Based off of Run the List Episode 24, here is a #tweetorial on💘Tachyarrhythmias💘
🎧Full episode: bit.ly
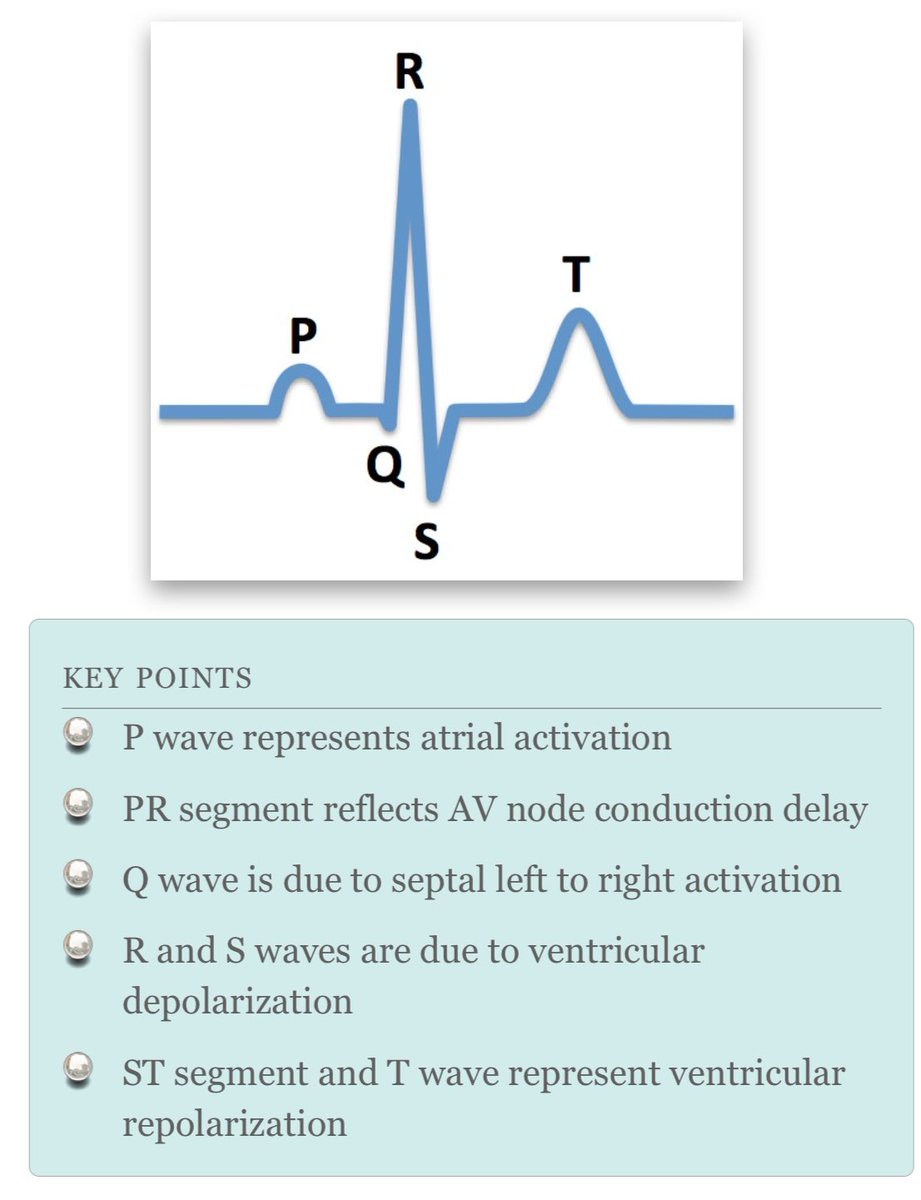
Let's start with an EKG 👇 (@medicine_strong). For more practice, check out: bit.ly
Thanks to @Gurleen_Kaur96 for this week's edition!
🎧Full episode: bit.ly
Let's start with an EKG 👇 (@medicine_strong). For more practice, check out: bit.ly
Thanks to @Gurleen_Kaur96 for this week's edition!
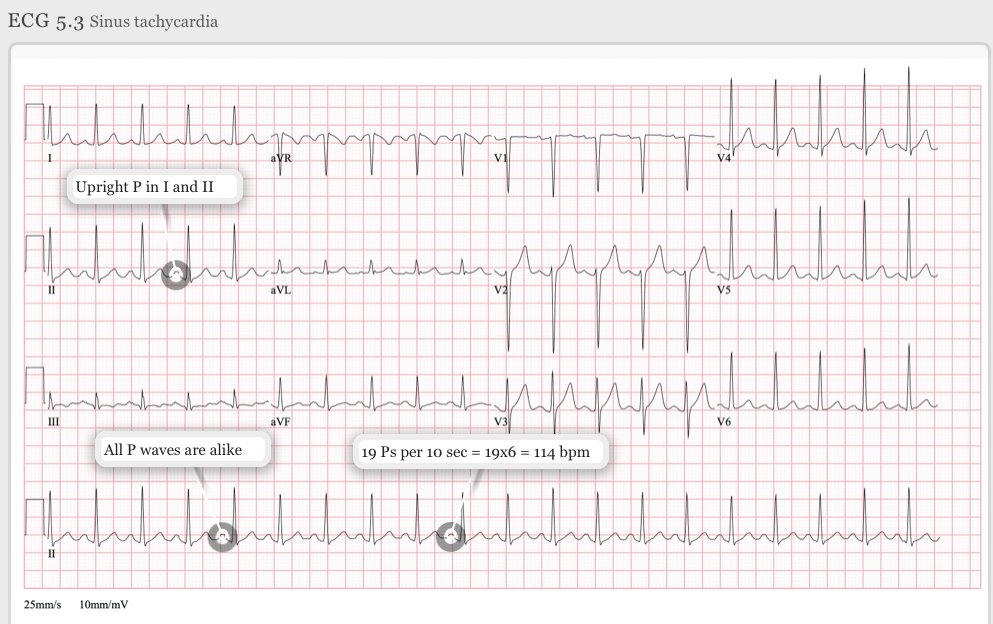
❓What tachyarrhythmia is shown on that EKG above❓
Keep these things in mind when interpreting:
🔶Rate
🔶Regularity
🔶Width of QRS complex
🔶Relationship of P wave to QRS complex
And continue reading this 🧵 for the correct answer...
Keep these things in mind when interpreting:
🔶Rate
🔶Regularity
🔶Width of QRS complex
🔶Relationship of P wave to QRS complex
And continue reading this 🧵 for the correct answer...
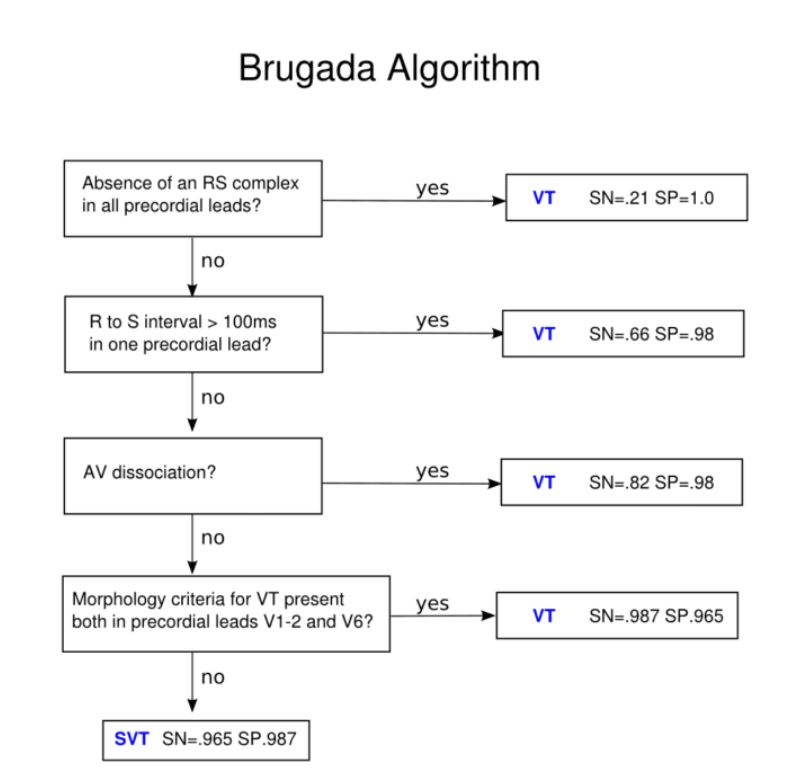
🧠Let's develop a diagnostic framework for tachyarrhythmias
QRS complex on EKG is 💯
🔹Narrow complex (QRS <120ms): SVT
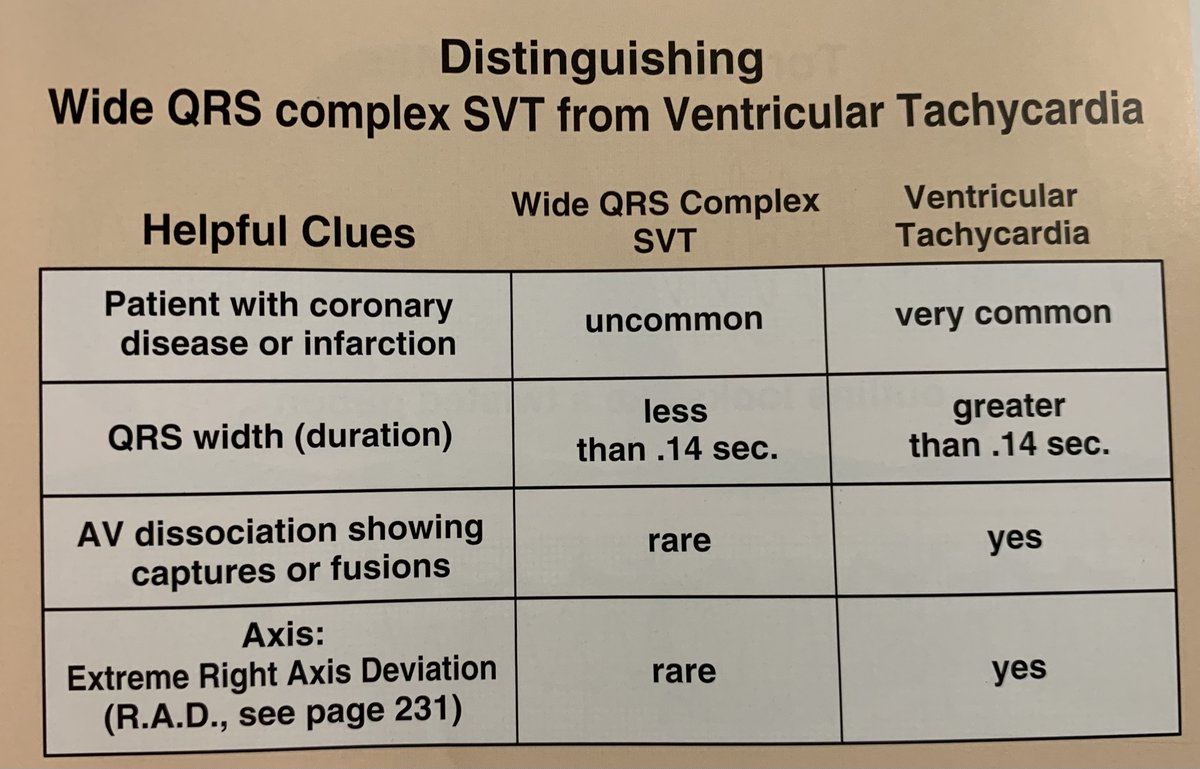
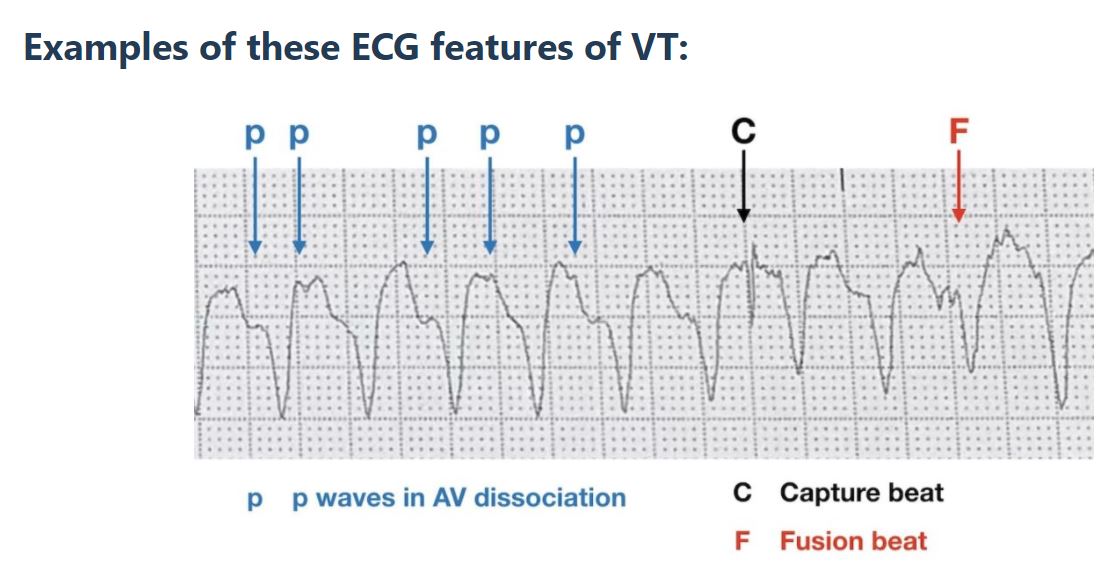
🔷Wide complex (QRS >120ms): SVT w/ aberrancy or ventricular tachycardia (V. tach)
Check out this ⤵️schema from @CPSolvers
QRS complex on EKG is 💯
🔹Narrow complex (QRS <120ms): SVT
🔷Wide complex (QRS >120ms): SVT w/ aberrancy or ventricular tachycardia (V. tach)
Check out this ⤵️schema from @CPSolvers
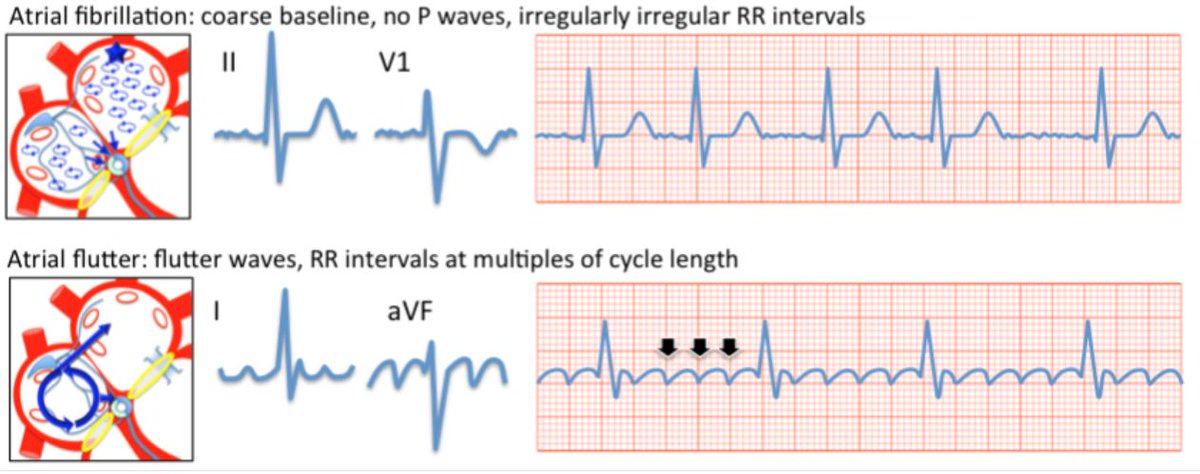
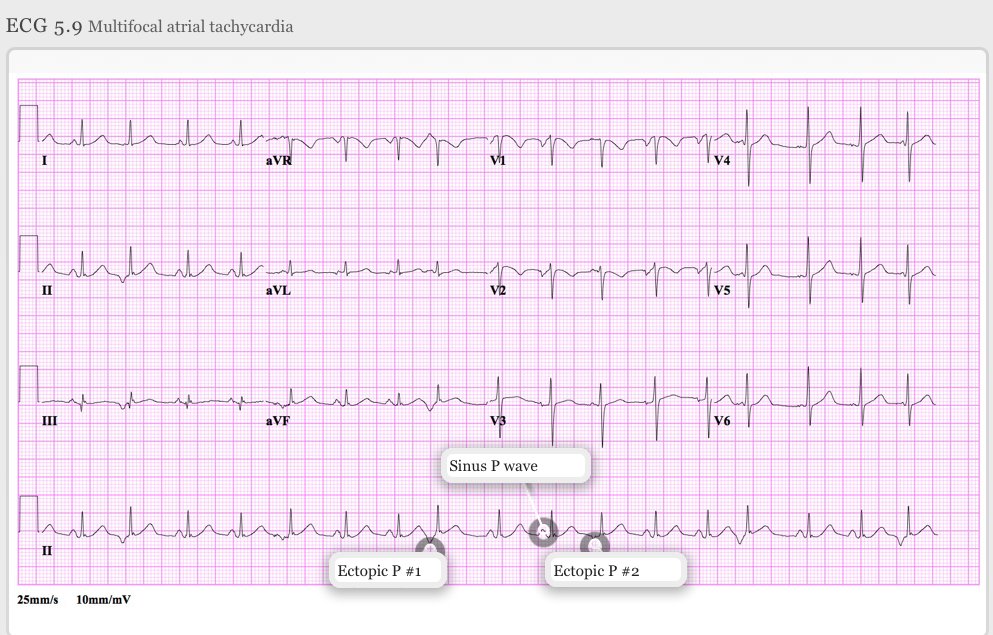
For *narrow* complex, next determine if irregular or regular
RTL schema by @haematognomist ⤵️
--
Ways to differentiate?
🪚Sawtooth pattern in inferior leads – A flutter
🌌Ectopic p wave – Atrial tachycardia
❎No p waves – A fib
🌈Irregularly regular, 3+ p waves – MAT
RTL schema by @haematognomist ⤵️
--
Ways to differentiate?
🪚Sawtooth pattern in inferior leads – A flutter
🌌Ectopic p wave – Atrial tachycardia
❎No p waves – A fib
🌈Irregularly regular, 3+ p waves – MAT
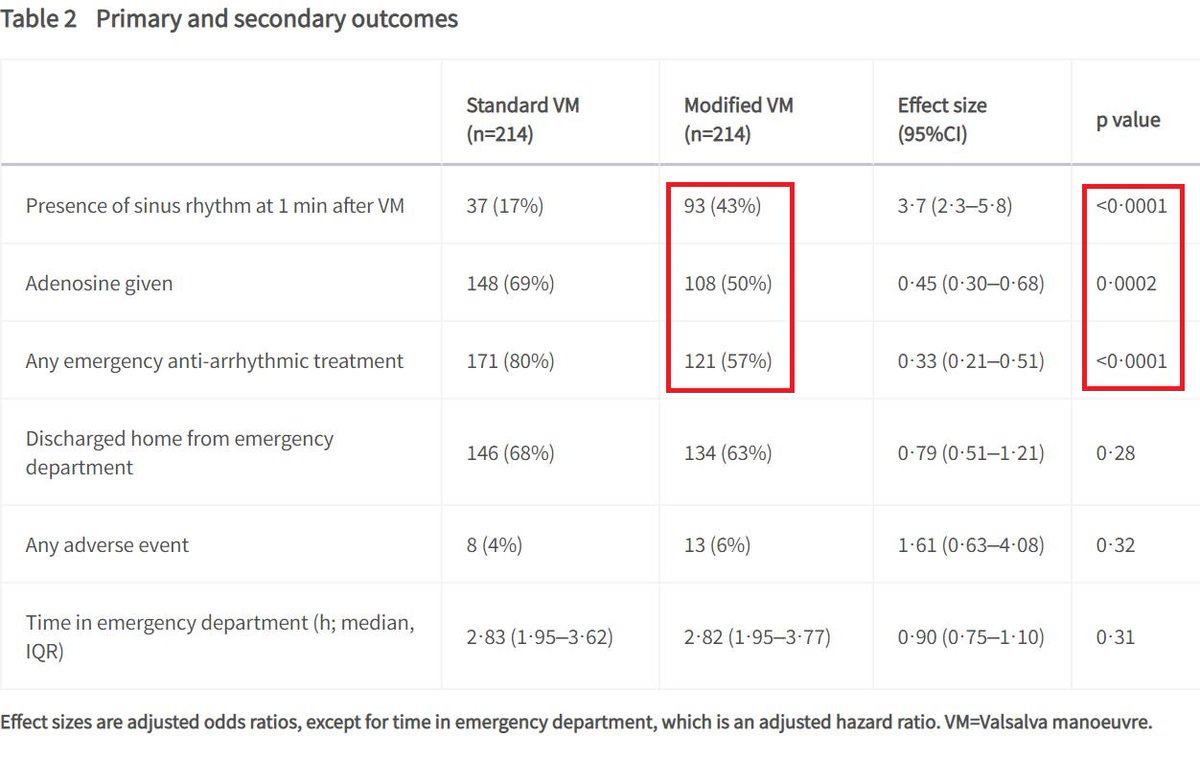
⁉️ Modified Valsalva ⁉️
The REVERT study from 🇬🇧 randomized patients presenting w/ SVT to either modified or standard Valsalva
Conclusion:
-Modified Valsalva should be considered as first-line treatment!
Video of Modified Valsalva: bit.ly
The REVERT study from 🇬🇧 randomized patients presenting w/ SVT to either modified or standard Valsalva
Conclusion:
-Modified Valsalva should be considered as first-line treatment!
Video of Modified Valsalva: bit.ly
💥Summary/pearls for Tachyarrhythmias💥
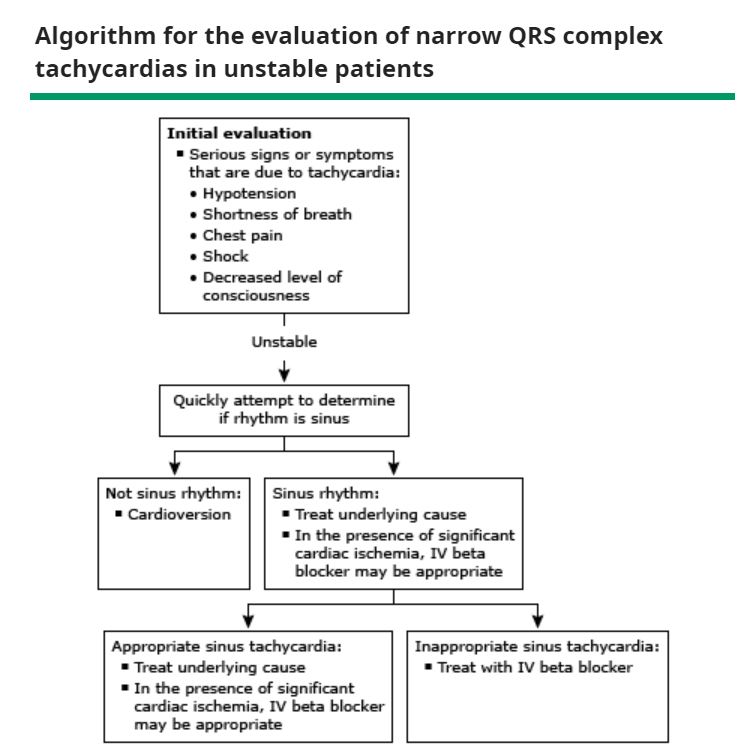
1. Assess hemodynamic instability
2. EKG is 🗝️ - wide or narrow QRS
3. If narrow, determine if regular or irregular rhythm
Other labs/imaging: BMP, TSH, Troponin, BNP, urine toxicology, Echo
RTL Episode Handout: bit.ly
1. Assess hemodynamic instability
2. EKG is 🗝️ - wide or narrow QRS
3. If narrow, determine if regular or irregular rhythm
Other labs/imaging: BMP, TSH, Troponin, BNP, urine toxicology, Echo
RTL Episode Handout: bit.ly
REFs (1/3):
[1,8]youtube.com
[3]uptodate.com
[4,7,10] Mikhail Torosoff & Steven A. Fein. "I Read ECGs An interactive practical guide to the electrocardiogram interpretation".
[5]clinicalproblemsolving.com
[6]litfl.com
[1,8]youtube.com
[3]uptodate.com
[4,7,10] Mikhail Torosoff & Steven A. Fein. "I Read ECGs An interactive practical guide to the electrocardiogram interpretation".
[5]clinicalproblemsolving.com
[6]litfl.com
REFs (2/3):
[6]Dale Dubin "Rapid Interpretation of EKGs". 6th edition.
[7] litfl.com
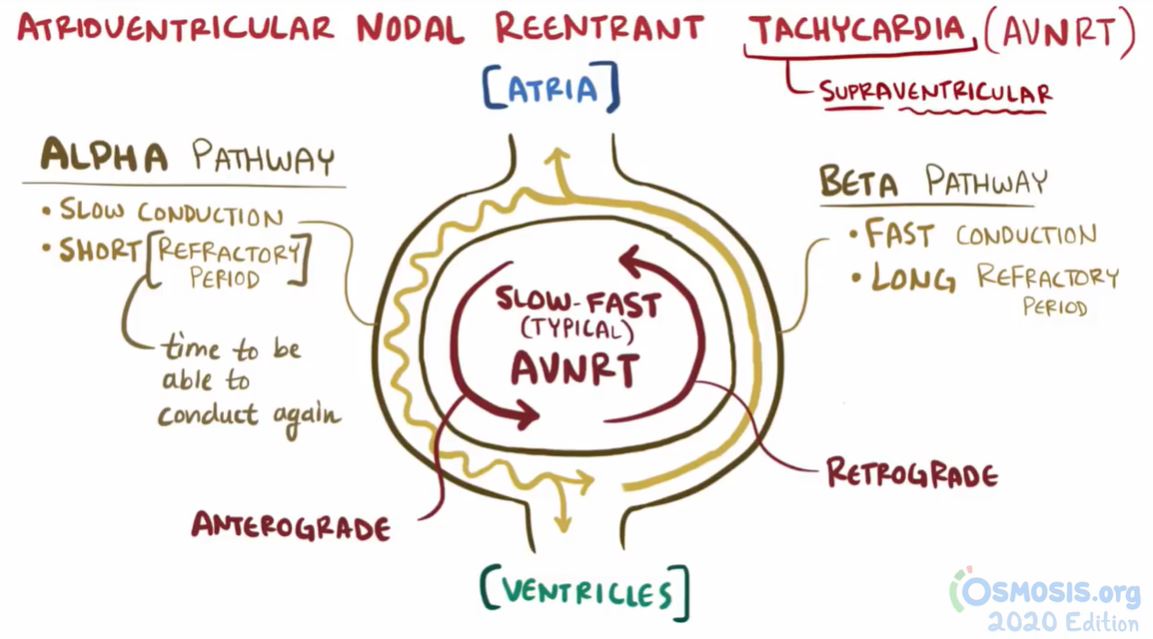
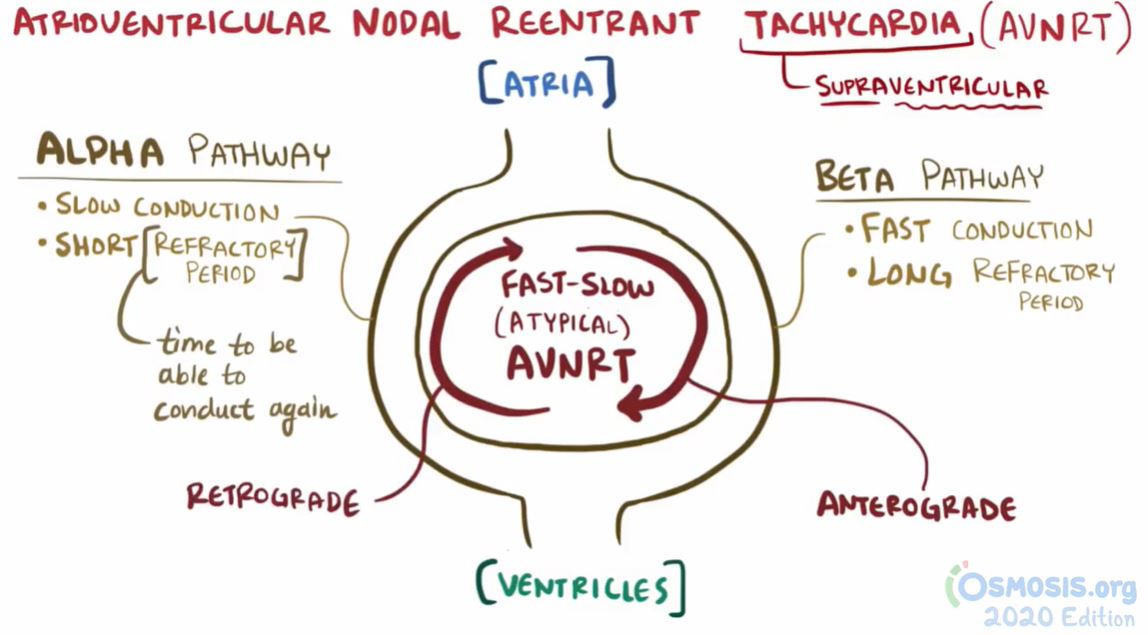
[9]osmosis.org
[9]litfl.com
[9]aafp.org
[6]Dale Dubin "Rapid Interpretation of EKGs". 6th edition.
[7] litfl.com
[9]osmosis.org
[9]litfl.com
[9]aafp.org
REFs (3/3):
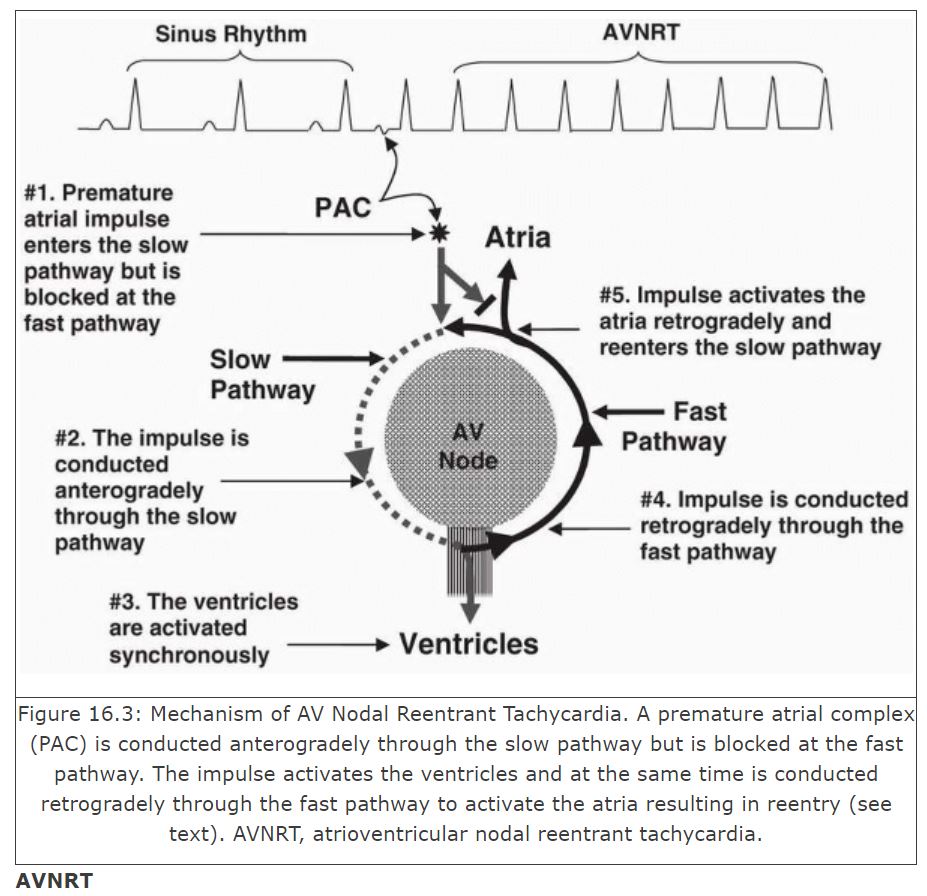
[9] Baltazar RF. Supraventricular Tachycardia due to Reentry. In: Basic and Bedside Electrocardiography. 1st ed.; 2009. doctorlib.info.
[10]ucsfmed.wordpress.com
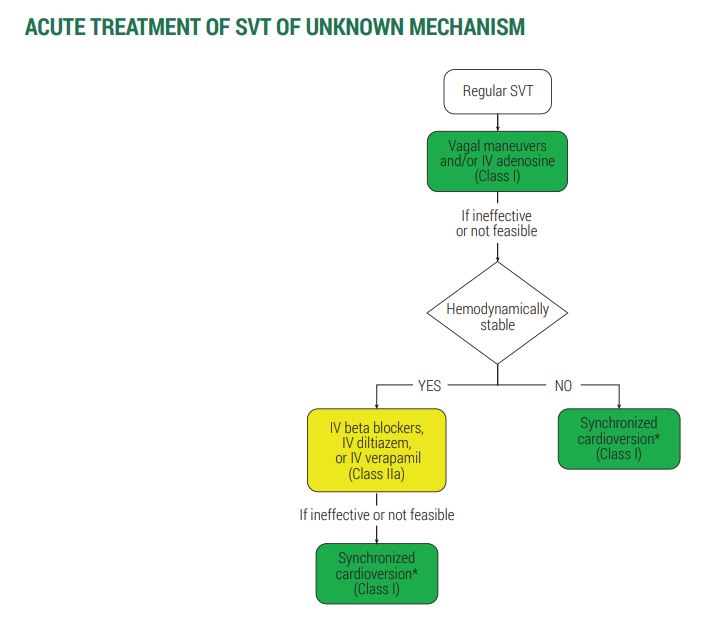
[11,13]ahajournals.org
[12]thelancet.com
[9] Baltazar RF. Supraventricular Tachycardia due to Reentry. In: Basic and Bedside Electrocardiography. 1st ed.; 2009. doctorlib.info.
[10]ucsfmed.wordpress.com
[11,13]ahajournals.org
[12]thelancet.com
thelancet.com/journals/lance…
Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial
In patients with supraventricular tachycardia, a modified Valsalva manoeuvre with leg elevation and...
doctorlib.info/cardiology/ele…
ucsfmed.wordpress.com/2017/07/18/mof…
ahajournals.org/doi/full/10.11…
Loading suggestions...