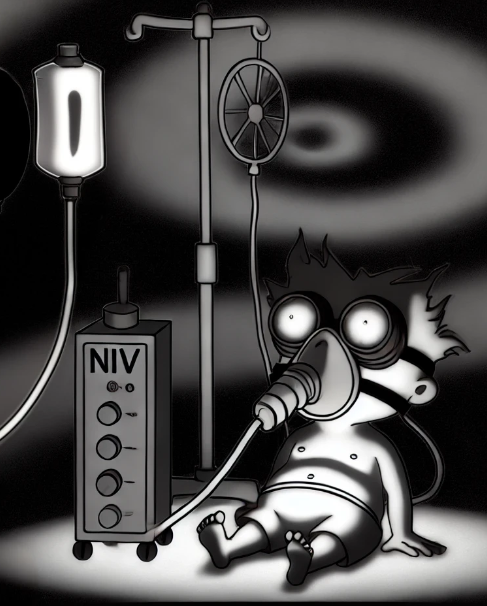
(1/x) Can you use BIPAP for patients with neuromuscular weakness (e.g. myasthenia) instead of intubating them?🧠🧠
Most textbook answers to when to intubate (20-30-40 rule etc.) are gross oversimplifications.
In our ICU (with the help of our chronic vent team) we sometimes use non-invasive ventilation for weeks.
Here's how 🧵
#medtwitter #foamed #Neurology
Most textbook answers to when to intubate (20-30-40 rule etc.) are gross oversimplifications.
In our ICU (with the help of our chronic vent team) we sometimes use non-invasive ventilation for weeks.
Here's how 🧵
#medtwitter #foamed #Neurology
(2/x) First, this is a super nuanced topic and this thread is not medical advice nor am I advocating for this for every patient! Its use is appropriate for select patients. Decisions regarding this should be approached with a multi-disciplinary team of ICU, neurology, RTs, RNs etc. and requires a team approach to make successful.
My approach to this topic has changed a lot in the past few years, largely from learning from experts in our chronic ventilation unit/clinic.
There is a myth that after 24 hours of non-invasive ventilation a patient needs to be intubated. We have patients who are on NIV for years chronically with ALS or other neuromuscular conditions.
So why don't they need to be intubated?
My approach to this topic has changed a lot in the past few years, largely from learning from experts in our chronic ventilation unit/clinic.
There is a myth that after 24 hours of non-invasive ventilation a patient needs to be intubated. We have patients who are on NIV for years chronically with ALS or other neuromuscular conditions.
So why don't they need to be intubated?
(3/x) To understand how you can non-invasively ventilate a patient for years, it is important to think about the differences between an endotracheal tube and well fitting NIV mask.
The main difference? A plastic tube into the lungs that allows for pulmonary toilet (clearing secretions).
The problem with neuromuscular weakness is many patients have impaired secretion clearance (oral and pulmonary) and weak or absent cough. These patients, if left on NIV without attempts at pulmonary toilet, WILL FAIL. FULL STOP.
The solution? Cough assist and excellent chest physio.
The main difference? A plastic tube into the lungs that allows for pulmonary toilet (clearing secretions).
The problem with neuromuscular weakness is many patients have impaired secretion clearance (oral and pulmonary) and weak or absent cough. These patients, if left on NIV without attempts at pulmonary toilet, WILL FAIL. FULL STOP.
The solution? Cough assist and excellent chest physio.
(4/x) In a patient with neuromuscular weakness requiring NIV but who is otherwise alert and stable, NIV might be an option IF you have the ability to regularly (4 times per day AND as needed) cough assist the patient to help them expectorate secretions and treat atelectasis.
With this regime, we have been able to manage patients with myasthenia or diaphragmatic dysfunction for weeks without intubation.
The advantage? You can avoid the potential harms of sedation, a foreign body in the trachea (and the risk of pneumonia), and can better mobilize the patient.
With this regime, we have been able to manage patients with myasthenia or diaphragmatic dysfunction for weeks without intubation.
The advantage? You can avoid the potential harms of sedation, a foreign body in the trachea (and the risk of pneumonia), and can better mobilize the patient.
(5/x) So what is needed to chronically use NIV in patients with neuromuscular weakness? (not an exhaustive list!)
1) A team with expertise in NIV who believes that this approach is best for patients - trust me, intubating the patient is often easier (although not necessarily best for the patient)
2) Multiple NIV mask options to address / prevent skin breakdown and discomfort
3) Amazing RT and physio colleagues who can be the patient's cough / secretion clearance
4) Understanding that traditional dogma (20-30-40 rule) is not evidence based, and is simply a heuristic.
5) The ability to respond to deteriorations 24/7. This is logistically harder in ICUs where intubators are not immediately available after hours
1) A team with expertise in NIV who believes that this approach is best for patients - trust me, intubating the patient is often easier (although not necessarily best for the patient)
2) Multiple NIV mask options to address / prevent skin breakdown and discomfort
3) Amazing RT and physio colleagues who can be the patient's cough / secretion clearance
4) Understanding that traditional dogma (20-30-40 rule) is not evidence based, and is simply a heuristic.
5) The ability to respond to deteriorations 24/7. This is logistically harder in ICUs where intubators are not immediately available after hours
(6/x) What are the pitfalls to NIV for neuromuscular weakness? There are a lot to consider.
1. If a patient has profound bulbar dysfunction and complete inability to manage oropharyngeal secretions this is more difficult.
2. If a patient has a lot of pulmonary secretions (pneumonia) this is difficult
3. If a patient develops a complication (e.g. sepsis) then often NIV fails. NIV is good for single system respiratory issues in this setting.
4. If a patient needs multiple tests outside of the ICU this can be more difficult.
5. If the patient has a lot of skin breakdown, this can lead to unacceptable pain.
1. If a patient has profound bulbar dysfunction and complete inability to manage oropharyngeal secretions this is more difficult.
2. If a patient has a lot of pulmonary secretions (pneumonia) this is difficult
3. If a patient develops a complication (e.g. sepsis) then often NIV fails. NIV is good for single system respiratory issues in this setting.
4. If a patient needs multiple tests outside of the ICU this can be more difficult.
5. If the patient has a lot of skin breakdown, this can lead to unacceptable pain.
(7/x) Here are a few tips to using chronic (weeks) NIV for neuromuscular weakness.
1. You need to feed your patients! A small bore feeding tube (we try post-pyloric) shouldn't' impact mask seal.
2. Be proactive about preventing skin breakdown on the face - this can become a limiting step. Start with higher quality NIV masks if available (as opposed to the hard cheap plastic ones)
3. If you are seeing worsening oxygenation, this means you most likely have untreated atelectasis. Don't simply turn up the FiO2, address the atelectasis with cough assist and physio.
4. Obsess about mask seal and leak - NIV only works if you have a good seal. A leak will destroy your PEEP and driving pressure.
Final thoughts. I am not claiming that this is the optimal approach for all patients. It probably is only appropriate for a small subset. Instead, this is a tool that is nice to have in your toolkit for select patients where your multidisciplinary team feels like it will improve outcomes.
1. You need to feed your patients! A small bore feeding tube (we try post-pyloric) shouldn't' impact mask seal.
2. Be proactive about preventing skin breakdown on the face - this can become a limiting step. Start with higher quality NIV masks if available (as opposed to the hard cheap plastic ones)
3. If you are seeing worsening oxygenation, this means you most likely have untreated atelectasis. Don't simply turn up the FiO2, address the atelectasis with cough assist and physio.
4. Obsess about mask seal and leak - NIV only works if you have a good seal. A leak will destroy your PEEP and driving pressure.
Final thoughts. I am not claiming that this is the optimal approach for all patients. It probably is only appropriate for a small subset. Instead, this is a tool that is nice to have in your toolkit for select patients where your multidisciplinary team feels like it will improve outcomes.
(8/x) A great approach and review of this topic is covered by @PulmCrit in his post on Neuromuscular Disorders - a must read chapter of the IBCC.
emcrit.org
Neurocrit guru's out there, curious how your approach differs.
@CritCareWestern @MaratSlessarev @caseyalbin
emcrit.org
Neurocrit guru's out there, curious how your approach differs.
@CritCareWestern @MaratSlessarev @caseyalbin
Loading suggestions...