Breaking Down Bradycardia 🕰️
Slow heart rate with potential big impact. Dive into this high-yield 🧵 from @GlassHealthHQ
#MedTwitter #MedX #MedED #Cardiology #ACC2024
1/16
Slow heart rate with potential big impact. Dive into this high-yield 🧵 from @GlassHealthHQ
#MedTwitter #MedX #MedED #Cardiology #ACC2024
1/16
Context Team: @Joshua___Ross @kassisMD @MaxCollMD @AlexSpacht @Gurbanikaur.
Tweetorial Team: @ShivaniReddy_1 @AmierHaidar @clarencetsaiMD
Bradycardia AI Context Article with References:
glass.health
2/16
Tweetorial Team: @ShivaniReddy_1 @AmierHaidar @clarencetsaiMD
Bradycardia AI Context Article with References:
glass.health
2/16
Definition 📌
- The NIH defines sinus bradycardia as a heart rate < 60 bpm in adults other than well-trained athletes.
- However, the ACC/AHA Task Force on Clinical Practice Guidelines & the Heart Rhythm Society have defined it as a sinus rate of < 50 bpm.
3/16
- The NIH defines sinus bradycardia as a heart rate < 60 bpm in adults other than well-trained athletes.
- However, the ACC/AHA Task Force on Clinical Practice Guidelines & the Heart Rhythm Society have defined it as a sinus rate of < 50 bpm.
3/16
What are the causes of pathologic bradycardia?
- Sinus node dysfunction (SND) (aka sick sinus syndrome) or atrioventricular (AV) block.
- SND is the most common cause of bradycardia in the US, especially in patients over the age of 65. 👴 👵
4/16
- Sinus node dysfunction (SND) (aka sick sinus syndrome) or atrioventricular (AV) block.
- SND is the most common cause of bradycardia in the US, especially in patients over the age of 65. 👴 👵
4/16
Other causes:
- Ischemic ❤️🔥
- Infectious (Chagas, Endocarditis, Lyme disease) 🦠
- Infiltrative (sarcoidosis, amyloidosis)
- Rheumatological (Lupus)
- Procedural trauma (s/p cath or valve surgery)
- OSA
- Metabolic ( ⬆️ or ⬇️ K, hypothyroidism)
- Drugs (eg. opioids)
5/16
- Ischemic ❤️🔥
- Infectious (Chagas, Endocarditis, Lyme disease) 🦠
- Infiltrative (sarcoidosis, amyloidosis)
- Rheumatological (Lupus)
- Procedural trauma (s/p cath or valve surgery)
- OSA
- Metabolic ( ⬆️ or ⬇️ K, hypothyroidism)
- Drugs (eg. opioids)
5/16
Also, consider familial/inherited conduction disorders such as SCN5A gene mutation for cardiac sodium channel 🧂 and HCN4 gene mutation for cardiac pacemaker channel 💓
6/16
6/16
How does it present?
Young healthy patients or athletes may be asymptomatic 🏊♂️
Symptomatic presentation can include:
- Syncope or pre-syncope 😰
- Fatigue 😩
- Dizziness or lightheadedness 😵
- Chest pain ❤️🩹
- Shortness of breath 🫁
- Altered mental status 🧠
7/16
Young healthy patients or athletes may be asymptomatic 🏊♂️
Symptomatic presentation can include:
- Syncope or pre-syncope 😰
- Fatigue 😩
- Dizziness or lightheadedness 😵
- Chest pain ❤️🩹
- Shortness of breath 🫁
- Altered mental status 🧠
7/16
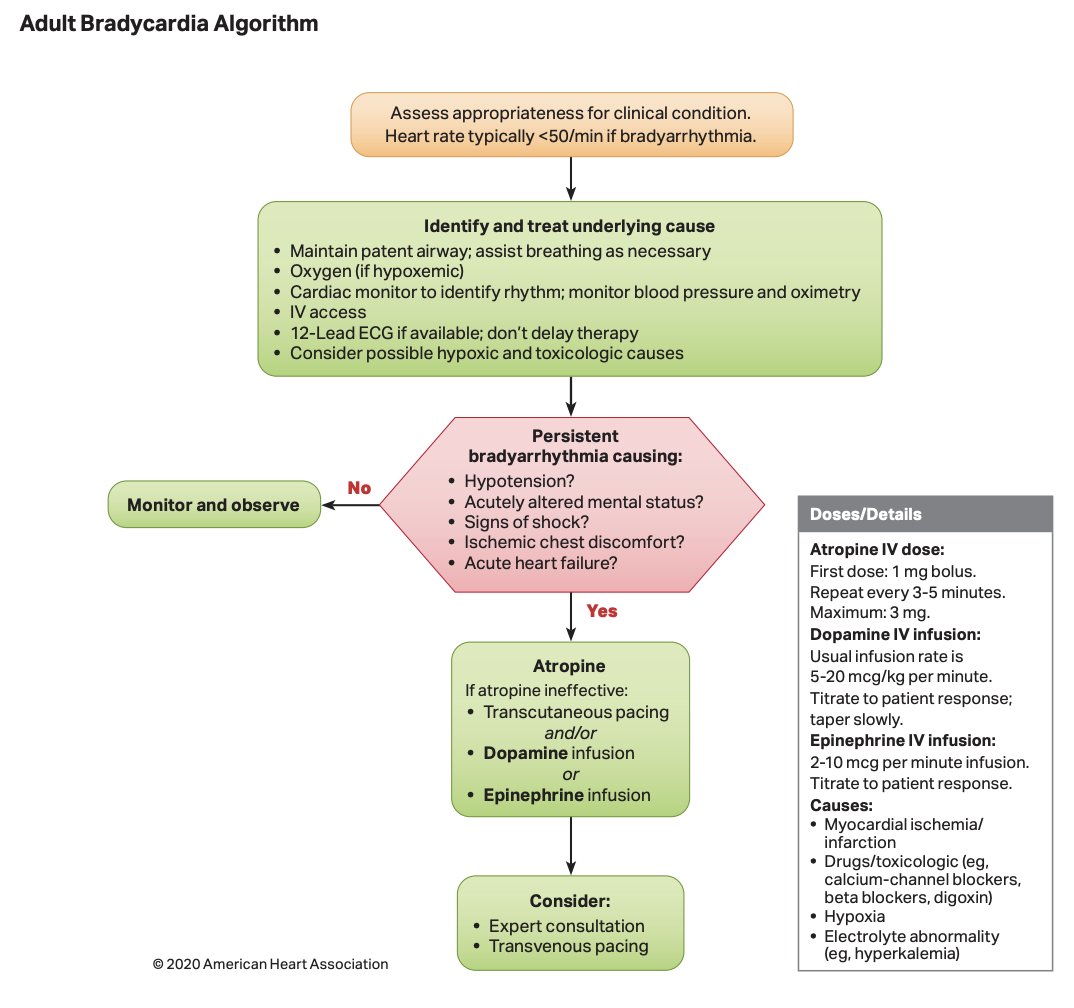
❌ Avoid atropine in patients who are s/p heart transplant or have high-degree AV block.
Use it with caution with those w/ active coronary ischemia, glaucoma, GI obstruction, and pyloric stenosis.
9/16
Use it with caution with those w/ active coronary ischemia, glaucoma, GI obstruction, and pyloric stenosis.
9/16
❓The patient does not respond to atropine? How should we proceed next?
💡 Transcutaneous pacing! It provides temporary rate support until transvenous pacing or a permanent pacemaker can be placed.
10/16
💡 Transcutaneous pacing! It provides temporary rate support until transvenous pacing or a permanent pacemaker can be placed.
10/16
💊 Other med options if atropine is ineffective & pacing is unavailable: dopamine (2-10 mcg/kg/min), epi (2-10 mcg/min), isoproterenol (20-60 mcg bolus + 1-20 mcg/min infusion), aminophylline (250 mg bolus; for pts w/ 2nd or 3rd degree AV block associated w/ inferior MI)
11/16
11/16
What if we have a patient who has drug-induced bradycardia?
👉 Ca-channel blocker overdose (OD): tx w/ 10% Ca gluconate or 10% Ca chloride
👉 Beta-blocker OD: tx w/ glucagon + insulin
👉 Digoxin OD: tx w/ digoxin antibody fragment
12/16
👉 Ca-channel blocker overdose (OD): tx w/ 10% Ca gluconate or 10% Ca chloride
👉 Beta-blocker OD: tx w/ glucagon + insulin
👉 Digoxin OD: tx w/ digoxin antibody fragment
12/16
🔑 For chronic management of patients w/ symptomatic bradycardia due to SND, high-degree AV block, or non-reversible causes of bradycardia, consider electrophysiology consult for pacemaker placement.
13/16
13/16
What are some complications of bradycardia? 🩺
- ❤️ Heart failure
- Worsening of ischemic heart disease
- Tachy-brady syndrome
- Cardiac arrest (asystole)
14/16
- ❤️ Heart failure
- Worsening of ischemic heart disease
- Tachy-brady syndrome
- Cardiac arrest (asystole)
14/16
🗒️ Summary:
🗝️ Bradycardia is defined as HR < 50-60 bpm
🗝️ SND or AV block are common causes
🗝️ Presentation is highly variable
🗝️ Atropine is first-line tx for hemodynamically unstable patients
🗝️ Consider PPM placement for chronic mgmt of symptomatic bradycardia
15/16
🗝️ Bradycardia is defined as HR < 50-60 bpm
🗝️ SND or AV block are common causes
🗝️ Presentation is highly variable
🗝️ Atropine is first-line tx for hemodynamically unstable patients
🗝️ Consider PPM placement for chronic mgmt of symptomatic bradycardia
15/16
We hope you've found this thread helpful.
Follow @GlassHealthHQ for more.
Like/Repost the quote below if you can:
16/16
Follow @GlassHealthHQ for more.
Like/Repost the quote below if you can:
16/16
Loading suggestions...