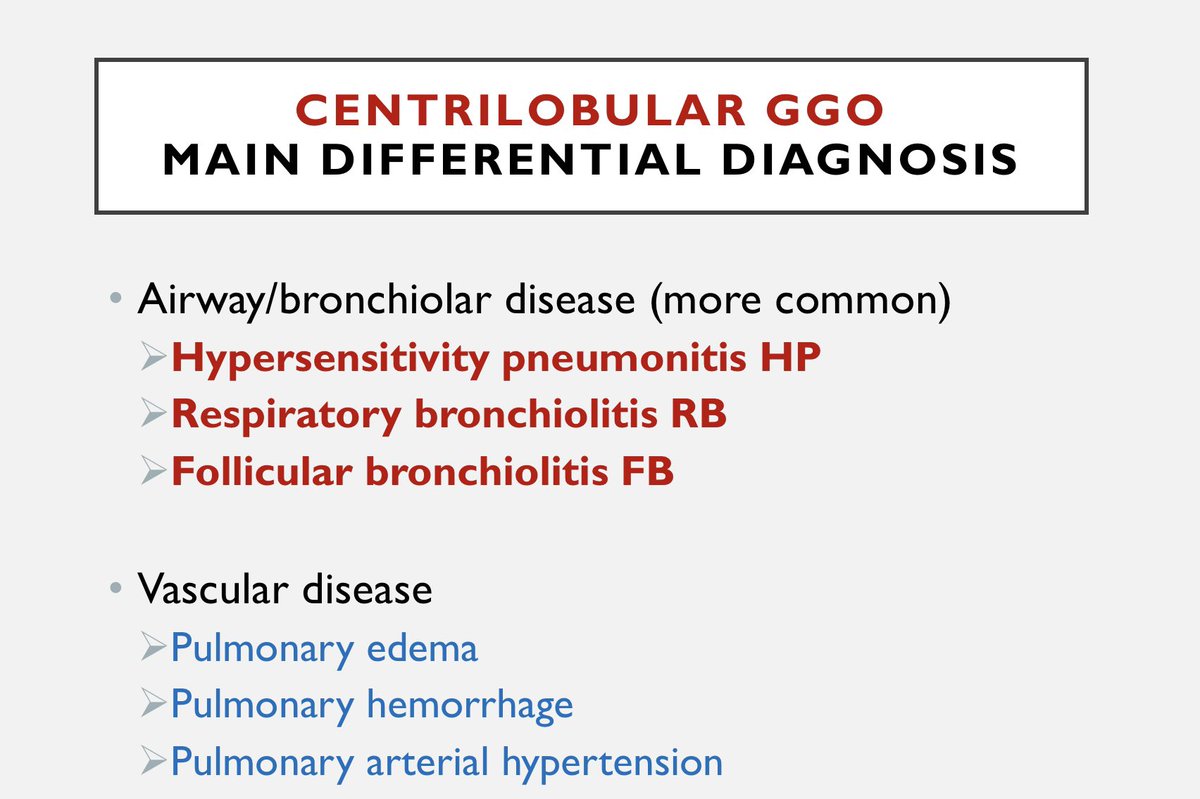
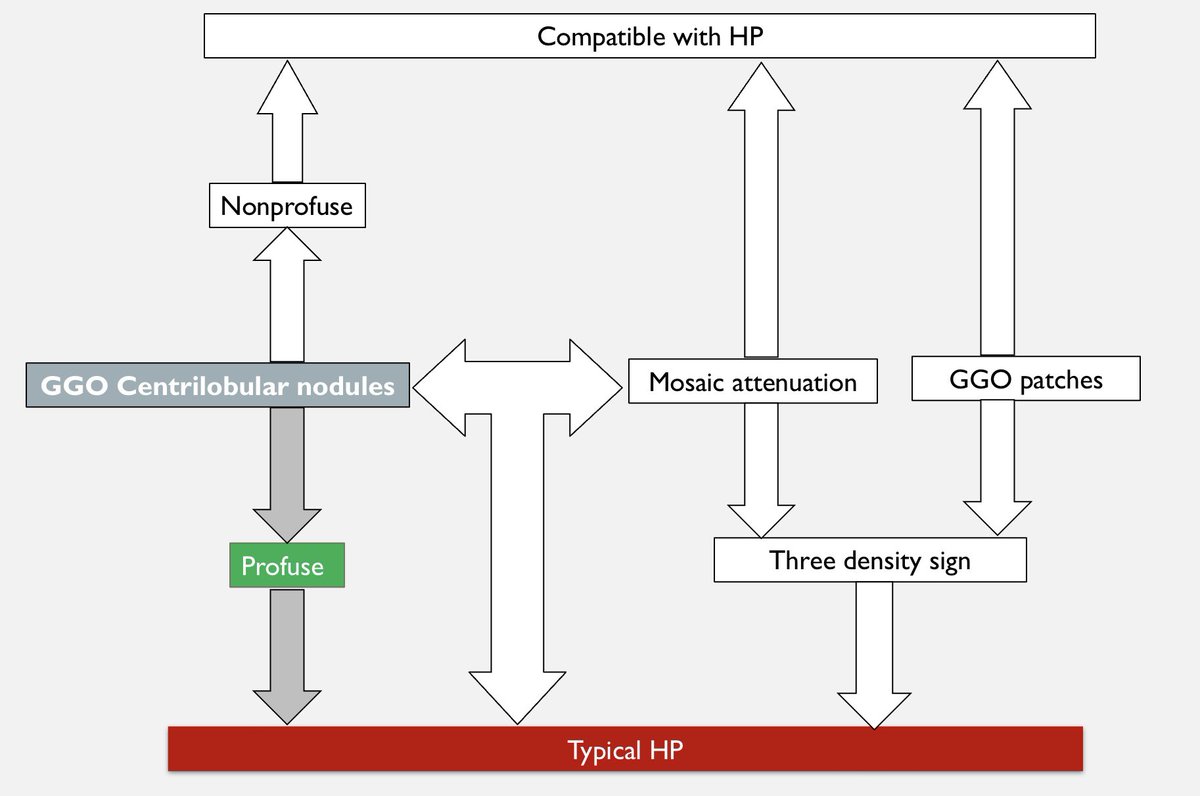
In evaluating pulmonary micronodules, the initial step involves categorizing micronodules based on distribution. Since these nodules are absent along major fissures or pleural surfaces, they exhibit a centrilobular CLN distribution. The next crucial aspect is recognizing the density of the nodules, differentiating between ground glass and soft tissue density. Identifying ground glass density prompts consideration of underlying causes, such as small airway disease or vascular disease. In this case, the absence of pulmonary edema, pulmonary hypertension, or diffuse pulmonary hemorrhage points to airway disease. The primary differentials for small airway disease include hypersensitivity pneumonitis, respiratory bronchiolitis, and follicular bronchiolitis. Profuse centrilobular nodules of ground glass density, as seen here, are indicative of hypersensitivity pneumonitis, especially in the absence of alternative features. Respiratory bronchiolitis typically involves upper lobes in smokers, while follicular bronchiolitis requires a history of collagen vascular disease or immunosuppression and doesn't present with extensive micronodularity. Atypical infections may share a similar presentation but lack the pronounced profuseness observed in this case. The clinician suspected pulmonary tuberculosis, prompting an HRCT due to negative AFB tests. Tuberculosis, a typical infection, presents with centrilobular nodules of soft tissue density accompanied by a tree-in-bud pattern. In summary, the case likely involves non-fibrotic hypersensitivity pneumonitis.
Loading suggestions...