1/ A case: I was asked to assess a pt that just arrived with hypotension and HR in the 20s by my co-attending in the ED. ECG was with no P waves and RBBB w/ LAFB & severe bradycardia. POC K was ordered, and echo done as epinephrine gtt started at 5 mcg/min.
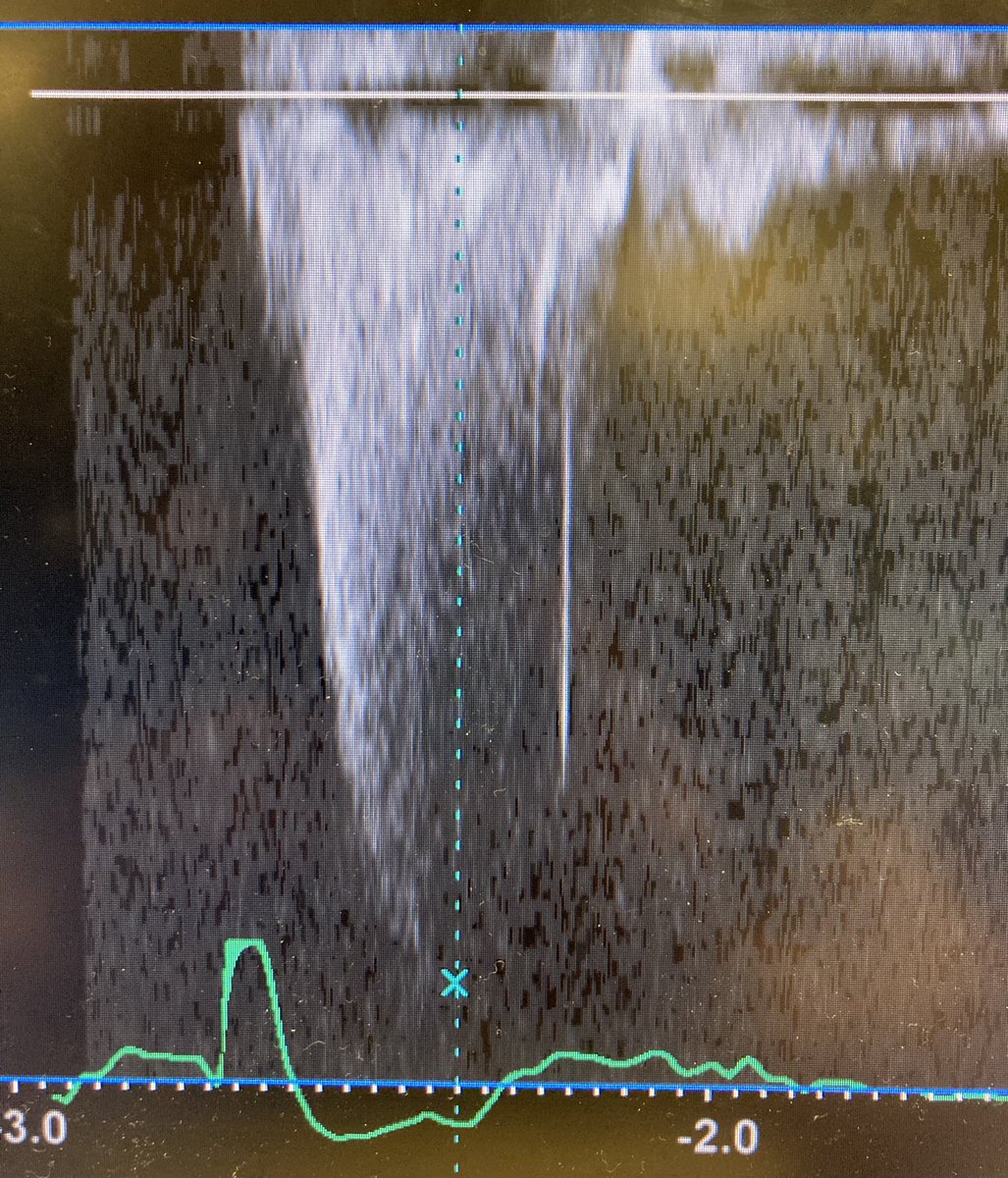
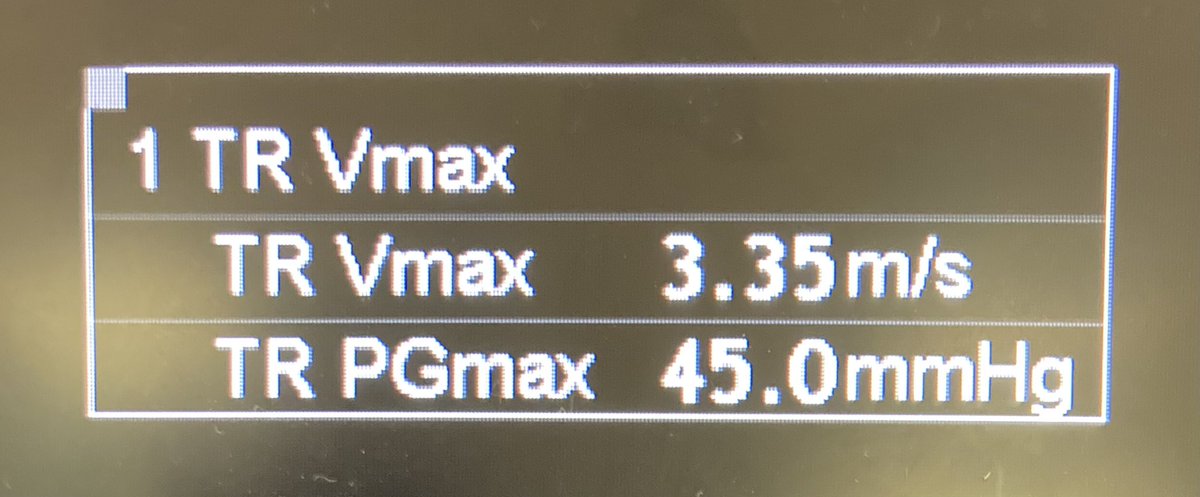
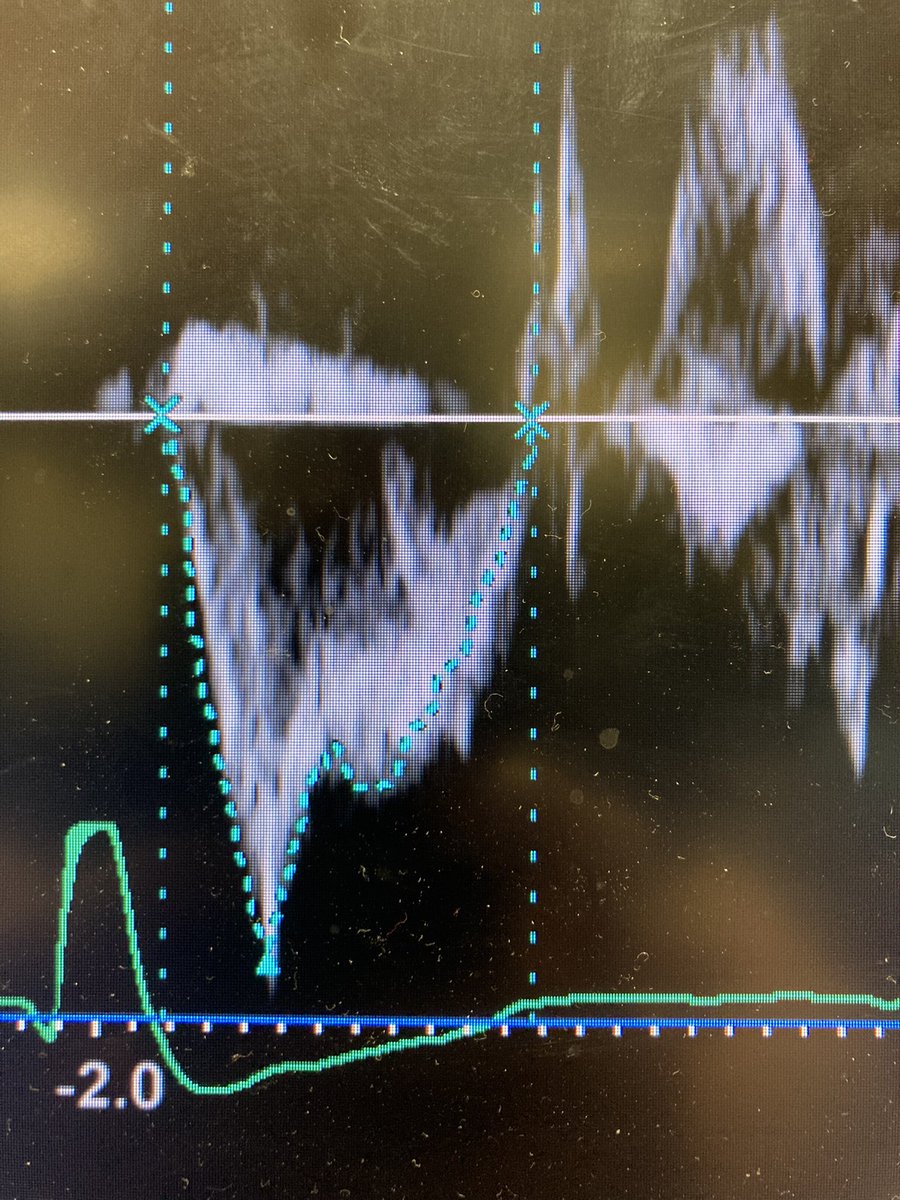
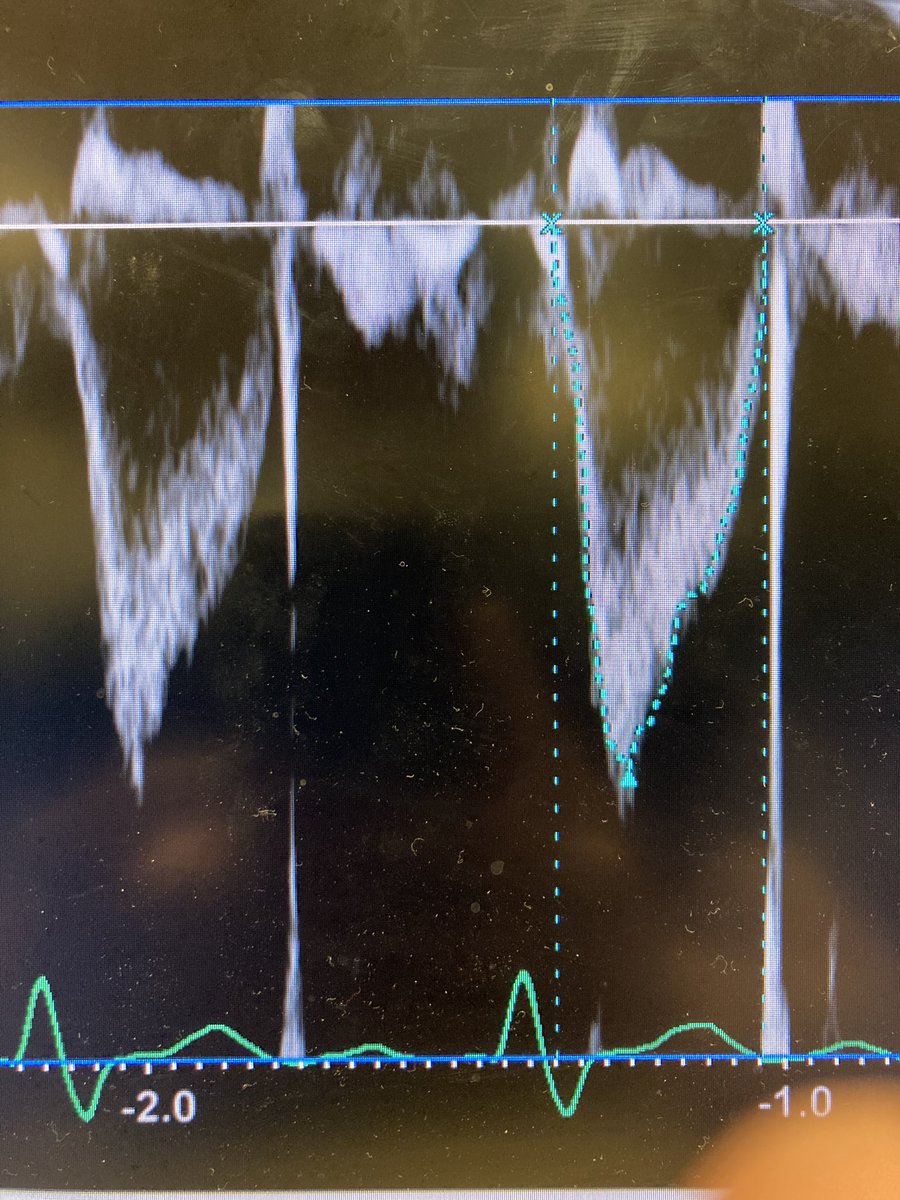
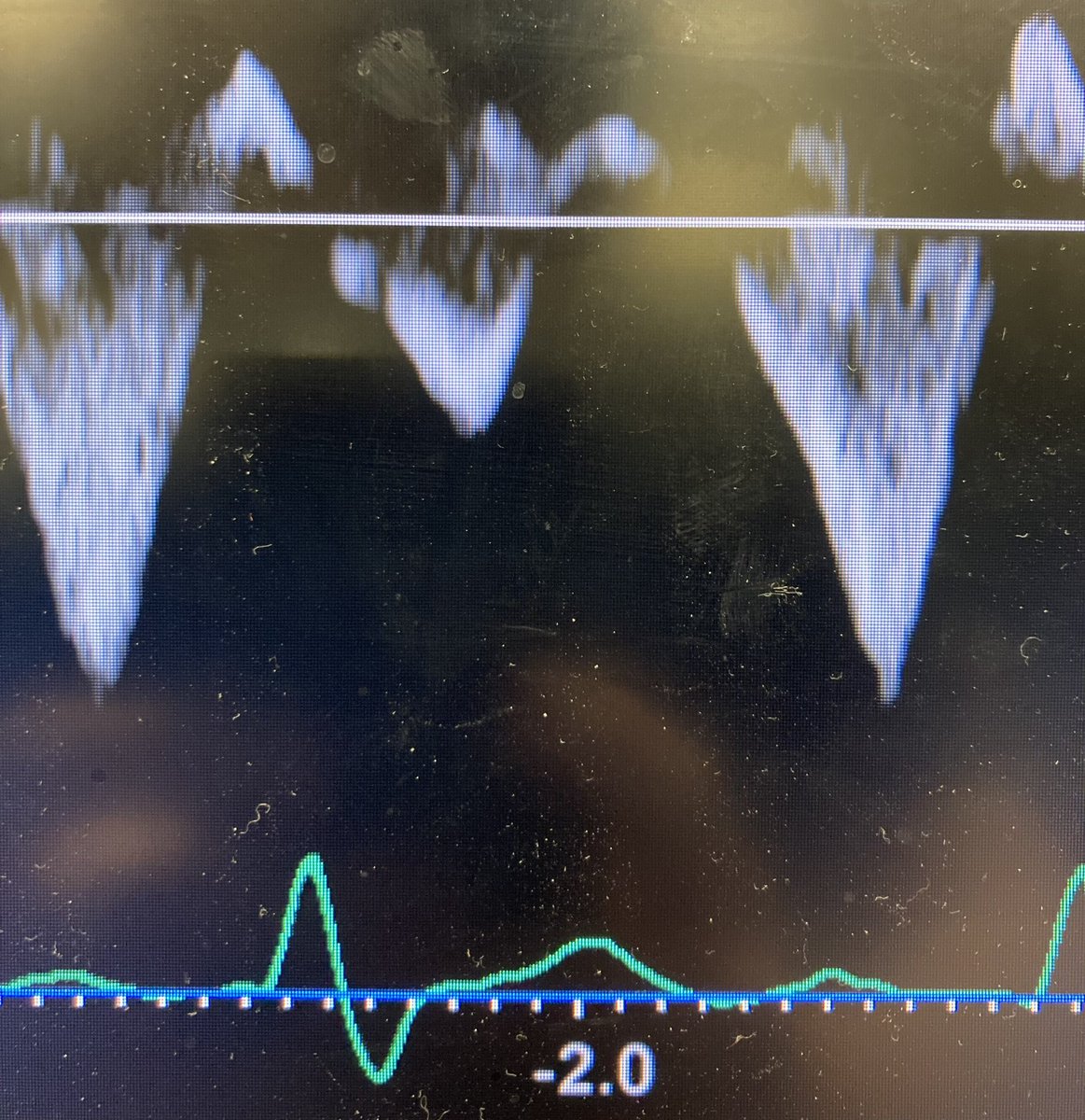
4/ In addition there was interventricular septal shift in systole and diastology: further evidence of increased PVR and RV pressures > LV pressures.
5/ POC K was 7.4 and so the patient was given CaCl2, NaHCO3, Insulin/D10, Albuterol, and furosemide. HR immediately increased to 70s, BP became slightly elevated, and the pt became alert. Skin from ashen to pink. Epinephrine gtt was able to be turned off.
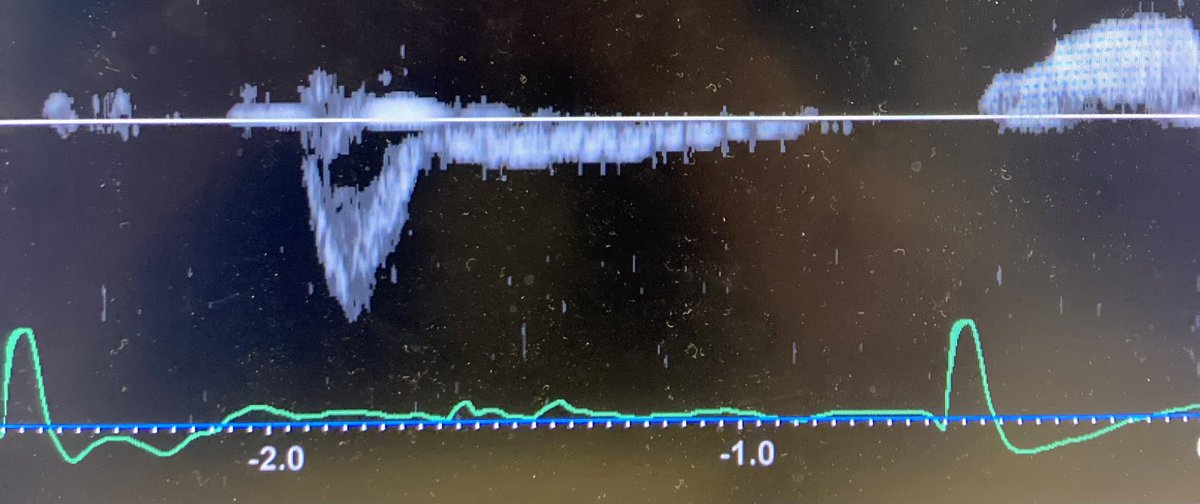
8/ ECG: NRS now with the same RBBB & LAFB.
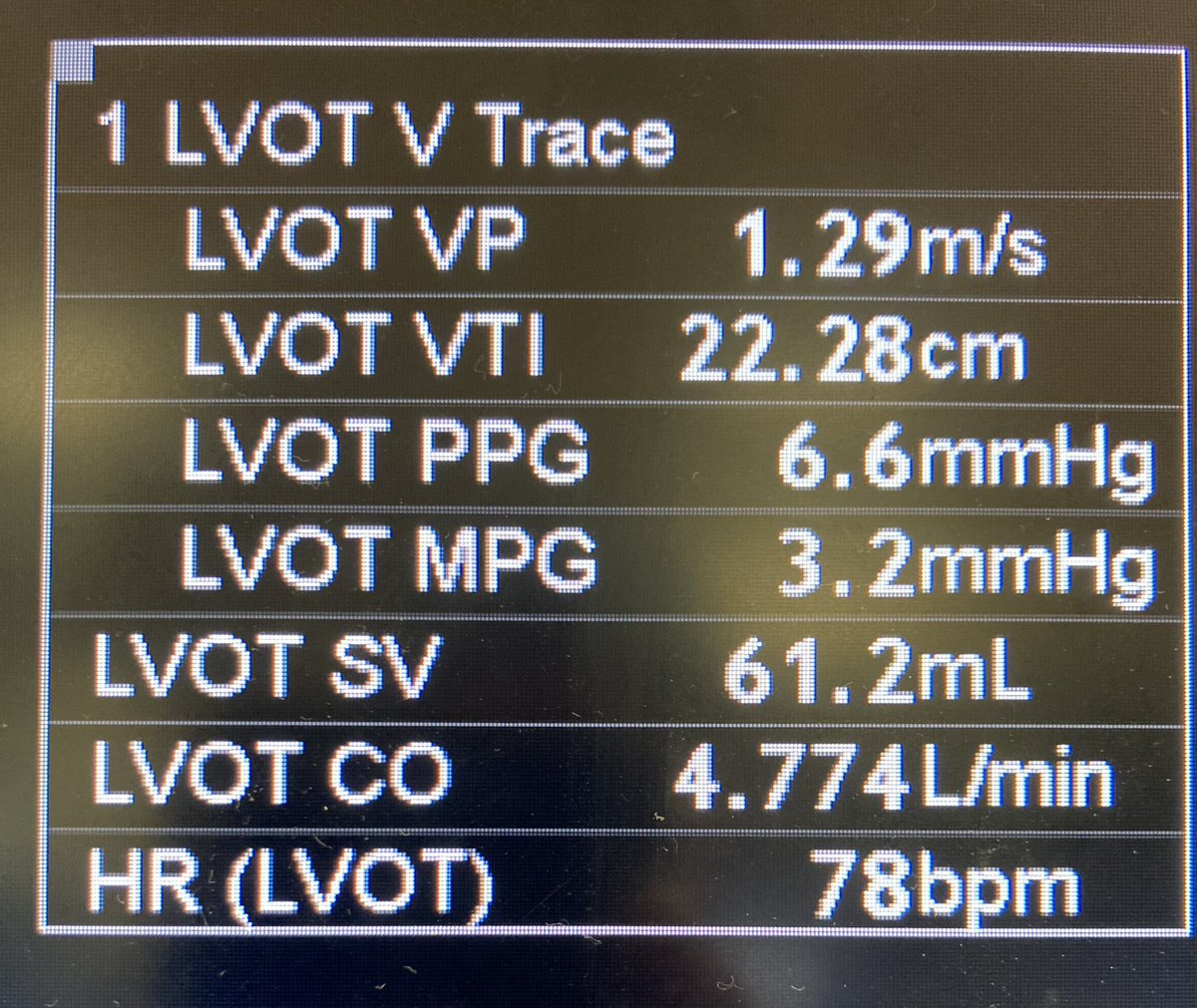
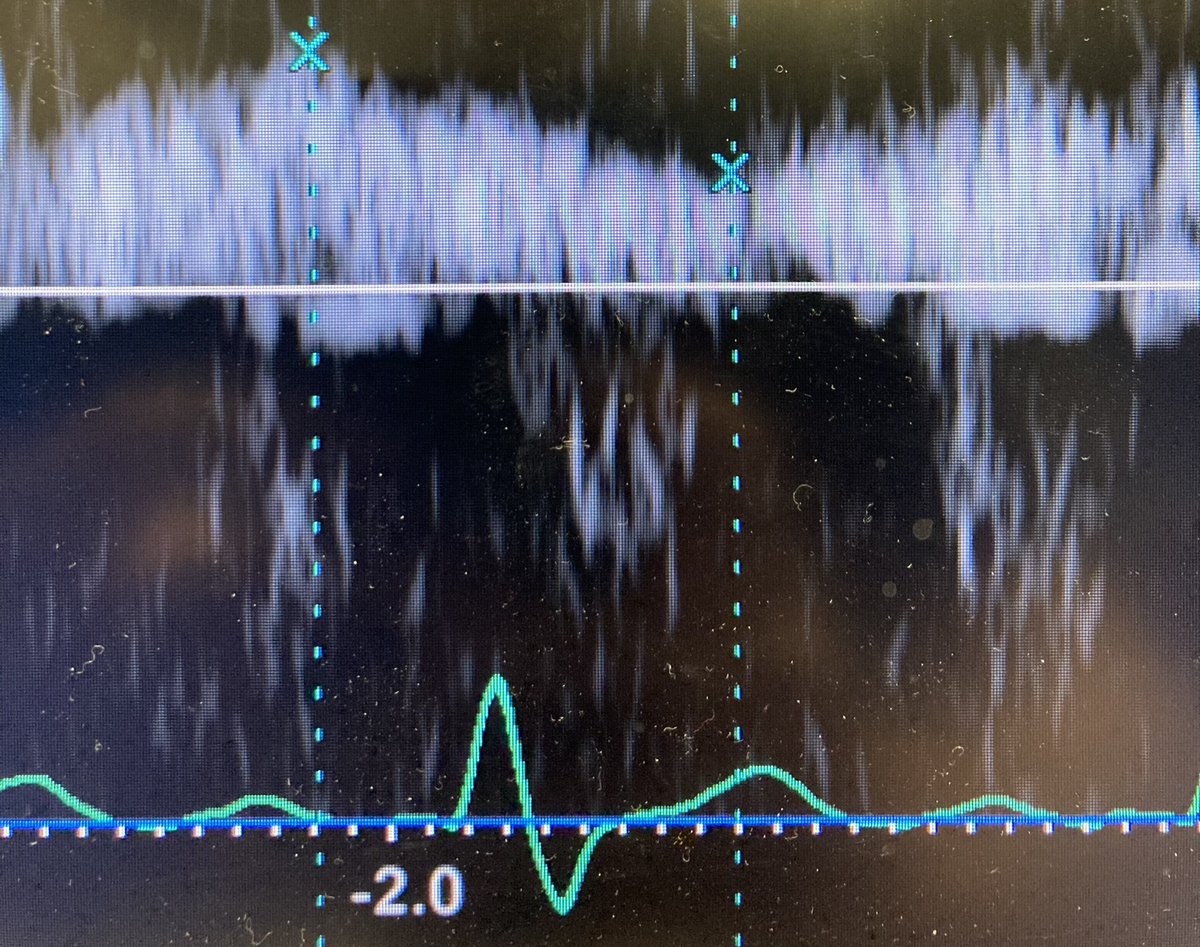
9/ So when the patient was shocked, there seemed to be a cardiogenic shock (due to ⬇️HR, SV preserved), and RV/PA uncoupling from elevated PVR. This seems to have completely resolved after potassium was corrected and HR/BP normalized.
10/ So a couple points: 1) hemodynamics are often a moving target and it is important to take a second look when things are done or things have changed. 2) In a sick patient, no inferences should be made about baseline cardiac function when not sick.
11/11 Finally, I’d be interested in comments on this patient’s changes in hemodynamic profile. I thought it was quite interesting for things to change so much with only potassium treatment.
Loading suggestions...