(1/x) I use #POCUS almost every day in clinical practice after my #pocus fellowship.
Here's my top tips for anyone learning or using #pocus 👇
(Including how I would learn #pocus if I was starting over without mentorship...)
A 🧵
#medtwitter #foamed #foamcc #echofirst
Here's my top tips for anyone learning or using #pocus 👇
(Including how I would learn #pocus if I was starting over without mentorship...)
A 🧵
#medtwitter #foamed #foamcc #echofirst
Tip 1. Don't get too complicated too quickly - start with solid acquisition
We often talk about a progression of competency for #pocus... this is how it can roughly go.
Indication - what is POCUS good for
Acquisition - how to acquire quality scans
Interpretation - what is normal vs. pathology
Synthesis - how to integrate #pocus with other clinical information.
It is not completely linear and its worth thinking about interpretation/synthesis early on, however, when learning, avoid relying on #pocus heavily while still mastering acquisition
Also, don't start pocus by learning #vexus lol
We often talk about a progression of competency for #pocus... this is how it can roughly go.
Indication - what is POCUS good for
Acquisition - how to acquire quality scans
Interpretation - what is normal vs. pathology
Synthesis - how to integrate #pocus with other clinical information.
It is not completely linear and its worth thinking about interpretation/synthesis early on, however, when learning, avoid relying on #pocus heavily while still mastering acquisition
Also, don't start pocus by learning #vexus lol
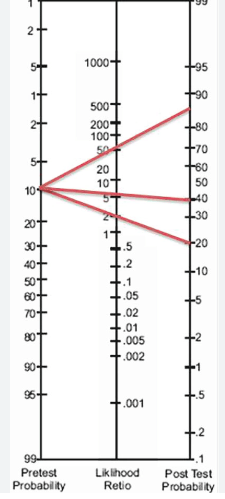
Tip 2. POCUS results are never definitive - they change post-test probability through a Bayesian lens
Now this often stated with a bunch of epidemiology mumbo-jumbo, so here it is simple.
A positive POCUS scan is not definitive - it helps make you be more certain (increases post-test probability) but is not absolute.
Similarly, a negative POCUS scan does not rule out a disease, it simply decreases the likelihood.
Whether you need more testing after a #pocus depends on the baseline likelihood that your patient has the condition, the confidence of your pocus assessment, the treatment options available (and at what threshold you would use them), and the risk of falsely confirming (or ruling out) the disease.
Now this often stated with a bunch of epidemiology mumbo-jumbo, so here it is simple.
A positive POCUS scan is not definitive - it helps make you be more certain (increases post-test probability) but is not absolute.
Similarly, a negative POCUS scan does not rule out a disease, it simply decreases the likelihood.
Whether you need more testing after a #pocus depends on the baseline likelihood that your patient has the condition, the confidence of your pocus assessment, the treatment options available (and at what threshold you would use them), and the risk of falsely confirming (or ruling out) the disease.
Tip 3. B-mode POCUS (no fancy Doppler) gets you 80% of the way there.
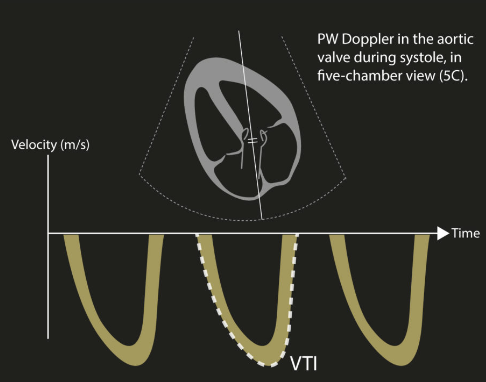
LVOT VTI + VEXUS gets you 90% of the way there...
The biggest difference between B-mode and Doppler is structure vs. function.
EF estimation is useful, however, for the patient in front of you can't tell you if the decreased LV function is acute vs. chronic. Doppler of the LVOT to get a VTI gives you stroke volume, a more actionalable real-time estimate of cardiac function that can help inform hemodynamic interventions.
Similarly, a dilated IVC is helpful, however, does not tell you whether that pressure is being transmitted retrograde to end organs and causing congestion. Doppler of the hepatic, portal, or intra-renal vein can help narrow that
LVOT VTI + VEXUS gets you 90% of the way there...
The biggest difference between B-mode and Doppler is structure vs. function.
EF estimation is useful, however, for the patient in front of you can't tell you if the decreased LV function is acute vs. chronic. Doppler of the LVOT to get a VTI gives you stroke volume, a more actionalable real-time estimate of cardiac function that can help inform hemodynamic interventions.
Similarly, a dilated IVC is helpful, however, does not tell you whether that pressure is being transmitted retrograde to end organs and causing congestion. Doppler of the hepatic, portal, or intra-renal vein can help narrow that
Tip 4. This is how I would learn POCUS completely from scratch without local mentorship 👇
I get asked this a ton in my DMs - how to learn #pocus without support from local mentors.
1. Go to any one of the #foamed ultrasound sites and review basic physics, knobology, cardiac, lung, and abdominal videos to start gaining some familiarity. (e.g. coreultrasound.com)
2. Take a #POCUS course (1 or 2 day) to get some supervsied scans under your belt
3. Integrate #POCUS into your practice within 1 week of the course (if you wait longer you might not get momentum going). Focus only on acquisition and interpretation and not integrating into practice.
4. Review challenging scans / pathology with mentors (remote vs. local). Make sure clips are deidentified.
5. Once acquisition solid, start integrating core scans into practice and start focusing more on interpretation and synthesis.
6. Develop mastery and see the benefit to your patients!
I get asked this a ton in my DMs - how to learn #pocus without support from local mentors.
1. Go to any one of the #foamed ultrasound sites and review basic physics, knobology, cardiac, lung, and abdominal videos to start gaining some familiarity. (e.g. coreultrasound.com)
2. Take a #POCUS course (1 or 2 day) to get some supervsied scans under your belt
3. Integrate #POCUS into your practice within 1 week of the course (if you wait longer you might not get momentum going). Focus only on acquisition and interpretation and not integrating into practice.
4. Review challenging scans / pathology with mentors (remote vs. local). Make sure clips are deidentified.
5. Once acquisition solid, start integrating core scans into practice and start focusing more on interpretation and synthesis.
6. Develop mastery and see the benefit to your patients!
Tip 5. If you take care of patients with shock, learn and understand the LVOT VTI
The LVOT VTI gives you an estimate of stroke volume. When managing shock, this is crucial as it can distinguish between high output and low output shock states.
It is easy to learn, repeatable, and we see success with all of our rotators going through our #pocus rotation
The LVOT VTI gives you an estimate of stroke volume. When managing shock, this is crucial as it can distinguish between high output and low output shock states.
It is easy to learn, repeatable, and we see success with all of our rotators going through our #pocus rotation
Loading suggestions...