ICU stories: Elderly pt w PMHx of CAD/COPD/CKD/DM2/cirrhosis c/b esoph varices + ascites requiring paracentesis (most recent a week earlier)/anemia of chronic dz/”etc” presented to the ED w 1-2 ds of falls/weakness/headache/hip and elbow pain. Vitals: BP 93/58, hr 80, afebrile.
Labs: WBC: 9.9K, Hb 7.7, PLT 83, INR 2.2, creat 2.1, TBil 3.0, Na 130. Alb 2.2. CT brain and c-spine: (-) for acute pathology. XRs (-) for fracture. Due to low Hb and SBP in 80s, despite 2 l of NS, decision was made to admit the pt for blood transfusion. There were no inpt beds,
and pt remained in the ED. The next 4 h, another 3 l of NS were given and eventually a RRT was called for “hypotension”. The ICU charge nurse responded; she called me saying that the patient “did not look good”; SBP was 57/36…
If there were 3 things (imagine you had 3 “wishes”...) to ask your RRT to do before bringing the pt to the ICU, what would you choose?
My main concern was that this multimorbid/cirrhotic pt was either septic or bleeding (from the GI tract or intra-abd/abd wall from recent paracentesis). So, under the condition that all could be performed in a reasonable time frame (15 min),
I asked for:
1. STAT peripheral vasopressors (it is not good to leave someone hypotensive),
2. CT (I was looking for hematoma or septic source) , and
3. NGT w gastric lavage (to r/o upper GI bleed)
1. STAT peripheral vasopressors (it is not good to leave someone hypotensive),
2. CT (I was looking for hematoma or septic source) , and
3. NGT w gastric lavage (to r/o upper GI bleed)
When pt arrived to the ICU 20 min later, he was “actively dying”… At least, gastric lavage was (-) for bleeding and NGT was removed. Pt was on neosynephrine 1.5 and SBP was 65; he was mottled and drowsy with significant ascites.
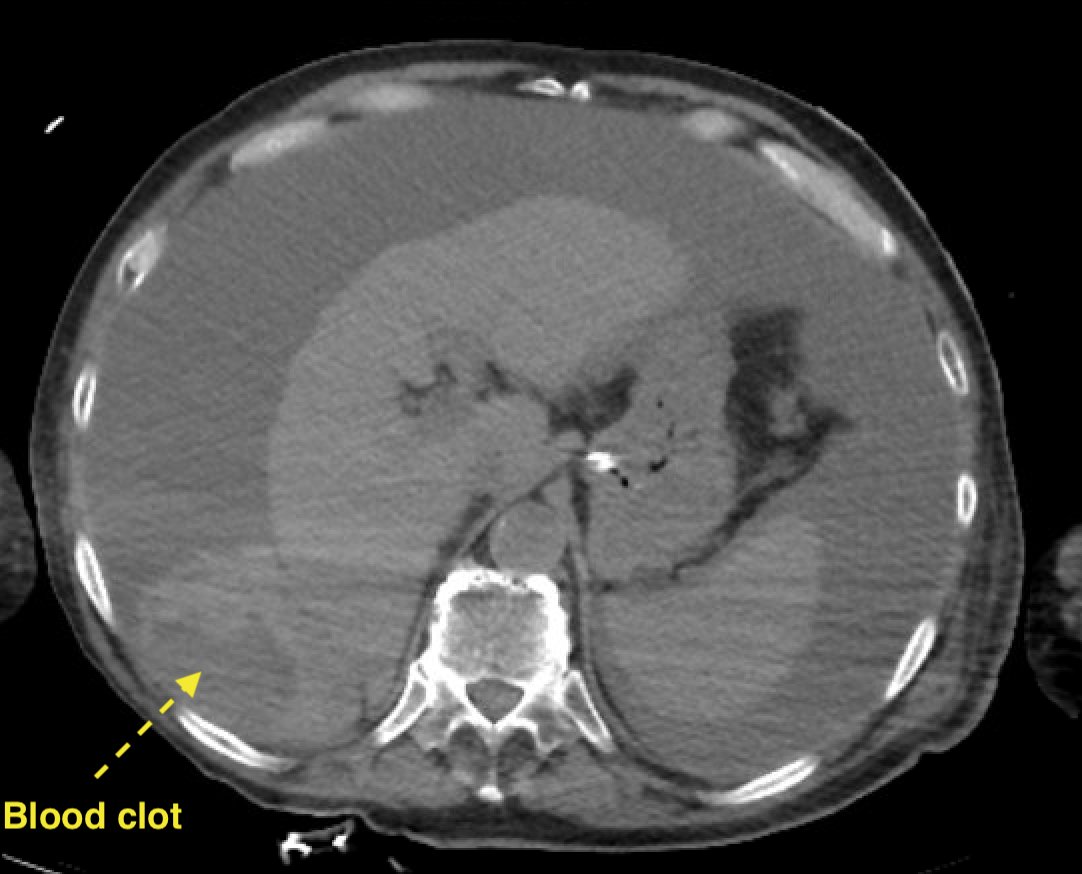
Neo gtt was immediately changed to levo 0.4 + vaso 0.12… A 5 sec POCUS showed hyperdynamic LV and ascites. I placed femoral central + arterial lines and sent vbg / labs / blood cultures. When I tapped the abdomen, I aspirated dark bloody fluid 😱
I was pretty sure that it was not from my tap because I had checked for the presence of vessels in the needle path. While I was finishing the paracentesis, the radiologist called to report that
We had the diagnosis “hemoperitoneum” but not the cause of it. I ordered blood/blood products. Would you order anything else? I have to confess that I have very low threshold giving antibiotics + stress steroids (remember the hepatoadrenal syndrome? PMID: 23382623) to cirrhotics.
What if the pt had SBP? Ascitic fluid mixed w blood will likely have increased WBC, so it's hard to r/o SBP in this setting (this pt had ascitic polys of 800). Also, in cirrhosis w septic shock, mortality ⬆️ 10% for every hour’s delay in initiating antibiotics (PMID: 22753144)
Let’s summarize: pt was lined/tapped/orders for blood/ABx/steroids had been given and an incomplete prelim diagnosis had been made. But I had not done something crucial: GOC discussion w family. When I have no help from NP/PA, I try to stabilize the patient in the first 30-45 min
...before talking to families. If there is NP/PA to take care of the pt, I usually go to talk to families myself right away. In this case, I apologized for keeping them waiting and told them that there is a life-threatening bleeding but I don’t know the source. I told them that
we would try to decrease the rate of blood loss but that I doubted we could stop it completely without a surgical or IR intervention. I still had to talk to our IR and GenSurg to see if there is something to “offer” but if they could not help,
I would not recommend transfer to a tertiary care center; I thought the pt was too unstable to be moved. Family agreed with the plan.
IR thought pt was too sick and also felt that the bleeding was from the liver, probably from a previous paracentesis or fall. The surgeon was about to start another case (🤦♂️) and would not be available for the next 2-3 h (one of the problems when you work in a small hospital).
After the family meeting and the calls to IR/GenSurg, I returned to check on the patient. The RN asked me how much ascitic fluid to drain. What would you say?
To her surprise, I asked her to drain no fluid. I don’t know if this was the right move (especially since the pt had already abdominal discomfort and was in resp distress) but I thought - and hoped - that if the bleeding was venous (what else could it be?)
the raised intra-abdominal pressure from hemoperitoneum might be higher than the venous pressure (DBP of 30s-40s with IAP of 30s-40s seemed likely) and/or at least keep the bleeding site under some pressure and slow down the blood loss until the surgeon could take care of it
Luckily, pt responded to our interventions and even his mental status improved to the point that a few hours later he participated in discussions with the surgeon about the “next step”. He did consent to surgery and an exp-lap was performed
8 liters of hemorrhagic ascites and blood clots were evacuated. There was active bleeding from the inferior part of the R hepatic lobe, likely from a hepatic tear. Topical application of hemostatic agent controlled the bleeding.
Pt returned to the ICU “stable”; he was extubated in 2 days, pressors were dc/ed and surprisingly even renal function recovered without need for dialysis. Patient left the ICU a few days later
Take-home messages:
1. “Falls” are very frequent, especially in elderly pts (50% of those over 80 fall at least once a year) but they shoud not represent the end of the diagnostic approach. Many times they are due to a separate, underlying process (sepsis, bleeding etc) or
1. “Falls” are very frequent, especially in elderly pts (50% of those over 80 fall at least once a year) but they shoud not represent the end of the diagnostic approach. Many times they are due to a separate, underlying process (sepsis, bleeding etc) or
lead to another pathological entity (fracture, bleeding etc) as probably happened in this case
2. There is always a discussion in EM/CC audiences about the safety or utility of placing NGT in cirrhotics w possible esoph varices / upper GI bleeding. My response is that
2. There is always a discussion in EM/CC audiences about the safety or utility of placing NGT in cirrhotics w possible esoph varices / upper GI bleeding. My response is that
the benefit of knowing if the pt is bleeding and narrowing my diagnostic thoughts is much bigger than any theoretical concern of harm
Loading suggestions...