1/
I *LOVE* candy (srsly love.)
Recently, at the airport, I saw a bag of sour patch kids (fav!).
It was v overpriced.
I did not NEED it.
And it might take a while to get.
‼️Same with the hypercoag panel in acute stroke‼️
A #tweetorial @MedTweetorials #NeuroTwitter
I *LOVE* candy (srsly love.)
Recently, at the airport, I saw a bag of sour patch kids (fav!).
It was v overpriced.
I did not NEED it.
And it might take a while to get.
‼️Same with the hypercoag panel in acute stroke‼️
A #tweetorial @MedTweetorials #NeuroTwitter
2/
There is small fraction of patients for whom some of these tests make sense.
But, what I hope this thread will address is a reflexic rx to send a hypercoag panel in any “young” stroke pt.
Out of curiosity has *anyone* ever diagnosed legit inherited Protein C deficiency?
There is small fraction of patients for whom some of these tests make sense.
But, what I hope this thread will address is a reflexic rx to send a hypercoag panel in any “young” stroke pt.
Out of curiosity has *anyone* ever diagnosed legit inherited Protein C deficiency?
3/
Goals for the scroll:
1⃣The concept of stroke in the young
2⃣The yield for the hypercoag panel tests
3⃣When it might be reasonable to send these tests
Goals for the scroll:
1⃣The concept of stroke in the young
2⃣The yield for the hypercoag panel tests
3⃣When it might be reasonable to send these tests
4/
Stroke in the young is ⏫. 1990s: 10% of strokes occurred in adults <54. That number has nearly doubled! pubmed.ncbi.nlm.nih.gov
Young patients are traditionally enriched in nontraditional stroke mechanisms and thus require a thoughtful eval.
Stroke in the young is ⏫. 1990s: 10% of strokes occurred in adults <54. That number has nearly doubled! pubmed.ncbi.nlm.nih.gov
Young patients are traditionally enriched in nontraditional stroke mechanisms and thus require a thoughtful eval.
5/
However, the double is not driven by an uptick in CADASIL cases. It’s that stroke in the young is starting to look more like stroke in the old.
The prevalence of these RF for stroke likely reflects some #socialdeteriments of health. @GreenJournal open.spotify.com
However, the double is not driven by an uptick in CADASIL cases. It’s that stroke in the young is starting to look more like stroke in the old.
The prevalence of these RF for stroke likely reflects some #socialdeteriments of health. @GreenJournal open.spotify.com
6/
For example, the 44 yo patient with a HgbA1c of 9, smoking, an LDL of 158 and poorly controlled BP is biologically not 44 and likely does not require an extended workup to understand what’s going on.
Alternatively, a 62 yo marathoner w/ a pristine metabolic *might.*
For example, the 44 yo patient with a HgbA1c of 9, smoking, an LDL of 158 and poorly controlled BP is biologically not 44 and likely does not require an extended workup to understand what’s going on.
Alternatively, a 62 yo marathoner w/ a pristine metabolic *might.*
7/
But for a young pt w/ no traditional vascular risk factors is the “hypercoag panel” going to be helpful?
What *is* the “hypercoag panel” anyways!?
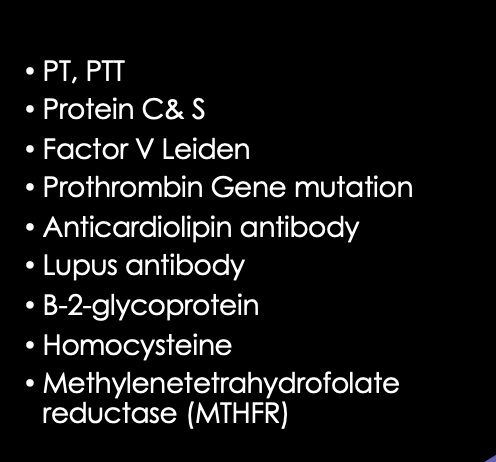
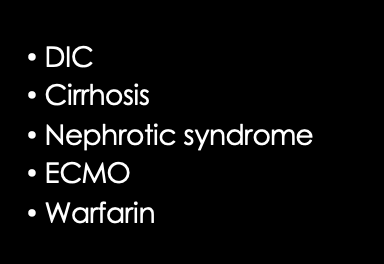
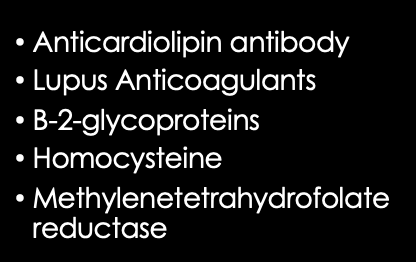
There is some hospital variability, but per the @StrokeAHA_ASA these are the tests that are part of the "hypercoag" w/u:
But for a young pt w/ no traditional vascular risk factors is the “hypercoag panel” going to be helpful?
What *is* the “hypercoag panel” anyways!?
There is some hospital variability, but per the @StrokeAHA_ASA these are the tests that are part of the "hypercoag" w/u:
9/
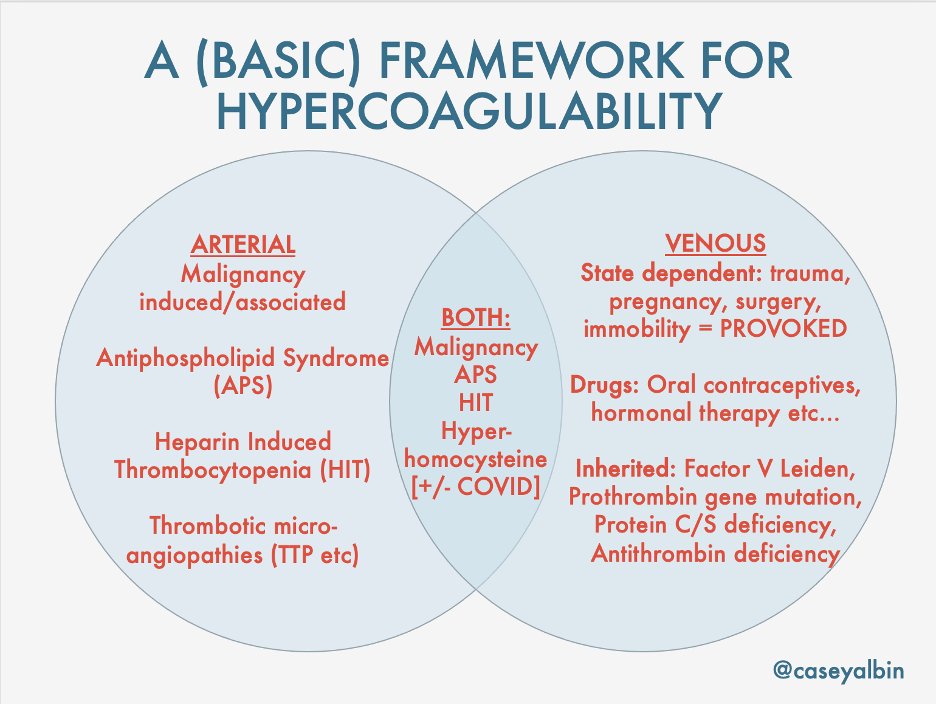
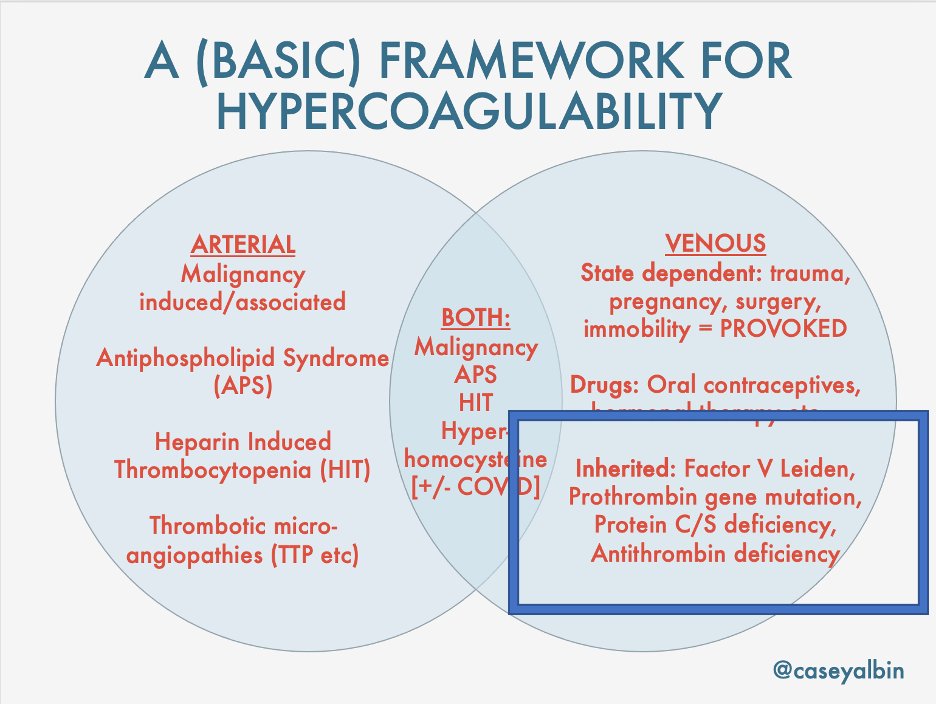
Could a risk factor for clots on the venous side lead to a cerebral artery clot?
Yes. *IF* there is a way that a clot bypassed the usual pulmonary filtration, ie there is R ➡️L shunt
The most common cause of R➡️ L shunting = patent foramen ovale (PFO). Others are ASDs & pAVM
Could a risk factor for clots on the venous side lead to a cerebral artery clot?
Yes. *IF* there is a way that a clot bypassed the usual pulmonary filtration, ie there is R ➡️L shunt
The most common cause of R➡️ L shunting = patent foramen ovale (PFO). Others are ASDs & pAVM
10/
The most sensitive way to find out if any shunt exists is TCD of the MCA during injection of agitated saline.
The TCDs unfortunately won’t tell you where the shunt is. Probability wise, tho, it’s likely a PFO, which can be confirmed with a TEE.
pubmed.ncbi.nlm.nih.gov
The most sensitive way to find out if any shunt exists is TCD of the MCA during injection of agitated saline.
The TCDs unfortunately won’t tell you where the shunt is. Probability wise, tho, it’s likely a PFO, which can be confirmed with a TEE.
pubmed.ncbi.nlm.nih.gov
12/
Being Heterozygous for Factor V Leiden mutation occurs in 3-6% percent of people of European descent. Very uncommon in stroke pts of African descent.
If testing starts w/ functional screen of activated protein C, know that Lupus a/c = false+, Tx w/ DT/Xa inhibitors = false-
Being Heterozygous for Factor V Leiden mutation occurs in 3-6% percent of people of European descent. Very uncommon in stroke pts of African descent.
If testing starts w/ functional screen of activated protein C, know that Lupus a/c = false+, Tx w/ DT/Xa inhibitors = false-
13/
What about prothrombin gene mutation? G20210A mutation can cause a 2-4 fold higher risk of venous thrombosis.
There was a significant association with stroke in pt <42 yo w/ Euorpean ancestry. The CI is very wide & this hasn’t yet been replicated.
pubmed.ncbi.nlm.nih.gov
What about prothrombin gene mutation? G20210A mutation can cause a 2-4 fold higher risk of venous thrombosis.
There was a significant association with stroke in pt <42 yo w/ Euorpean ancestry. The CI is very wide & this hasn’t yet been replicated.
pubmed.ncbi.nlm.nih.gov
13/
Let’s say you DO find FVL or PT gene mutation.
Will it change management?
The risk for thrombosis may be ~5x higher. But if this is the first hypercoag event, then the patient made several decades without a problem.
Do you commit this patient to lifelong anticoagulation?
Let’s say you DO find FVL or PT gene mutation.
Will it change management?
The risk for thrombosis may be ~5x higher. But if this is the first hypercoag event, then the patient made several decades without a problem.
Do you commit this patient to lifelong anticoagulation?
17/
Antithrombin – same thing. true inherited deficiencies are very rare, and this may also be depleted in the acute phase or from treatment w/ LWH and Heparin.
pubmed.ncbi.nlm.nih.gov
If these come back low, you’ll probably just shrug and say it’s not conclusive.
Antithrombin – same thing. true inherited deficiencies are very rare, and this may also be depleted in the acute phase or from treatment w/ LWH and Heparin.
pubmed.ncbi.nlm.nih.gov
If these come back low, you’ll probably just shrug and say it’s not conclusive.
18/
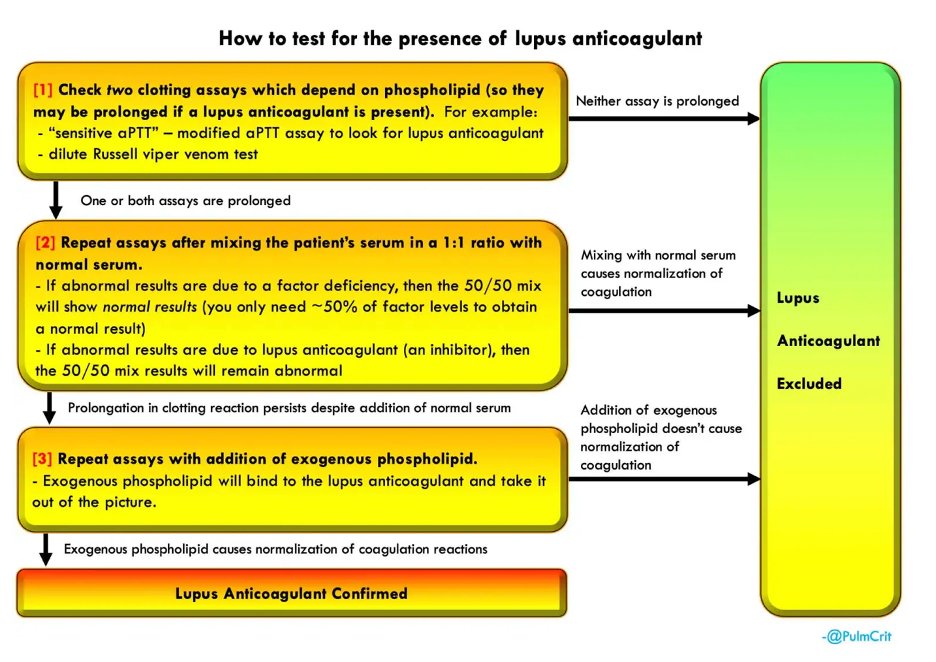
In the acute phase, the tests for LA and the aPTT can both be affected by acute thrombosis / inflammation, and give a false positive
For how acute inflammation interferes with testing, check out this awesome podcast/post from the @curiousclinicians.
curiousclinicians.com
In the acute phase, the tests for LA and the aPTT can both be affected by acute thrombosis / inflammation, and give a false positive
For how acute inflammation interferes with testing, check out this awesome podcast/post from the @curiousclinicians.
curiousclinicians.com
19/
Fortunately, the antibodies themselves (aCL and B-2-GP) can be tested with ELISA and thus not subject to the inflammatory state or anticoagulation, but they must be confirmed again on testing at least 12 weeks later.
The take away here?
Fortunately, the antibodies themselves (aCL and B-2-GP) can be tested with ELISA and thus not subject to the inflammatory state or anticoagulation, but they must be confirmed again on testing at least 12 weeks later.
The take away here?
20/
It’s reasonable to test women, those with autoimmunity (SLE)… or maybe even recent COVID and now stroke?… (emcrit.org)
A positive finding of aCL and B-2-GP is valid, but whether its causative or persistent won’t be known in the acute phase.
It’s reasonable to test women, those with autoimmunity (SLE)… or maybe even recent COVID and now stroke?… (emcrit.org)
A positive finding of aCL and B-2-GP is valid, but whether its causative or persistent won’t be known in the acute phase.
21/
You'll have to make management decisions about a/c before a definitive diagnosis is made!
The presence other clots (and certainly if it looks ike catastrophic APS) is helpful in making a temporary management call.
These tend to be highly personalized tx decisions.
You'll have to make management decisions about a/c before a definitive diagnosis is made!
The presence other clots (and certainly if it looks ike catastrophic APS) is helpful in making a temporary management call.
These tend to be highly personalized tx decisions.
22/
Final take aways? Stroke in the young is starting to look like stroke in the old. ✅ trad. stuff first! Proceed w/ caution for advanced w/u.
✨PTG & FLV testing only if euro-ancestry+ ⬆️RoPE score+PFO
✨Lupus A/c is affected by acute inflammation& +aCL/B2-GP require confirm
Final take aways? Stroke in the young is starting to look like stroke in the old. ✅ trad. stuff first! Proceed w/ caution for advanced w/u.
✨PTG & FLV testing only if euro-ancestry+ ⬆️RoPE score+PFO
✨Lupus A/c is affected by acute inflammation& +aCL/B2-GP require confirm
24/
Out of space for homocysteine, so stay tuned but in the meantime, love anyone else thoughts/ opinions on this murky topic! @namorrismd @nsanar @a_charidimou @MicieliA_MD @feras_akbik @AvrahamCooperMD @dr_jmartindale @drdangayach @aartisarwal @AANMember @LyellJ @EricLawson90
Out of space for homocysteine, so stay tuned but in the meantime, love anyone else thoughts/ opinions on this murky topic! @namorrismd @nsanar @a_charidimou @MicieliA_MD @feras_akbik @AvrahamCooperMD @dr_jmartindale @drdangayach @aartisarwal @AANMember @LyellJ @EricLawson90
Loading suggestions...