#POCUS #MedTwitter #FOAMed
How can POCUS differentiate Acute PE and Chronic Pulmonary Hypertension❓
1/
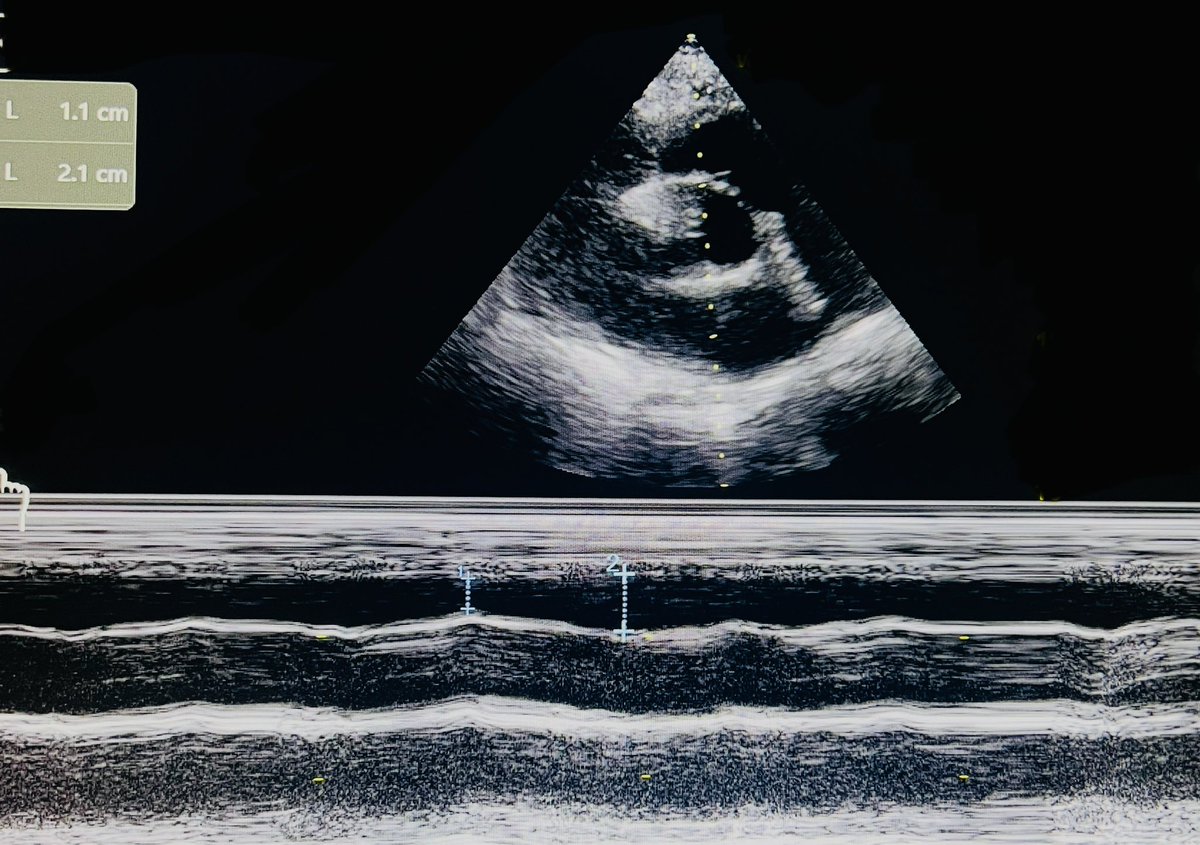
❇️ RVOT Systolic Excursion and Acute PE:
✅ RVOT end-diastolic diameter (RVOT EDD) ➡️ measured at onset of the Q-wave and
✅ RVOT end-systolic diameter (RVOT ESS) ➡️ measured at end of T-wave
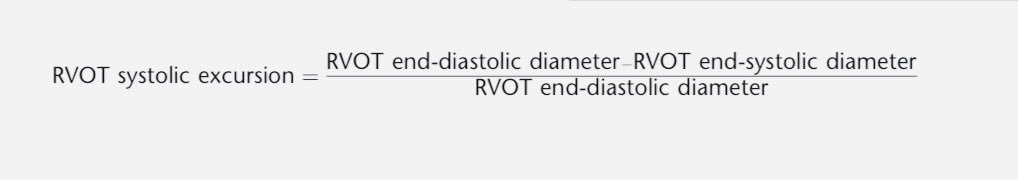
🛑 RVOT Systolic Excursion ➡️
(RVOT EDD - RVOT ESS)/RVOT EDD
☑️ < 24.3 % Acute PE
☑️ 100% sensitivity, 95.56% specificity‼️
🔗 pubmed.ncbi.nlm.nih.gov.
How can POCUS differentiate Acute PE and Chronic Pulmonary Hypertension❓
1/
❇️ RVOT Systolic Excursion and Acute PE:
✅ RVOT end-diastolic diameter (RVOT EDD) ➡️ measured at onset of the Q-wave and
✅ RVOT end-systolic diameter (RVOT ESS) ➡️ measured at end of T-wave
🛑 RVOT Systolic Excursion ➡️
(RVOT EDD - RVOT ESS)/RVOT EDD
☑️ < 24.3 % Acute PE
☑️ 100% sensitivity, 95.56% specificity‼️
🔗 pubmed.ncbi.nlm.nih.gov.
2/
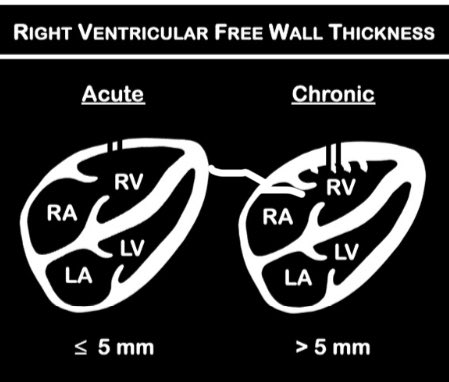
❇️ Right Ventricular Free Wall Thickness
✔️ < 5mm ➖Acute PE
✔️ > 5mm ➖ Chronic RV dysfunction (90-93% sensitive, 94-95% specific)
🔗 ncbi.nlm.nih.gov.
❇️ Right Ventricular Free Wall Thickness
✔️ < 5mm ➖Acute PE
✔️ > 5mm ➖ Chronic RV dysfunction (90-93% sensitive, 94-95% specific)
🔗 ncbi.nlm.nih.gov.
@ArgaizR @Drnasap @msiuba @nickmmark 3/
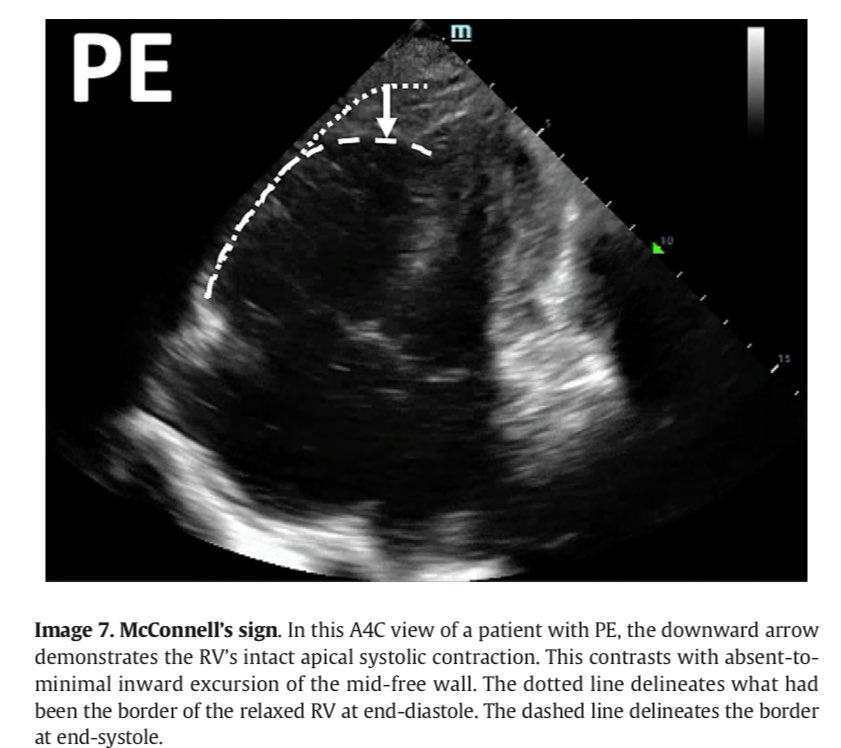
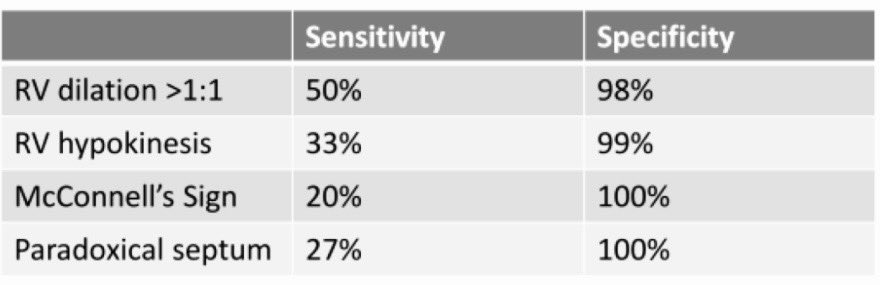
❇️ McConnell’s Sign
❌ Not sensitive (20%)
✅ Highly specific (100%)
🚧 This sign is positive in around 17% of patients with chronic pulmonary hypertension ‼️
🔗 pubmed.ncbi.nlm.nih.gov.
❇️ McConnell’s Sign
❌ Not sensitive (20%)
✅ Highly specific (100%)
🚧 This sign is positive in around 17% of patients with chronic pulmonary hypertension ‼️
🔗 pubmed.ncbi.nlm.nih.gov.
4/
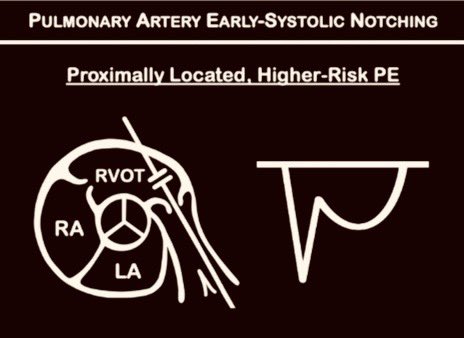
❇️ Pulmonary Artery Early Systolic Notching
✅ Proximally-located, higher-risk PEs ➡️ Sensitivity 69-97%, Specificity 90- 99%
🔗 pubmed.ncbi.nlm.nih.gov).
❇️ Pulmonary Artery Early Systolic Notching
✅ Proximally-located, higher-risk PEs ➡️ Sensitivity 69-97%, Specificity 90- 99%
🔗 pubmed.ncbi.nlm.nih.gov).
@POCUSpeek 5/
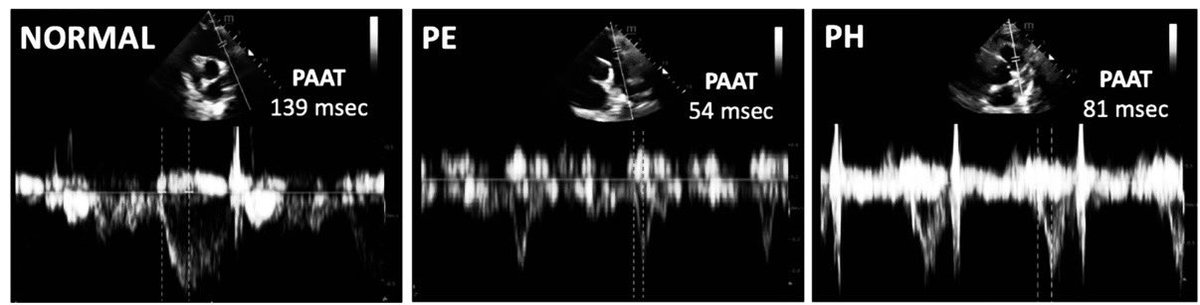
❇️ Pulmonary Artery Acceleration Time
✔️ ≤ 60-80 msec ➡️ Acute PE
✔️ < 105 msec ➡️ Chronic right ventricular dysfunction
❇️ Pulmonary Artery Acceleration Time
✔️ ≤ 60-80 msec ➡️ Acute PE
✔️ < 105 msec ➡️ Chronic right ventricular dysfunction
@POCUSpeek 6/
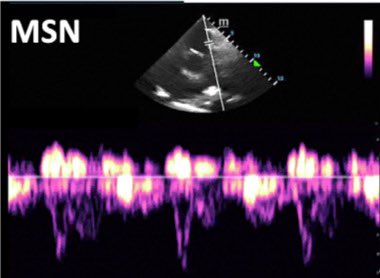
❇️ Midsystolic Notching
▶️ ‘Spike and dome pattern’
▶️ Seen in both peripherally-located, lower-risk PE and chronic PH‼️
❇️ Midsystolic Notching
▶️ ‘Spike and dome pattern’
▶️ Seen in both peripherally-located, lower-risk PE and chronic PH‼️
@POCUSpeek 7/
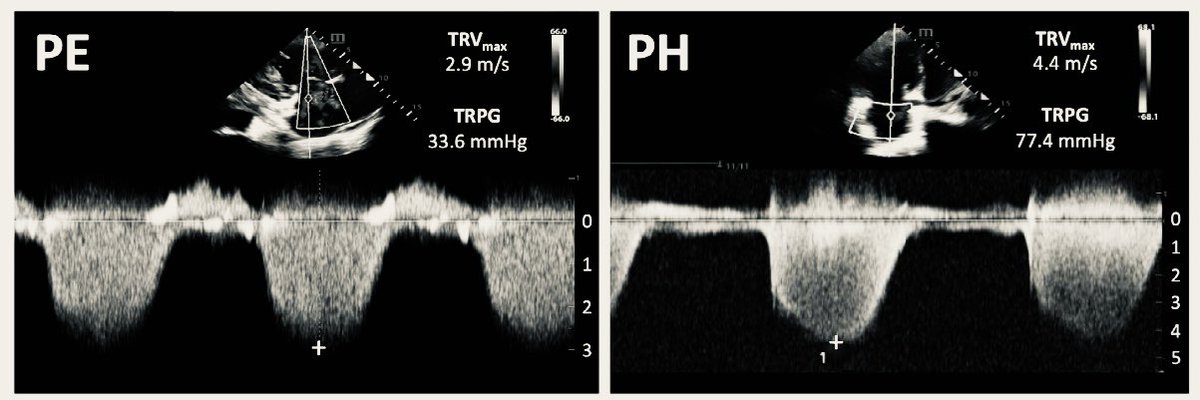
❇️ 60/60 Sign
♦️ Tricuspid regurgitation pressure gradient ≤ 60 mmHg (TRVmax ≤ 3.9 m/sec)
♦️Pulmonary artery acceleration time ≤ 60 ms
🚧 Sensitivity 13−71%, Specificity 69–98% ‼️
❇️ 60/60 Sign
♦️ Tricuspid regurgitation pressure gradient ≤ 60 mmHg (TRVmax ≤ 3.9 m/sec)
♦️Pulmonary artery acceleration time ≤ 60 ms
🚧 Sensitivity 13−71%, Specificity 69–98% ‼️
@POCUSpeek 8/
To wrap up -
To wrap up -
@POCUSpeek @Rajiv_Sinanan @katiewiskar @MDBeni @Thind888 @MegriMohammed @norfolk_tim How often do you use RVOT Systolic excursion in your practice❓
Loading suggestions...