🧵 **Tweetorial**: Unraveling the Impact of Intravitreal Anti-VEGF on Kidney Failure 🧵
Do you think intravitreal anti-vegf agents cause renal disease?
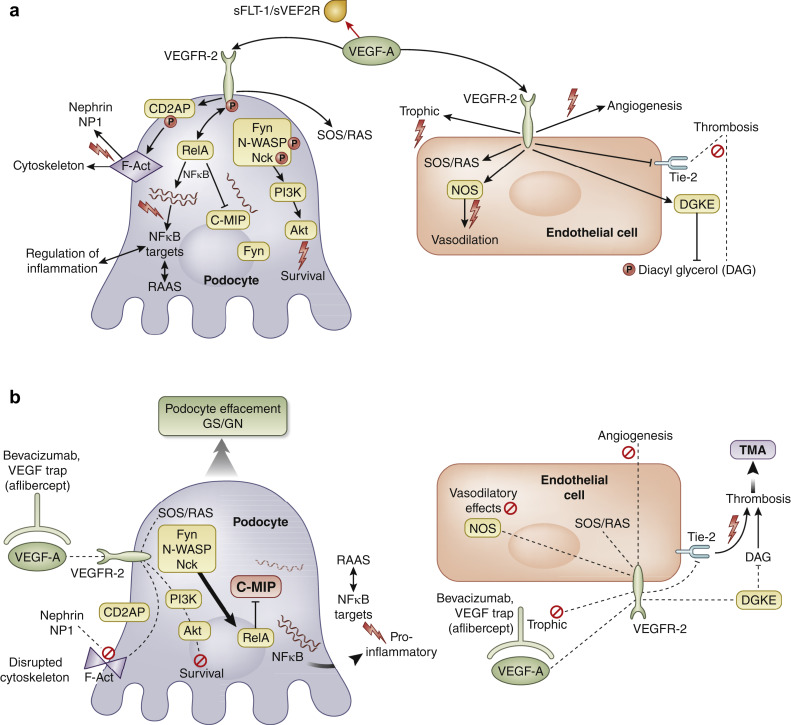
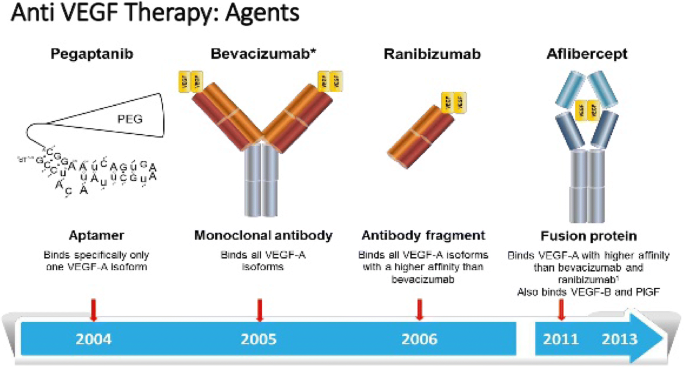
2/ Some case series data suggests that there is some risk of endothelial injury with such agents used for treating diabetic retinopathy or Macular degeneration linkinghub.elsevier.com @Kidney_Int @RMHUCINEPHRO
3/ More case reviews suggests that one type may be more risky for the kidney than other ncbi.nlm.nih.gov
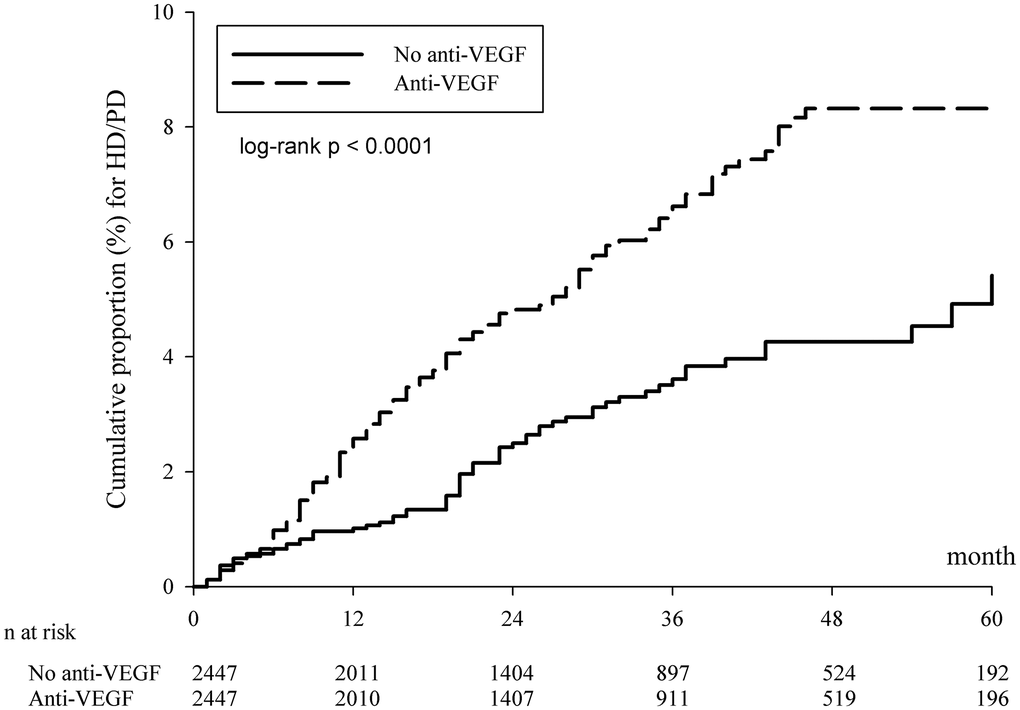
4/ A recent study also showed that pubmed.ncbi.nlm.nih.gov Risk of dialysis in patients receiving intravitreal anti-vascular endothelial growth factor treatment: a population-based cohort study
5/ 🚨 Big news for ophthalmologists and nephrologists! Our new study sheds light on the risk of kidney failure from intravitreal anti-VEGF treatments. Let's dive in! #ophthalmology #nephrology- @jiahweing @drdeidracrews @hopkinsneph sciencedirect.com @HofstraKidney
6/ 🎯 **Objective**: The study aimed to:
A) Determine the incidence of kidney failure in patients exposed to intravitreal anti-VEGF.
B) Compare kidney failure risk across 3 treatments: ranibizumab, aflibercept, & bevacizumab.
#retinacare
A) Determine the incidence of kidney failure in patients exposed to intravitreal anti-VEGF.
B) Compare kidney failure risk across 3 treatments: ranibizumab, aflibercept, & bevacizumab.
#retinacare
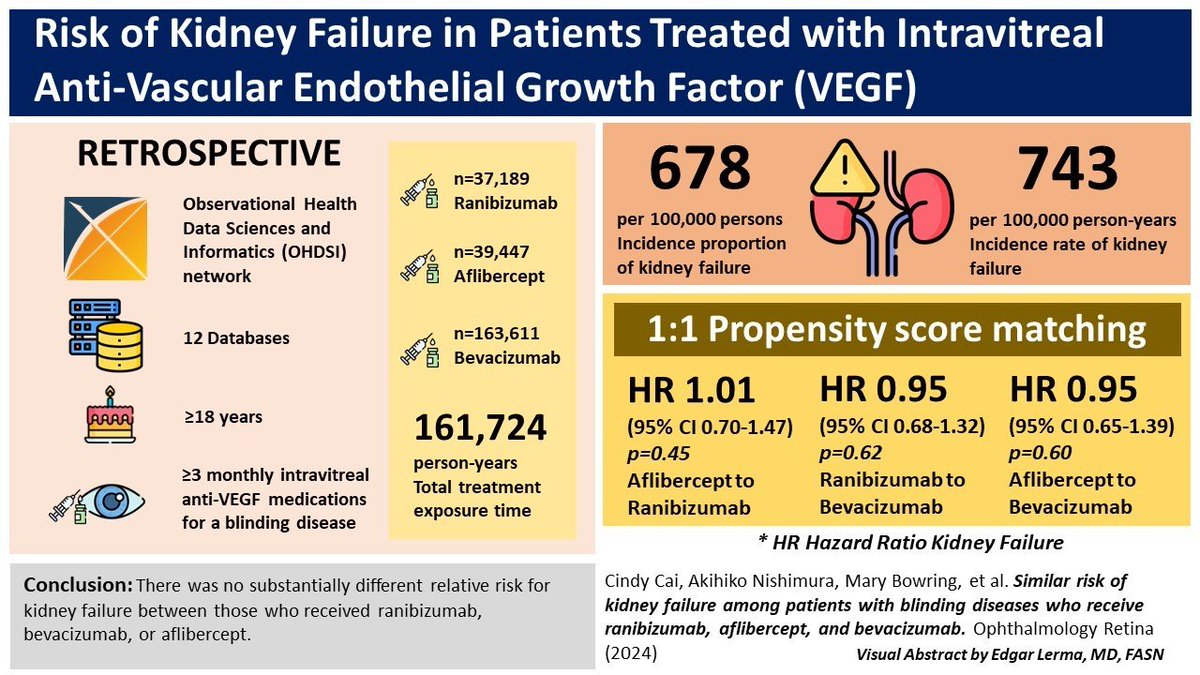
7/ 📚 **Design**: This was a retrospective cohort study, leveraging 12 databases within the OHDSI network. A massive endeavor to understand a critical patient safety issue! #healthdata ohdsi.org
8/🎬 **Participants**: Included were adults ≥18 years receiving ≥3 monthly intravitreal anti-VEGF injections for conditions like diabetic retinopathy and age-related macular degeneration. Over 6 million patients' data were analyzed! #patientcare
9/ 📈 **Methods**:
- Standardized incidence proportions & rates of kidney failure during treatment were calculated.
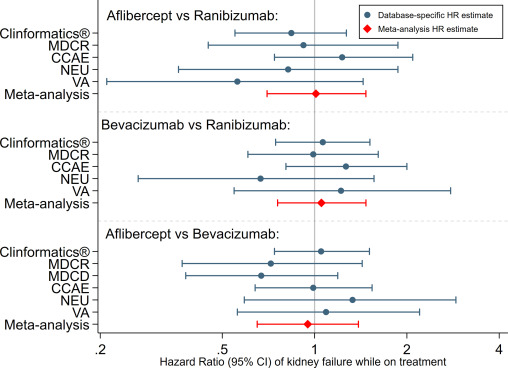
- Patients were matched 1:1 using propensity scores to compare treatments.
- A meta-analysis combined data for a comprehensive look. #clinicalresearch
- Standardized incidence proportions & rates of kidney failure during treatment were calculated.
- Patients were matched 1:1 using propensity scores to compare treatments.
- A meta-analysis combined data for a comprehensive look. #clinicalresearch
10/📊 **Results**:
- Out of 6.1M, 37,189 received ranibizumab, 39,447 aflibercept, & 163,611 bevacizumab.
- Incidence of kidney failure was 678 per 100,000 persons.
- No significant difference in kidney failure risk among the treatments. #studyfindings
- Out of 6.1M, 37,189 received ranibizumab, 39,447 aflibercept, & 163,611 bevacizumab.
- Incidence of kidney failure was 678 per 100,000 persons.
- No significant difference in kidney failure risk among the treatments. #studyfindings
12/🤔 **What does this mean?**
This extensive study provides comforting evidence that there's little risk difference in kidney failure among the three major anti-VEGF treatments. A crucial insight for prescribing doctors! #eyedisease but there is renal disease.
This extensive study provides comforting evidence that there's little risk difference in kidney failure among the three major anti-VEGF treatments. A crucial insight for prescribing doctors! #eyedisease but there is renal disease.
13/ We find an incidence rate of 743 per 100,000 person-years with a standardized incidence proportion of 678 per 100,000 persons of kidney failure, which is higher than the overall population, among patients who are on treatment with intravitreal anti-VEGF medications.
14/ Limitations: Definitions used in OHDSI, dosing information, and retrospective nature of the study. But, this is the largest study examining the association between intravitreal anti-VEGF and AKI & the largest application of the OHDSI network to an ophthalmic question to date.
15/ 📌 **Final Thought**: This study highlights the importance of large-scale data analysis in understanding the safety profiles of treatments. A win for evidence-based medicine! #EBM
16/ Special thanks to all the Retina specialists and Nephrologists on the paper and lead author Dr. Cindy X. Cai @ASNKidney @nkf @aao_ophth @RetinaToday #diabetes #retina #renal @onconephsociety @AAOjournal #endXorial
Loading suggestions...