The first step, we’ve all been told, is to find out what a patient means by dizzy:
⁃Vertigo
⁃Presyncope
⁃Imbalance
⁃Other
When it comes to acute dizziness, we neurologists tend to care most about vertigo.
⁃Vertigo
⁃Presyncope
⁃Imbalance
⁃Other
When it comes to acute dizziness, we neurologists tend to care most about vertigo.
But it turns out asking about a rotational spinning sensation lacks both sensitivity and specificity.
PMID: 17976352
True vertigo can cause tunnel vision and cardiac presyncope can cause a spinning sensation.
PMID: 17976352
True vertigo can cause tunnel vision and cardiac presyncope can cause a spinning sensation.
Nevertheless, there are a few history features that can point to an acute vestibular syndrome (AVS):
⁃Illusory movement in space
⁃Head motion intolerance
⁃Nausea
⁃Illusory movement in space
⁃Head motion intolerance
⁃Nausea
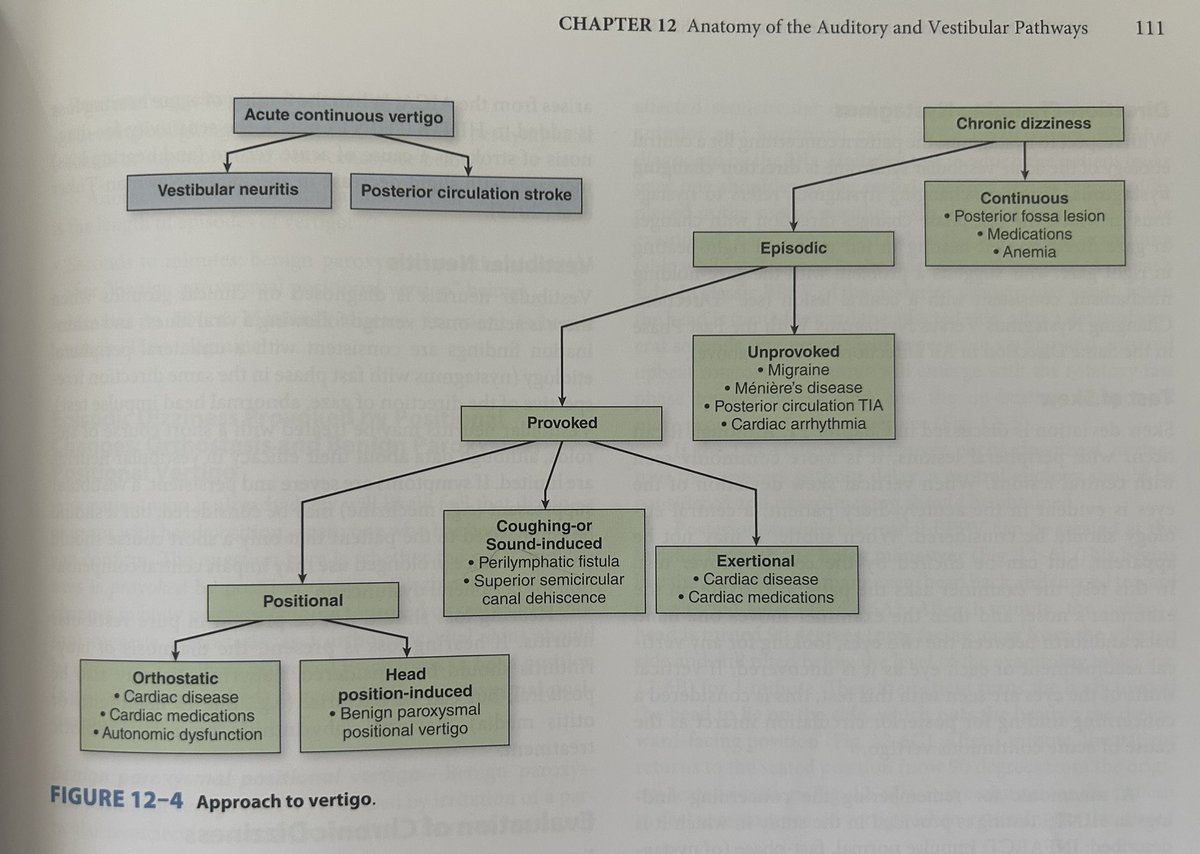
Once we’ve established AVS, the next step should be asking about triggers and timing.
⁃ Are you still having the symptoms now?
- Do they ever go away?
- What, if anything, brings them on?
Knowing this helps us sort the syndrome into the buckets below: (credit @AaronLBerkowitz)
⁃ Are you still having the symptoms now?
- Do they ever go away?
- What, if anything, brings them on?
Knowing this helps us sort the syndrome into the buckets below: (credit @AaronLBerkowitz)
Acute continuous vertigo is the most concerning as the differential includes various central causes including mass-occupying lesion and acute posterior circulation stroke.
Should we just get an MRI for anyone who feels dizzy?
Should we just get an MRI for anyone who feels dizzy?
Not so fast! There is a rapid beside neurologic exam that has high sensitivity and specificity for assessing risk for central etiology of AVS (and therefore, who needs imaging): the HINTS+ exam.
The HINTS+ test consists of:
- Head Impulse
- Nystagmus
- Test of Skew
Additionally (+) there should be no hearing loss or focal neurologic deficits like weakness, vision loss, or sensory loss.
Here’s a great video showing the exam with example patients:
youtu.be
- Head Impulse
- Nystagmus
- Test of Skew
Additionally (+) there should be no hearing loss or focal neurologic deficits like weakness, vision loss, or sensory loss.
Here’s a great video showing the exam with example patients:
youtu.be
Shameless self-plug: if you are having trouble remembering the neuroanatomy of the posterior circulation, specifically the brainstem, try using the Rule of 4s. I made a thread about it way back:
x.com
x.com
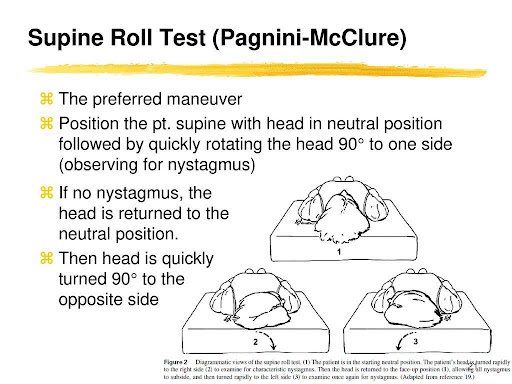
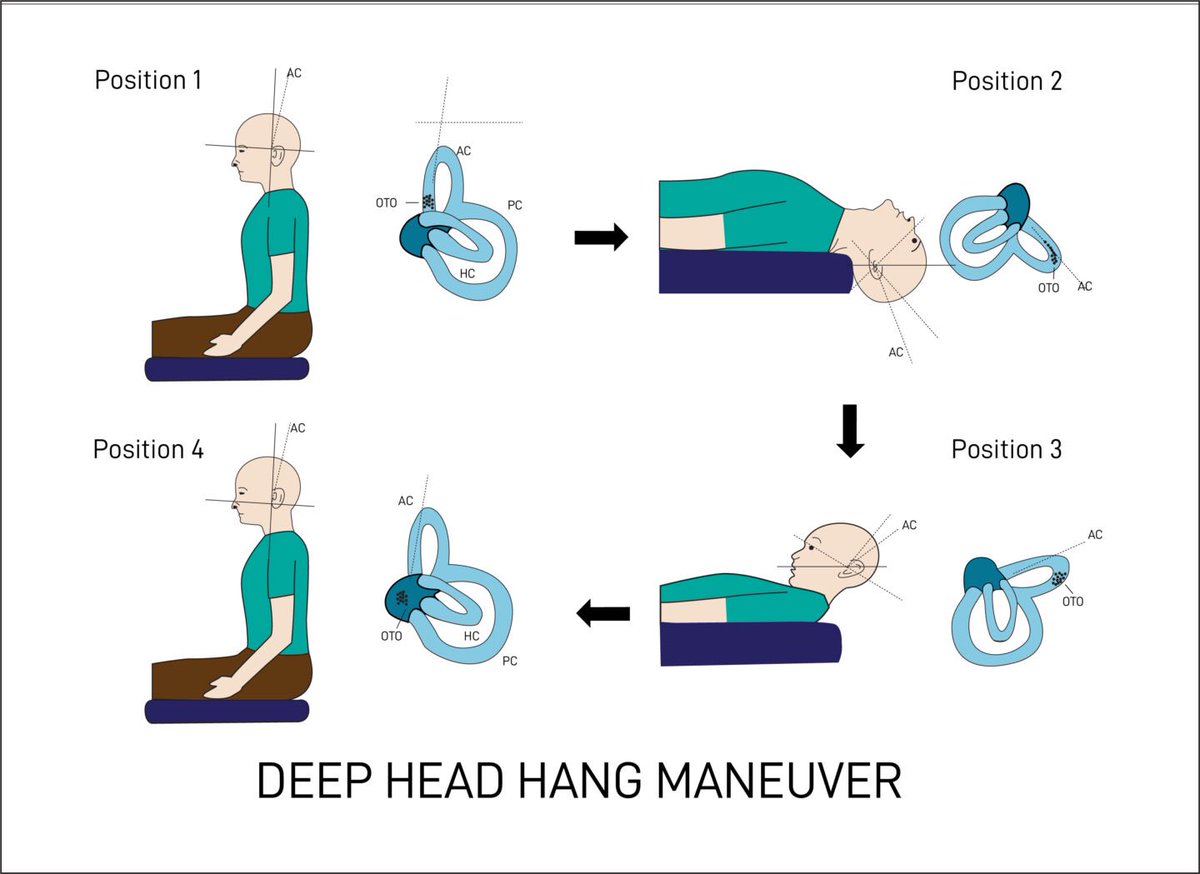
What about acute episodic vertigo?
The bottom line is that we are going to try to provoke the dizziness with exam maneuvers.
The bottom line is that we are going to try to provoke the dizziness with exam maneuvers.
Orthostasis, cardiac presyncope, vasovagal (pre)syncope, and psychiatric disorders can also cause a vertiginous sensation. History and provocative maneuvers (eg orthostatic vitals) may be helpful.
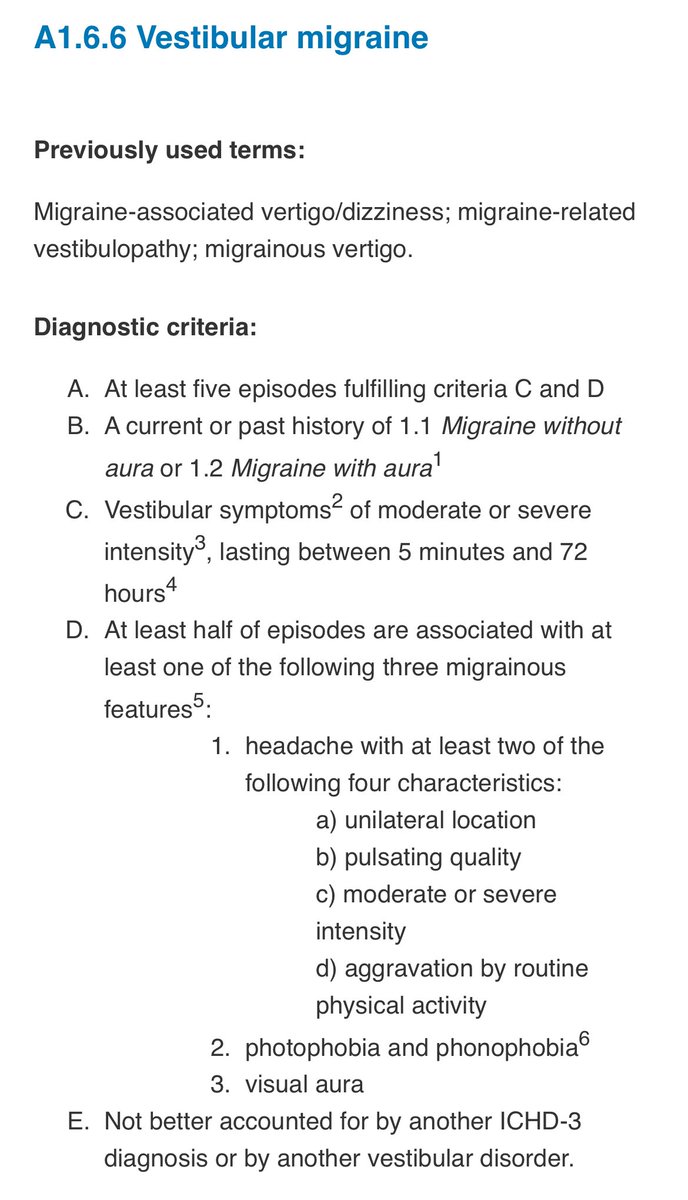
Chronic dizziness is its own entity. Chronic, continuous *vertigo* is usually non-neurologic as the vestibular system should eventually adapt to an insult. Recurrent episodes of vertigo are common though.
Causes of chronic dizziness include:
- Cardiovascular disease
- Anemia
- Perceptual postural-perceptual dizziness
- Peripheral neuropathy
- Hip girdle weakness/instability
- Diplopia/vision problems
- Cardiovascular disease
- Anemia
- Perceptual postural-perceptual dizziness
- Peripheral neuropathy
- Hip girdle weakness/instability
- Diplopia/vision problems
There’s an entire field of neurology devoted to vestibular disorders so I can’t summarize it all in one tweet, so we’ll call it a wrap!
#neurology #MedEd #FOAMed #neurotwitter #tweetorial
#neurology #MedEd #FOAMed #neurotwitter #tweetorial
Special thanks to @AaronLBerkowitz and his book Clinical Neurology and Neuroanatomy: a Localization-Based Approach. I borrowed extremely heavily from his book for this tweetorial! Such a great resource!
Loading suggestions...