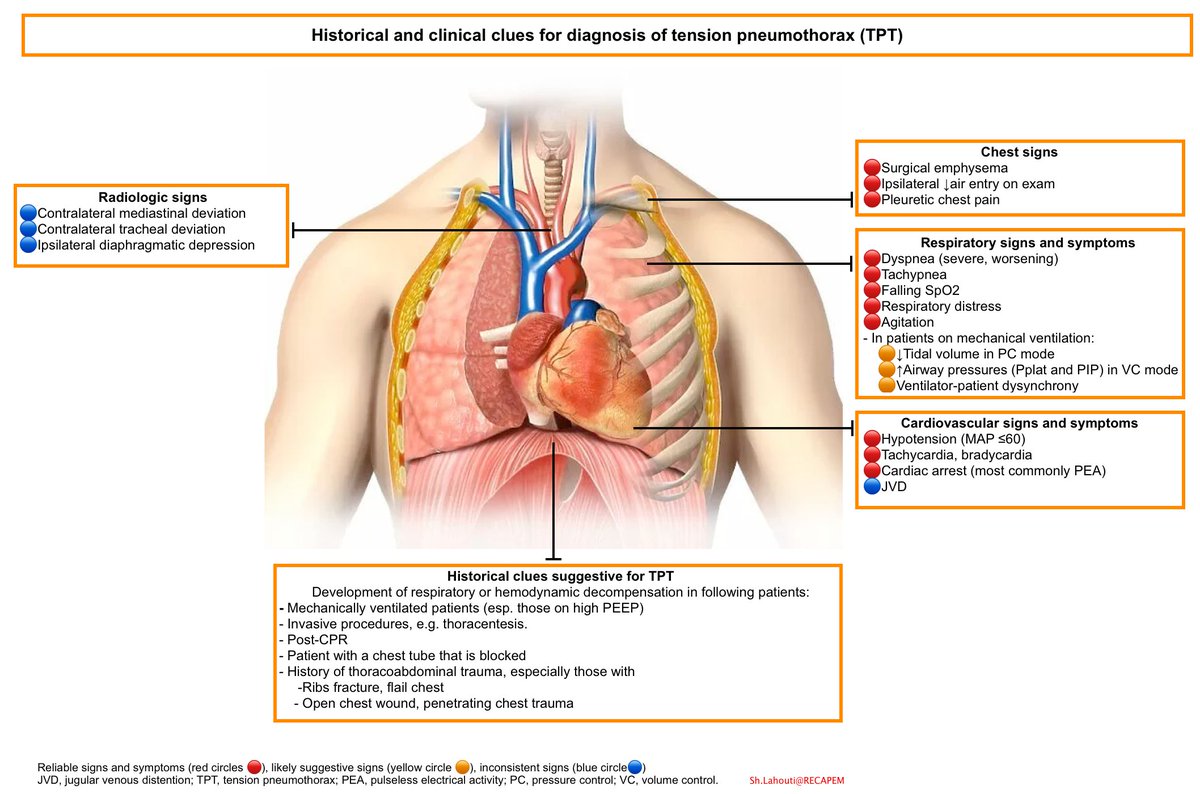
Confirmation: Tension pneumothorax is a CLINICAL diagnosis!!!
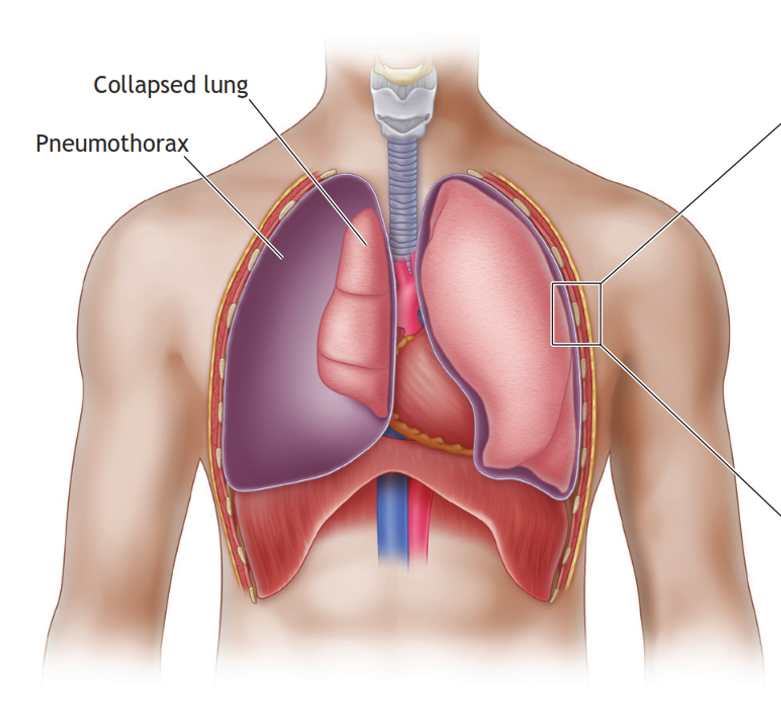
Confirm with #POCUS signs of a pneumothorax if available at the bedside. Undue delays to obtain X-ray or CT imaging MUST NOT delay your intervention, as progression may cause your patient to further deteriorate.
Confirm with #POCUS signs of a pneumothorax if available at the bedside. Undue delays to obtain X-ray or CT imaging MUST NOT delay your intervention, as progression may cause your patient to further deteriorate.
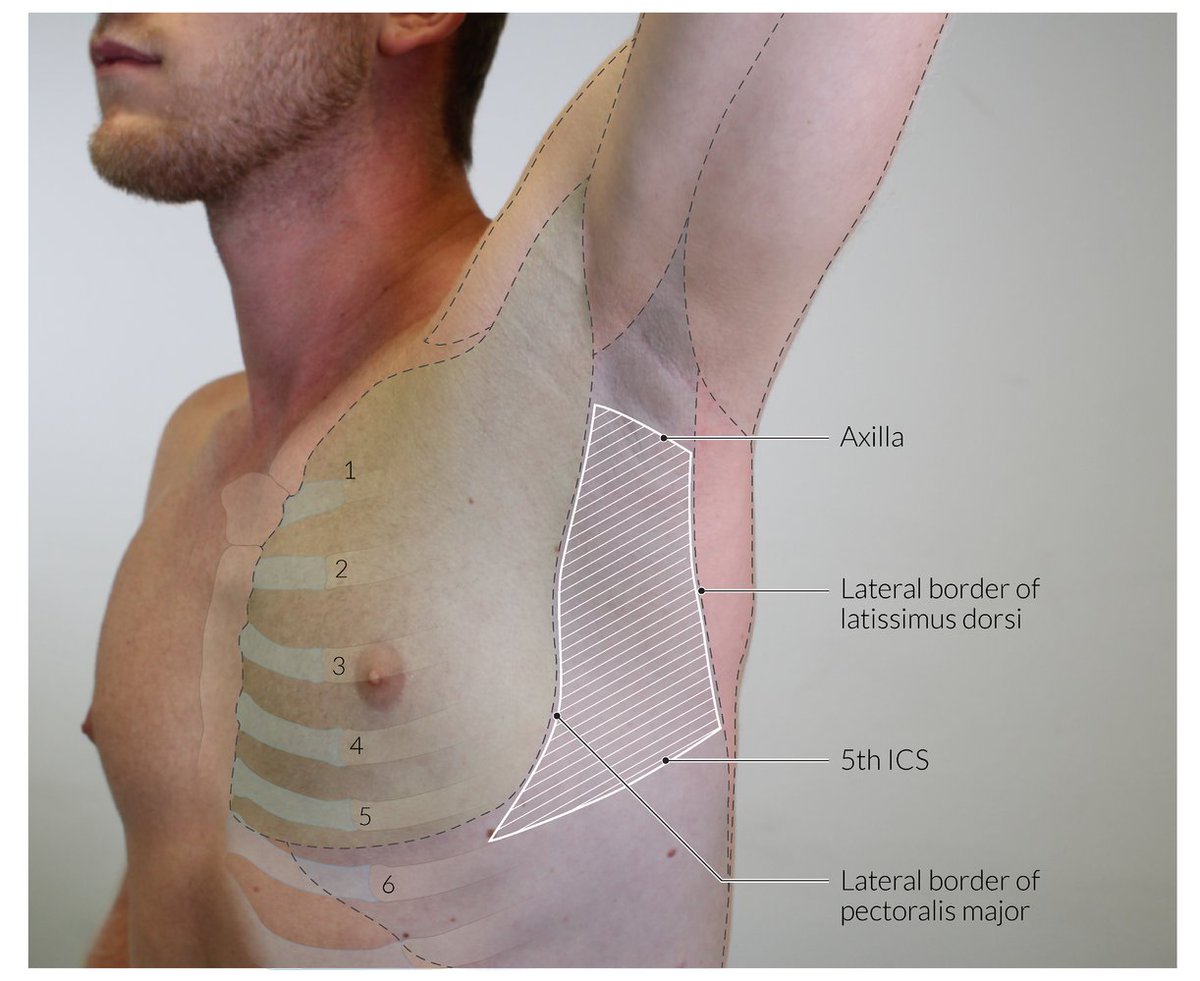
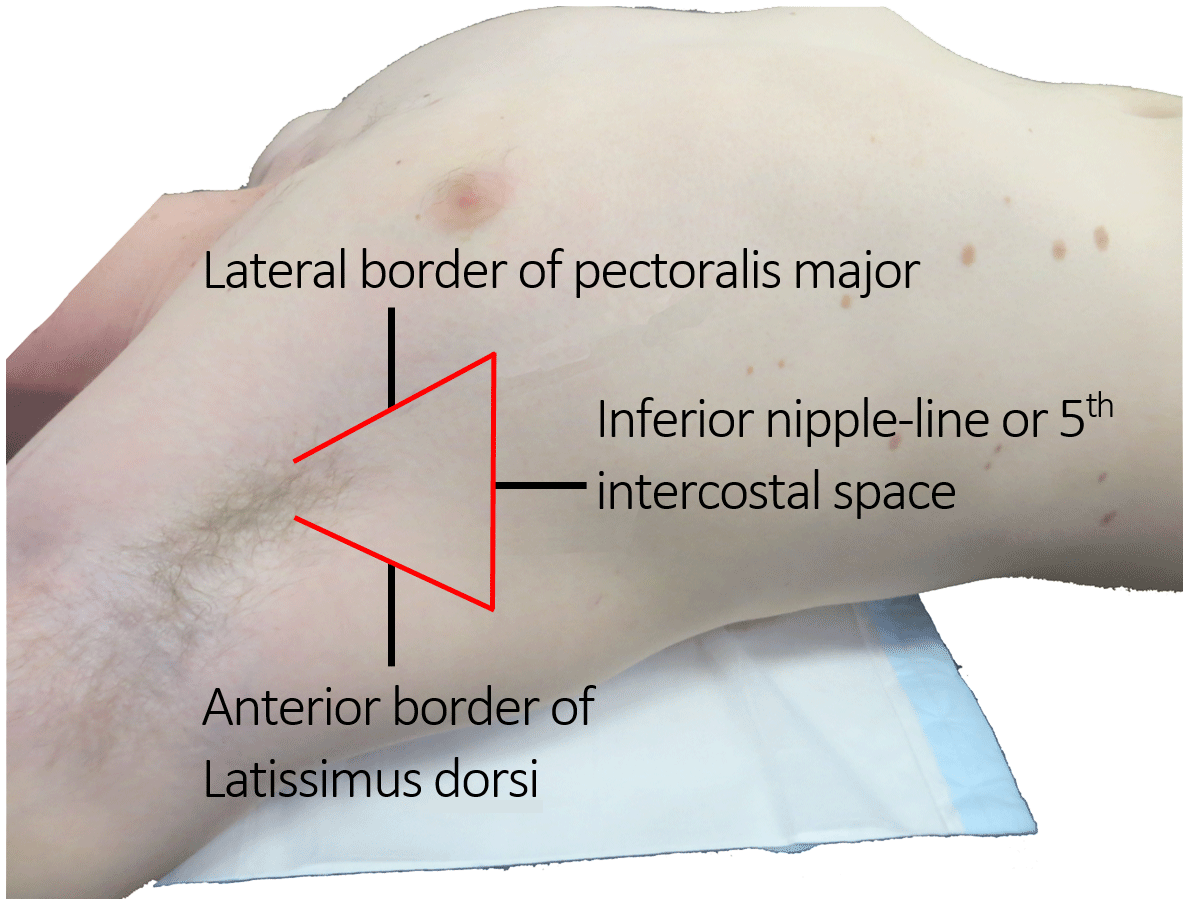
Incision parallel to the 5th rib is made on the lateral chest wall in the "Triangle of safety", and blunt dissection of a tract is performed with a closed forceps.
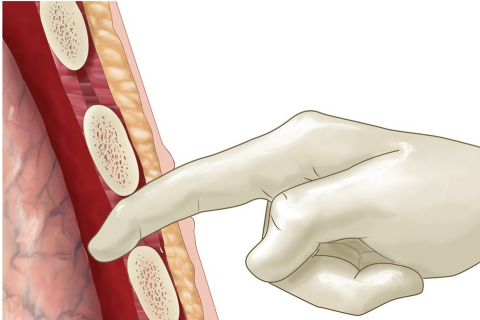
The pleural is entered and a gloved finger is introduced into the space and air drained.
clinical.stjohnwa.com.au
The pleural is entered and a gloved finger is introduced into the space and air drained.
clinical.stjohnwa.com.au
TL;DR
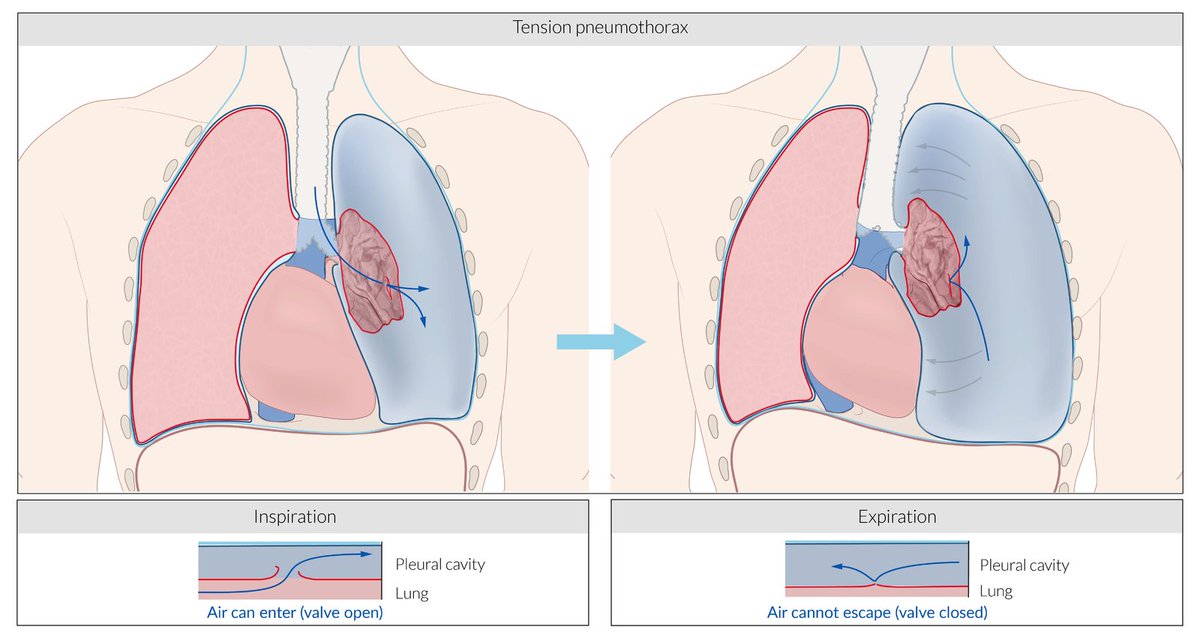
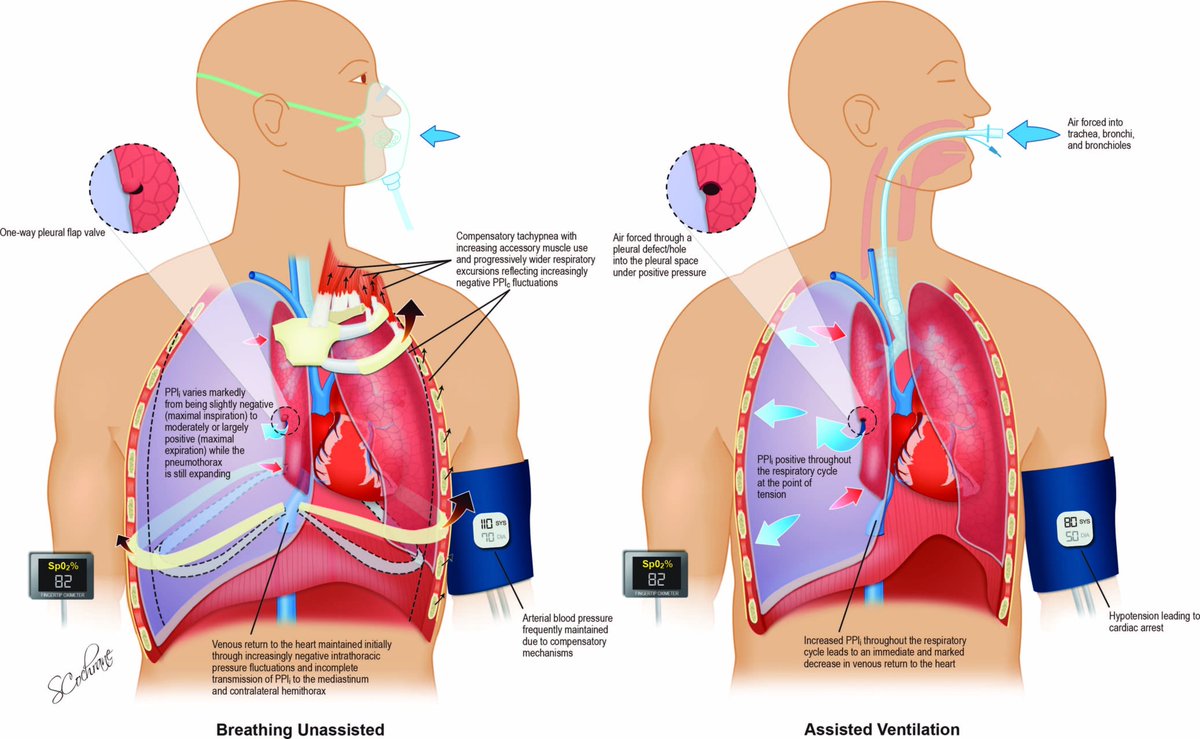
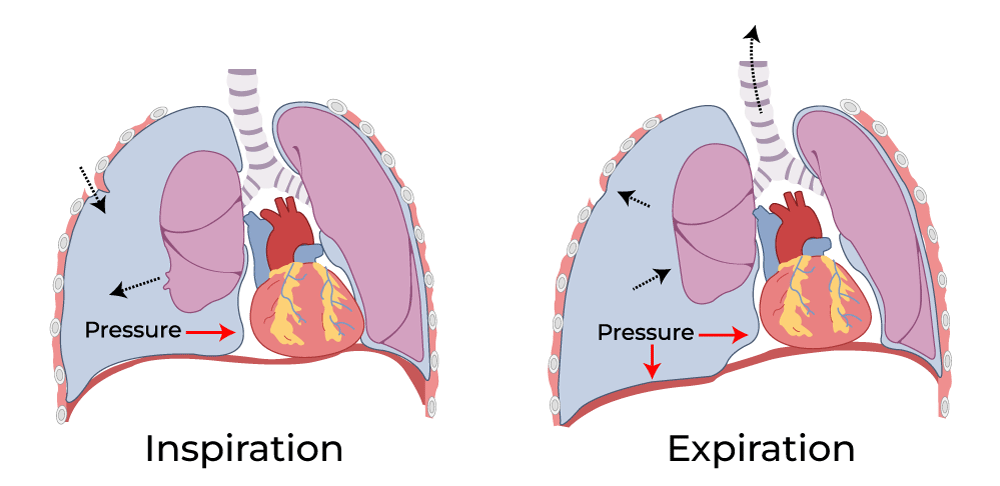
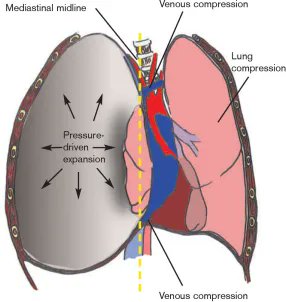
◾️Tension pneumothorax is a progressive pathology
◾️Life threatening as it worsens
◾️Diagnosed clinically
◾️Requires emergency decompression:
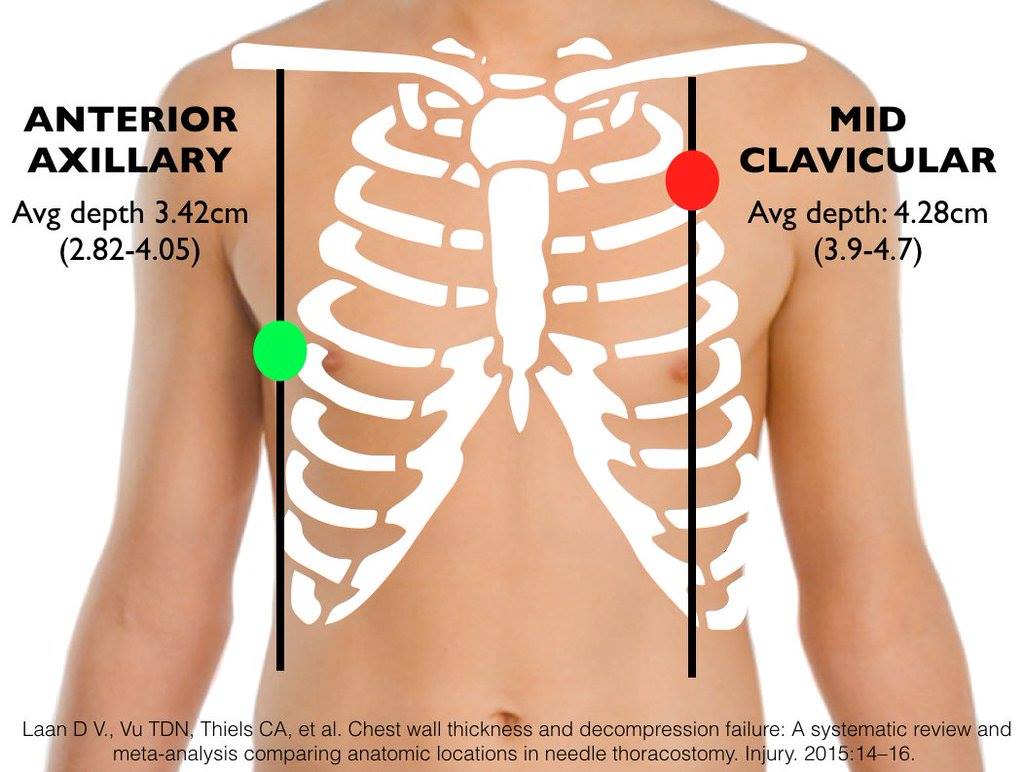
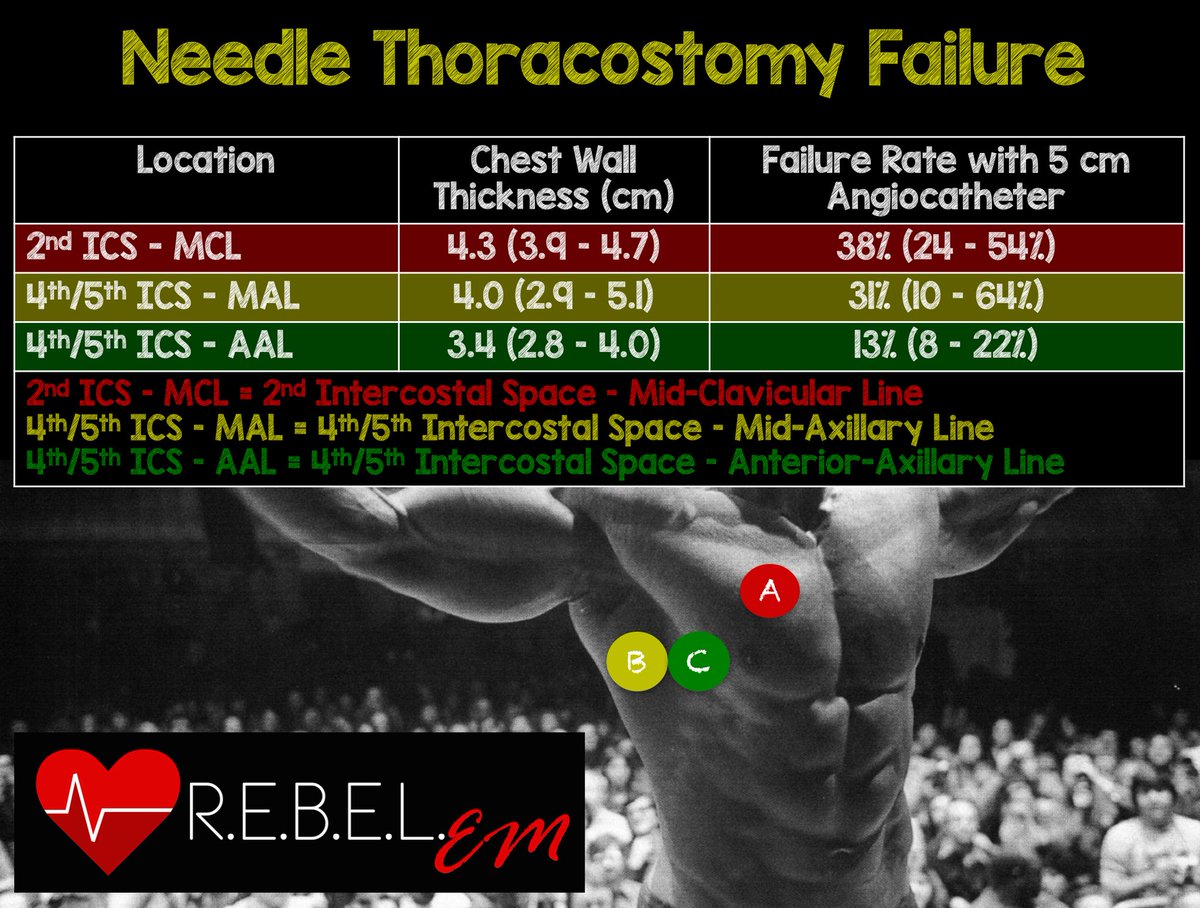
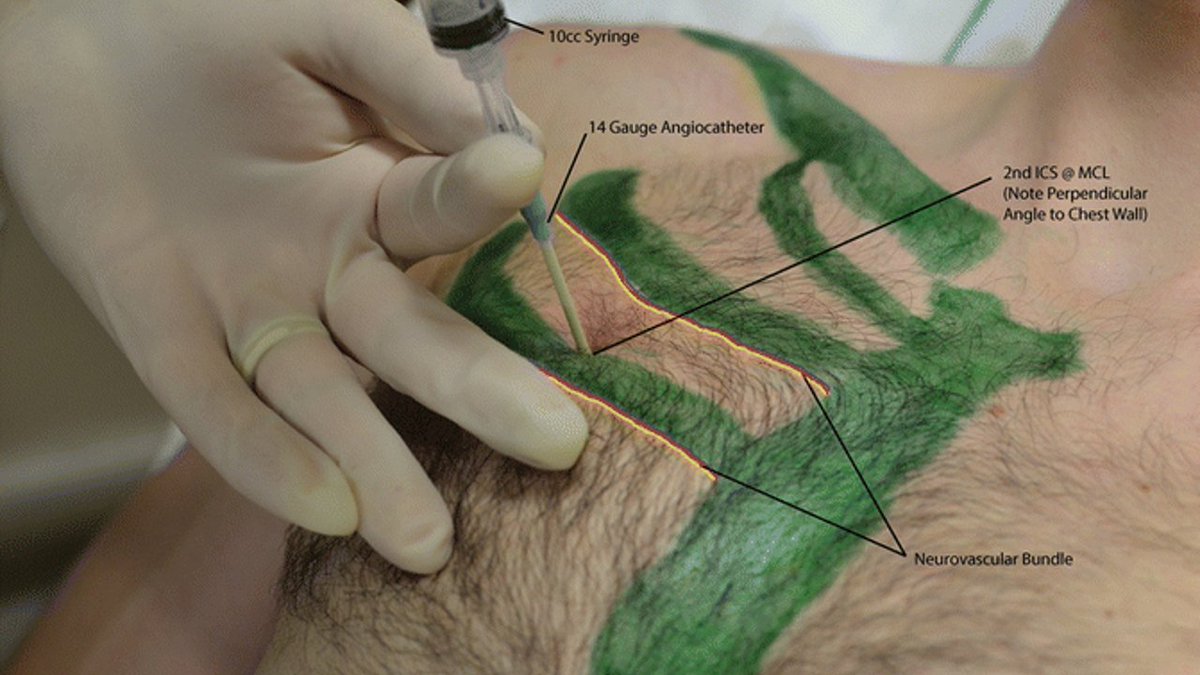
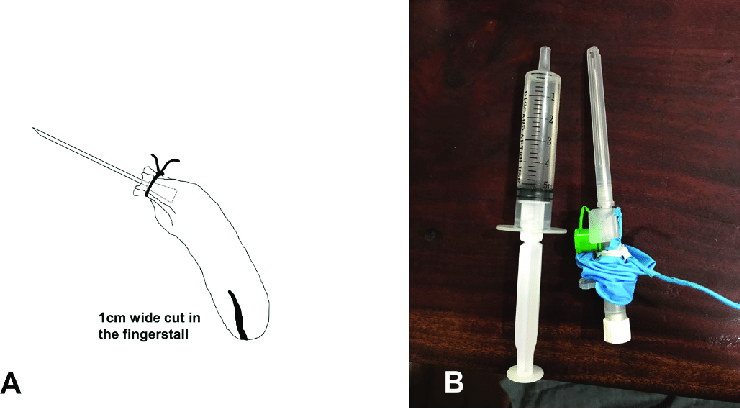
◾️Needle & finger thoracostomy are options
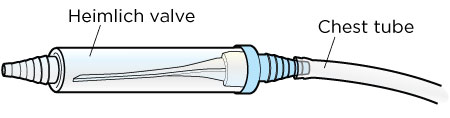
◾️Follow-up with tube thoracostomy for definitive treatment
End/🧵
Image credits in ALT
◾️Tension pneumothorax is a progressive pathology
◾️Life threatening as it worsens
◾️Diagnosed clinically
◾️Requires emergency decompression:
◾️Needle & finger thoracostomy are options
◾️Follow-up with tube thoracostomy for definitive treatment
End/🧵
Image credits in ALT
Thanks for reading. Please RT/QT from the 1st tweet of the thread which can be found here:
#Medtwitter #MedX #FOAMed #MedEd #Trauma
#Medtwitter #MedX #FOAMed #MedEd #Trauma
Loading suggestions...