COPD definition: heterogeneous 🫁 condition characterized by chronic respiratory symptoms (cough, dyspnea, Sputum) due to abnormalities in the airway “bronchitis, bronchiolitis, emphysema” that cause persistent, often progressive airflow obstruction x.com
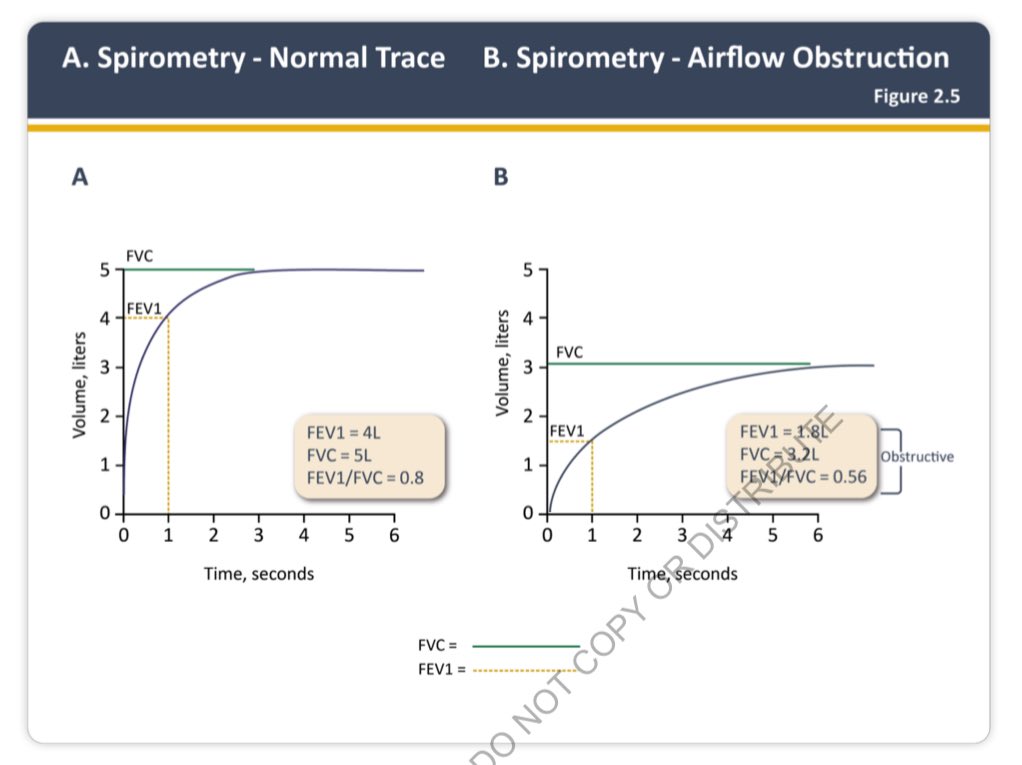
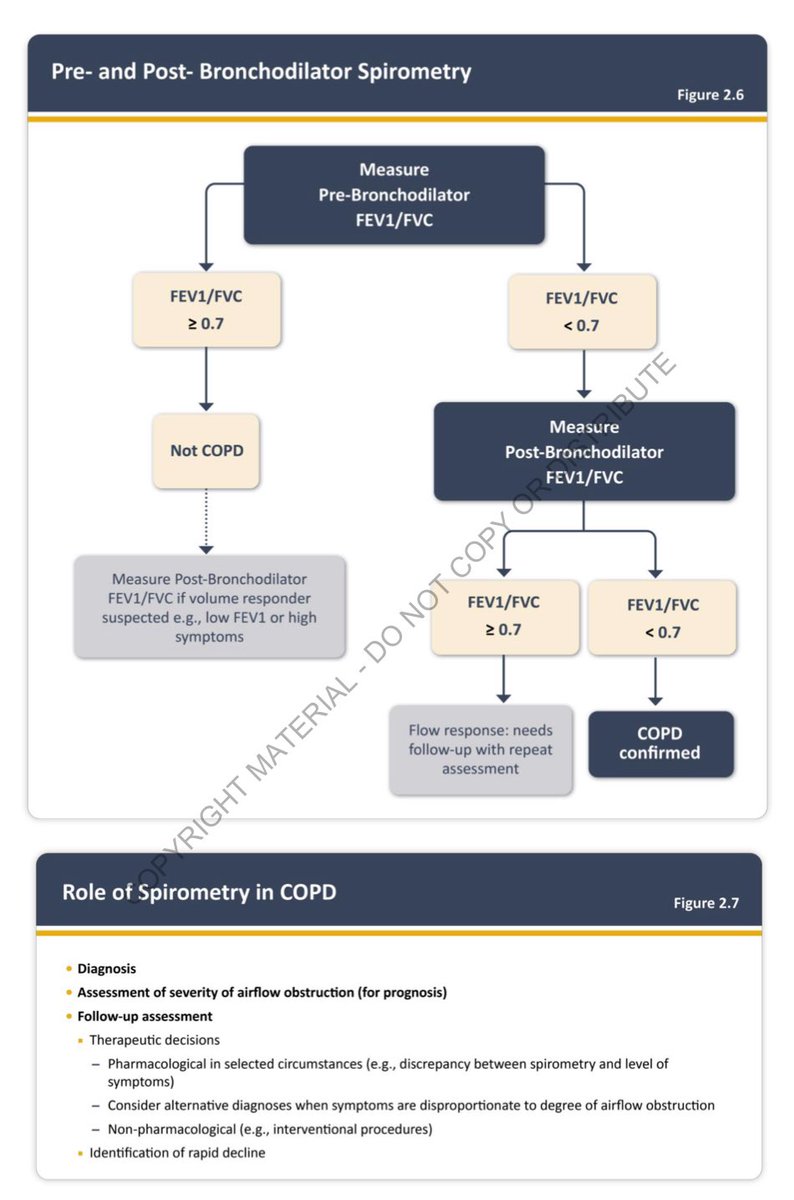
Diagnostic criteria:
Respiratory symptoms (dyspnea, sputum production, chronic cough) + Risk factor + post bronchodilator (FEV1/FVC) < 0.7 (fixed ratio not LLN) x.com
Respiratory symptoms (dyspnea, sputum production, chronic cough) + Risk factor + post bronchodilator (FEV1/FVC) < 0.7 (fixed ratio not LLN) x.com
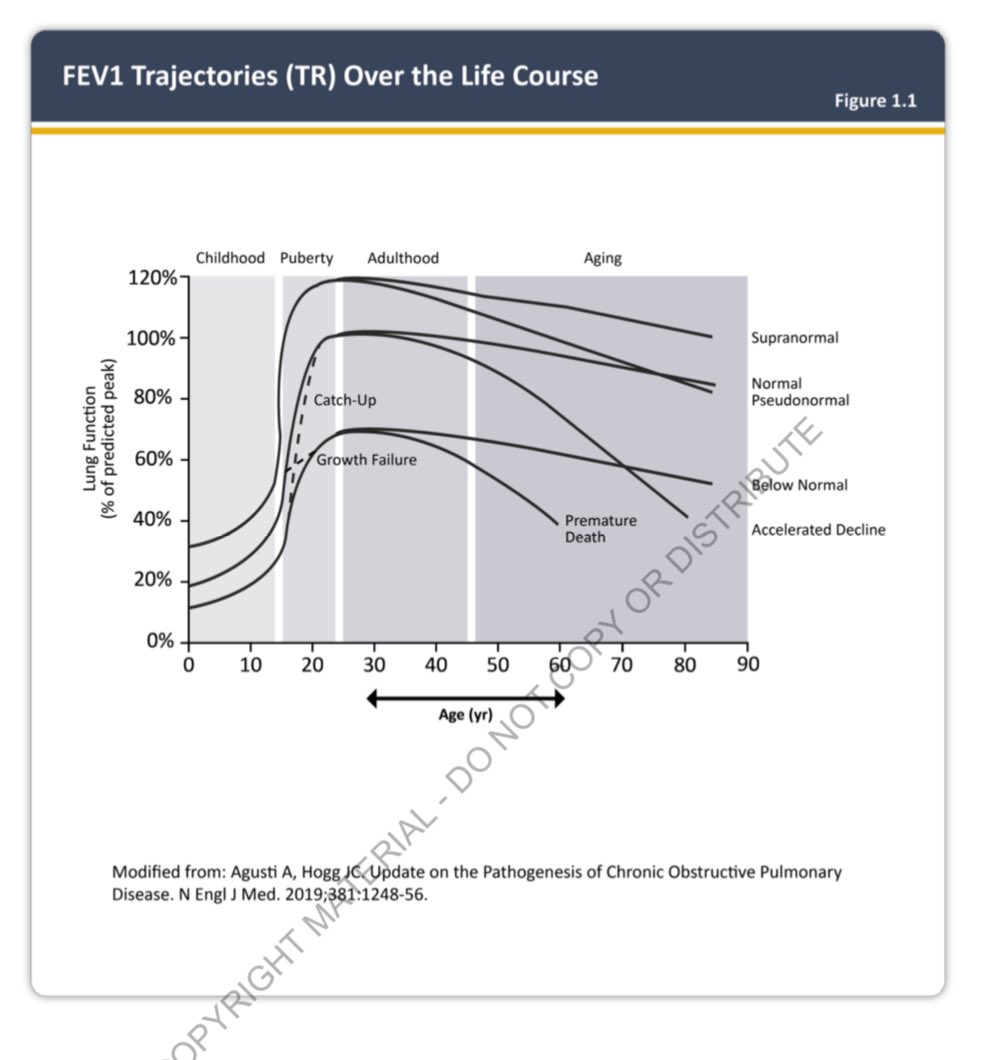
Patients with symptoms, risk factors, hyperinflation, air trapping, and reduced DLCO, but a preserved FEV1/FVC (no obstruction), are classified as Pre-COPD. If FEV1 or FVC are reduced but the ratio is preserved, they fall under PRISM. x.com
Etiotypes of COPD:
• COPD-G: genetic-AATD (SERPINA1 gene mutation)
• COPD-D: development defect
• COPD-C: exposure to tobacco product, Vaping, cannabis
• COPD-P: exposure to pollution
• COPD-A: COPD with Asthma
• COPD-I: due to infection (TB, HIV)
• COPD-U: unknown
• COPD-G: genetic-AATD (SERPINA1 gene mutation)
• COPD-D: development defect
• COPD-C: exposure to tobacco product, Vaping, cannabis
• COPD-P: exposure to pollution
• COPD-A: COPD with Asthma
• COPD-I: due to infection (TB, HIV)
• COPD-U: unknown
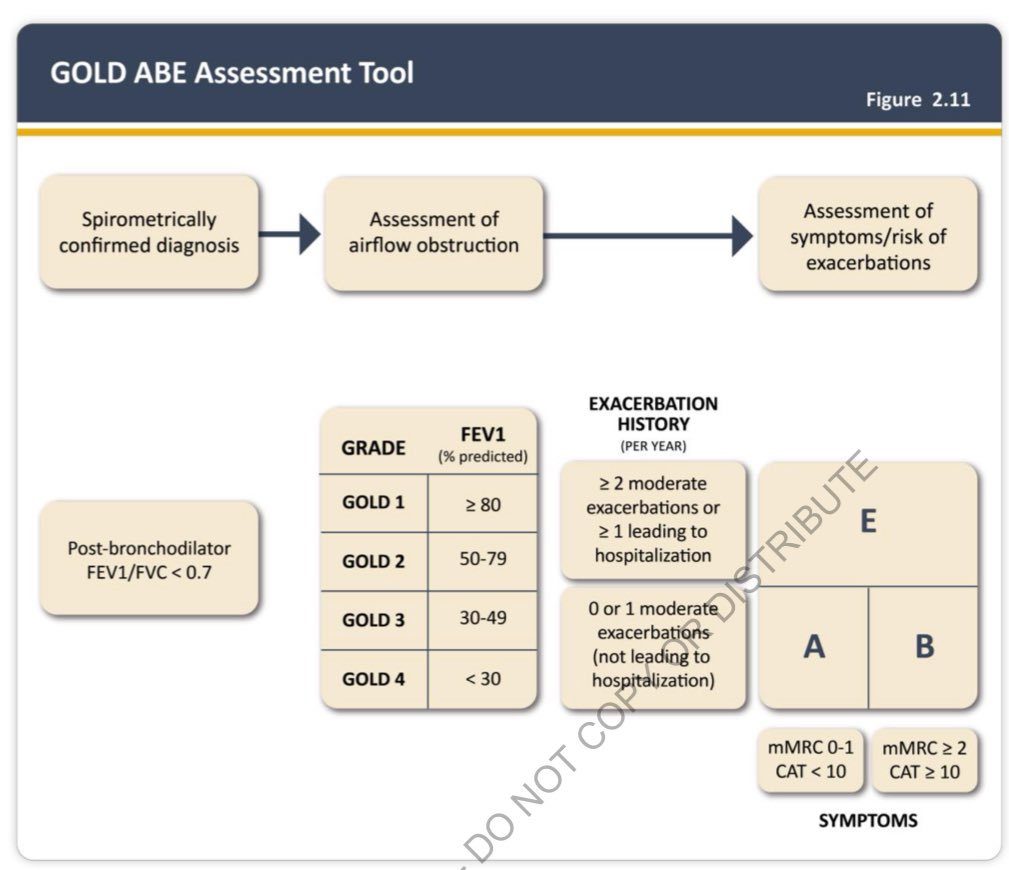
GOLD ABE classification:
GOLD A : mMRC <2, < 2 exacerbation, no Hospitalization
GOLD B : mMRC ≥ 2, < 2 exacerbation, no Hospitalization
GOLD E: ≥ 2 exacerbation, or hospitalization for COPD exacerbation x.com
GOLD A : mMRC <2, < 2 exacerbation, no Hospitalization
GOLD B : mMRC ≥ 2, < 2 exacerbation, no Hospitalization
GOLD E: ≥ 2 exacerbation, or hospitalization for COPD exacerbation x.com
Goal of treatment:
• improve symptoms
• improve exercise tolerance
• improve health status
• prevent disease progression
• prevent and treat exacerbation
• reduce mortality x.com
• improve symptoms
• improve exercise tolerance
• improve health status
• prevent disease progression
• prevent and treat exacerbation
• reduce mortality x.com
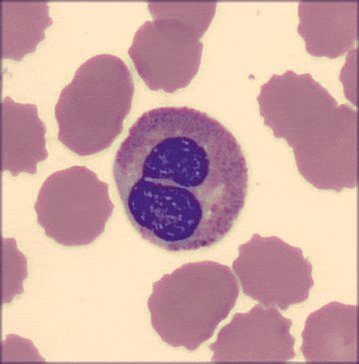
Conduct a CBC with differential for all COPD patients to assess peripheral eosinophil levels, which can guide management and medication choices.
Check alpha-1 antitrypsin (ATT) levels in all COPD patients with emphysema. x.com
Check alpha-1 antitrypsin (ATT) levels in all COPD patients with emphysema. x.com
First step in managing COPD patient:
• Education + education + education
• support your patient to quit smoking 🚬
• prevent exposure if present
• Active life style
• Appropriate vaccinations x.com
• Education + education + education
• support your patient to quit smoking 🚬
• prevent exposure if present
• Active life style
• Appropriate vaccinations x.com
Vaccinations for COPD Patients:
•Annual influenza vaccine
•SARS-CoV-2 vaccine per CDC guidelines
•One dose of PCV20 or PCV21
•RSV vaccine for patients >60 years old, and Zoster vaccine for those >50 years old
•Tdap if not previously administered during adolescence x.com
•Annual influenza vaccine
•SARS-CoV-2 vaccine per CDC guidelines
•One dose of PCV20 or PCV21
•RSV vaccine for patients >60 years old, and Zoster vaccine for those >50 years old
•Tdap if not previously administered during adolescence x.com
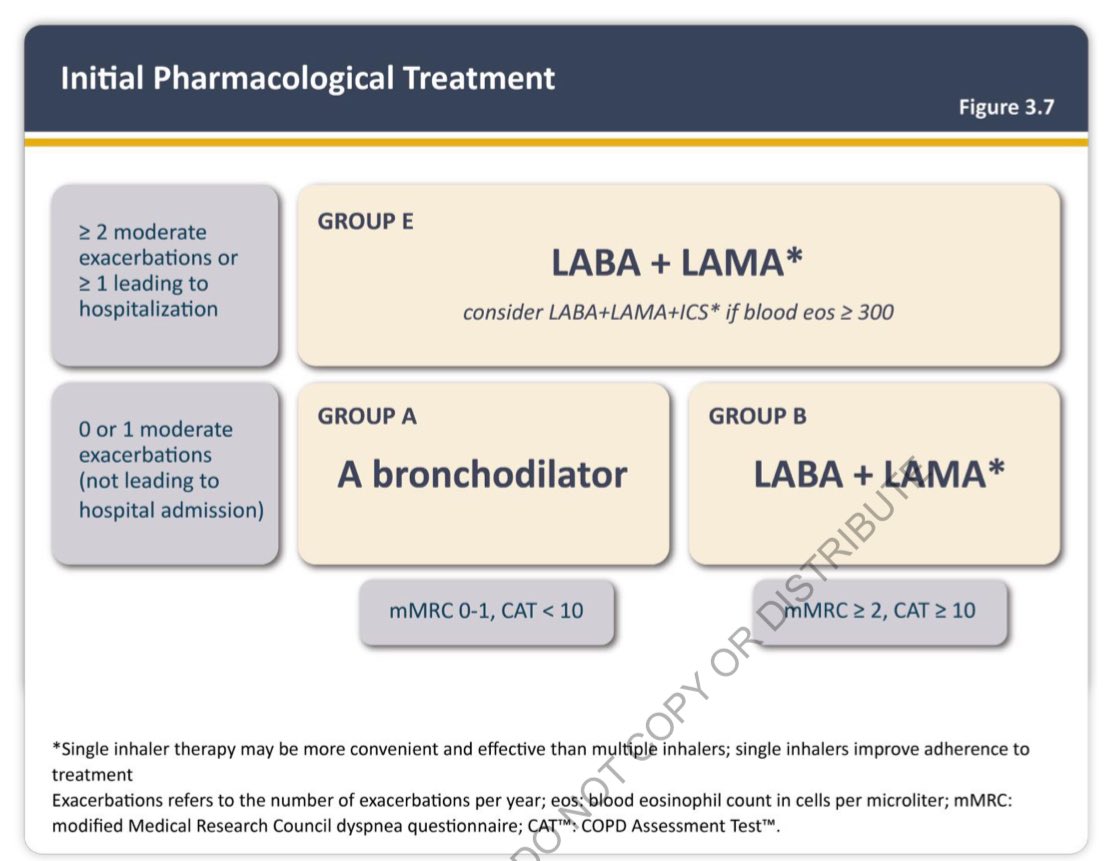
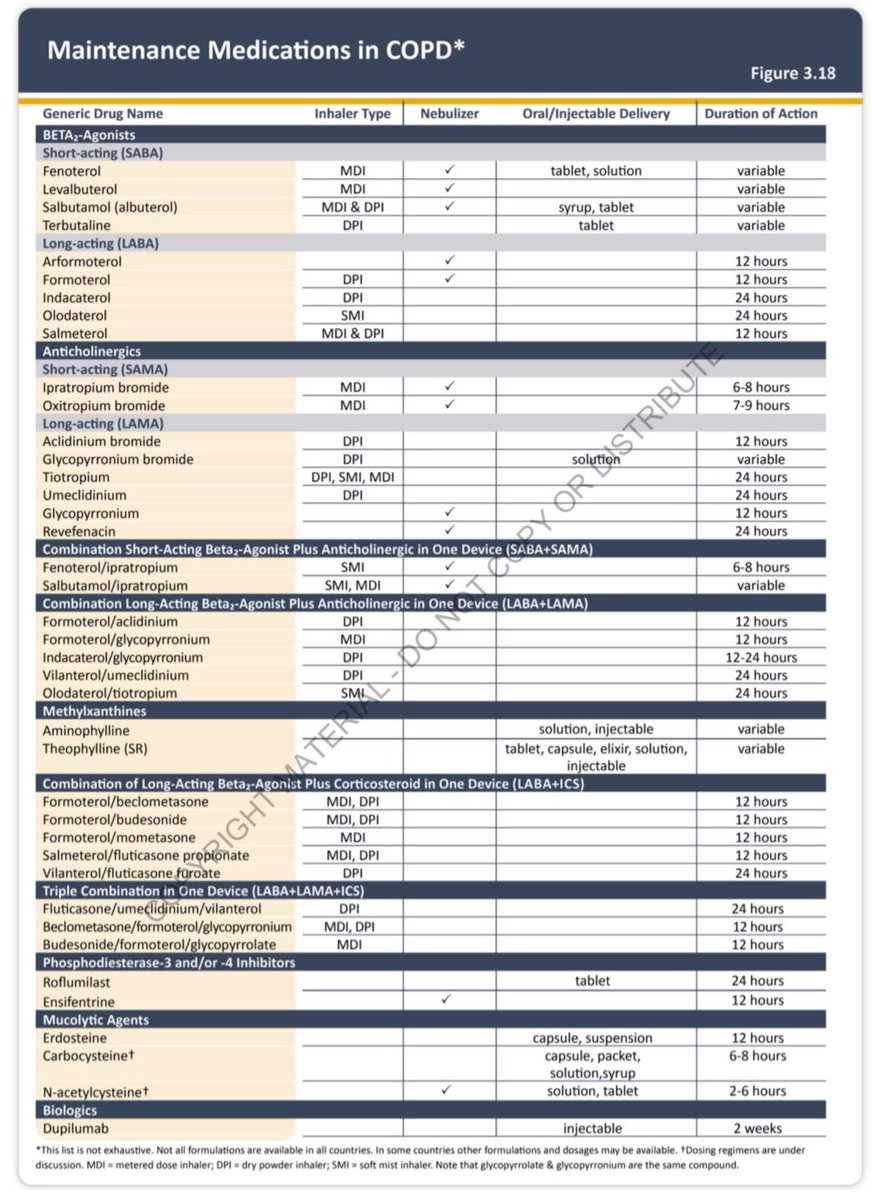
Pharmacological treatment!
Technique is very important!!!!!!!!
GOLD-A : LAMA or LABA
GOLD-B: LABA + LAMA
GOLD-E: LABA + LAMA + ICS if peripheral eosinophils ≥ 300 cell/ul x.com
Technique is very important!!!!!!!!
GOLD-A : LAMA or LABA
GOLD-B: LABA + LAMA
GOLD-E: LABA + LAMA + ICS if peripheral eosinophils ≥ 300 cell/ul x.com
When can I add ICS in COPD patient?
• History of hospitalization from COPD
• ≥ 2 exacerbation per year
• ≥ 300 eosinophils
• Why not ICS for everyone because evidence showed ICS can increase pneumonia in severe disease.
• History of hospitalization from COPD
• ≥ 2 exacerbation per year
• ≥ 300 eosinophils
• Why not ICS for everyone because evidence showed ICS can increase pneumonia in severe disease.
If a patient is came to my clinic on LABA + ICS what should I do?
•If well-controlled (no relevant exacerbation history, no asthma): Switch to LABA + LAMA.
•If experiencing exacerbations with eosinophils <100: Switch to LABA + LAMA. If > 100 consider adding LAMA
•If well-controlled (no relevant exacerbation history, no asthma): Switch to LABA + LAMA.
•If experiencing exacerbations with eosinophils <100: Switch to LABA + LAMA. If > 100 consider adding LAMA
If a patient is came to my clinic on LABA + ICS what should I do?
• No current exacerbation with hx of positive response to bronchodilator and low symptoms load - continue LABA + ICS
•
• No current exacerbation with hx of positive response to bronchodilator and low symptoms load - continue LABA + ICS
•
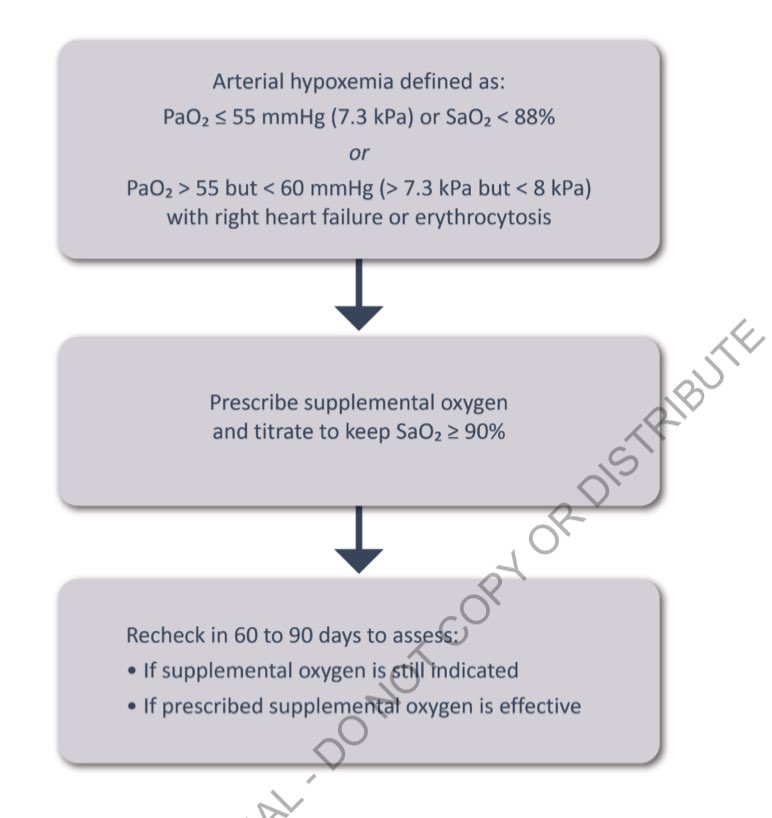
Treatment affect mortality:
• triple therapy when it’s indicated
• smoking cessation
• pulmonary rehabilitation within 4 wks post discharge
• long term oxygen therapy
• BPAP in stable COPD with persistent Hypercapnia
• Lung volume reduction if indicated x.com
• triple therapy when it’s indicated
• smoking cessation
• pulmonary rehabilitation within 4 wks post discharge
• long term oxygen therapy
• BPAP in stable COPD with persistent Hypercapnia
• Lung volume reduction if indicated x.com
On top of the education, smoking cessation, maximum inhalers, vaccinations, active lifestyle what can we do to decrease the chance of exacerbation
When should we use PDE inhibitors?
severe COPD with history of exacerbation in the previous year despite appropriate therapy
Roflumilast improves lung function and reduce moderate and severe exacerbation
severe COPD with history of exacerbation in the previous year despite appropriate therapy
Roflumilast improves lung function and reduce moderate and severe exacerbation
What’s about long term Azithromycin?
Preferably in former smoker with recurrent exacerbation despite appropriate therapy
Azithromycin reduce exacerbation but can lead to hearing deficits and possible bacterial resistance
Preferably in former smoker with recurrent exacerbation despite appropriate therapy
Azithromycin reduce exacerbation but can lead to hearing deficits and possible bacterial resistance
What biological agent yes we can use Dupilumab in severe COPD with history of exacerbation and high eosinophilia > 300 cell/ul
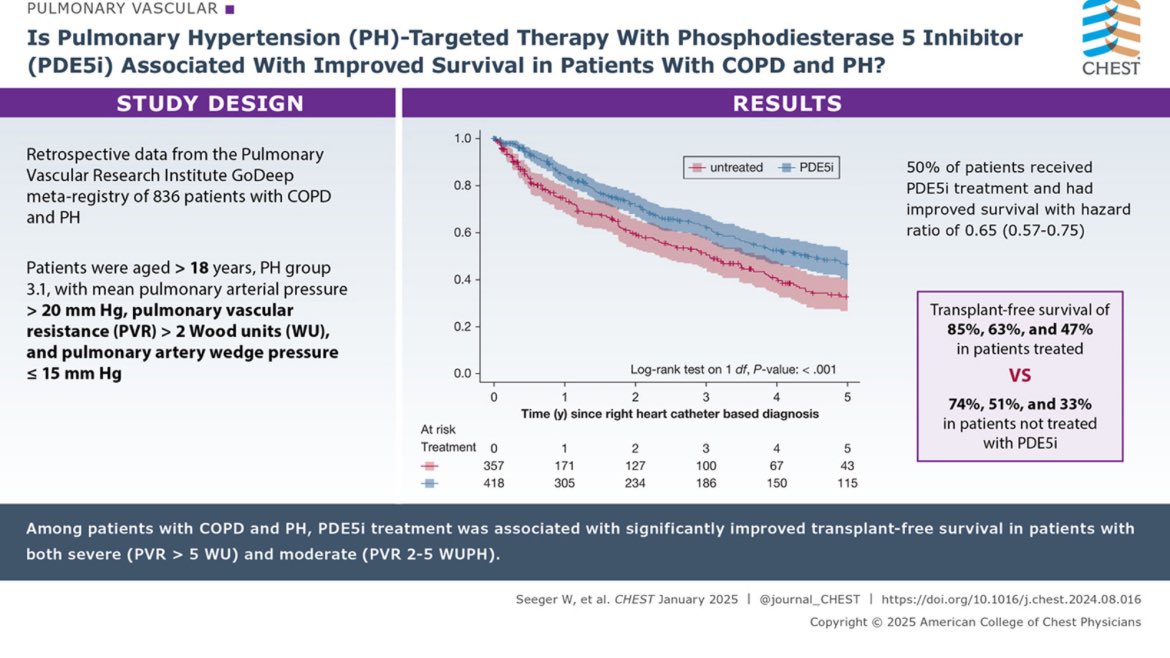
What’s about Pulmonary hypertension (WHO 3) with COPD exhibit poor transplant-free survival, with PVR being a predictor of mortality. PDE5i therapy was associated with a significant reduction in mortality x.com
Let’s strive to be strong advocates for COPD patients and their families.
Remember, if you’ve done everything & the patient is still deteriorating, it’s always wise to seek a fresh perspective, ask transplant team evaluation, and involve the support of palliative care colleagues
Remember, if you’ve done everything & the patient is still deteriorating, it’s always wise to seek a fresh perspective, ask transplant team evaluation, and involve the support of palliative care colleagues
Loading suggestions...