shape.
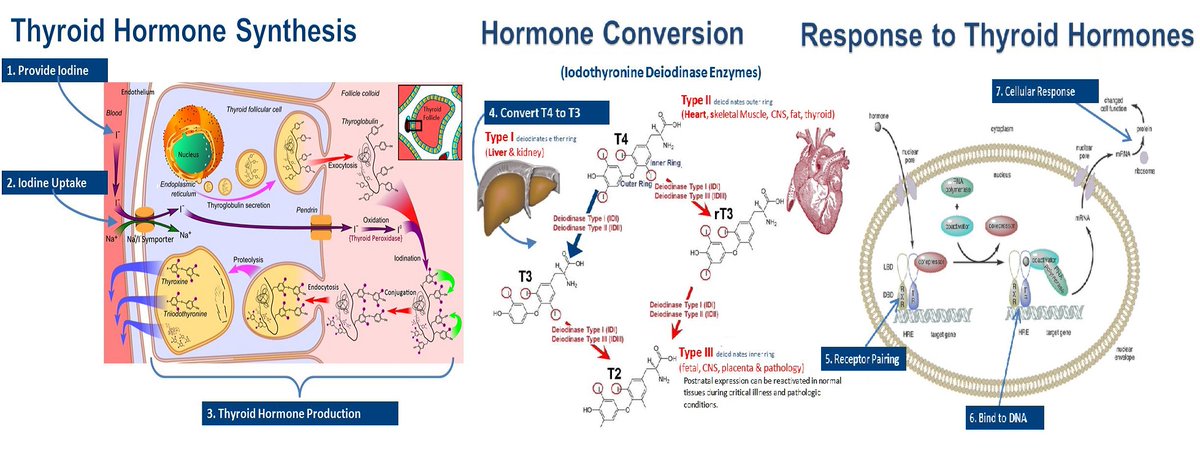
The thyroid is one of the glands that make up the endocrine system.
The glands of the endocrine system produce and store hormones and release them into the bloodstream.
The hormones then travel through the body and direct the activity of the body’s cells.
The thyroid is one of the glands that make up the endocrine system.
The glands of the endocrine system produce and store hormones and release them into the bloodstream.
The hormones then travel through the body and direct the activity of the body’s cells.
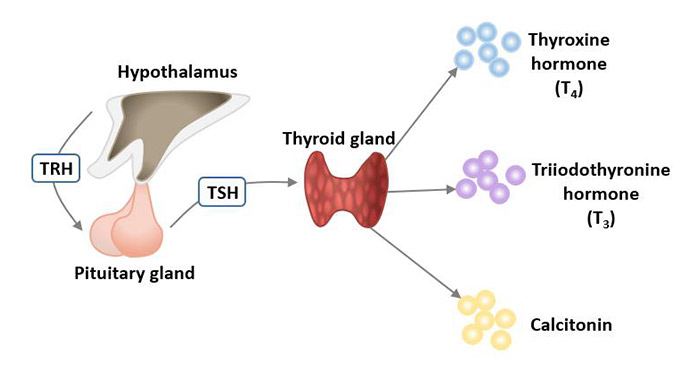
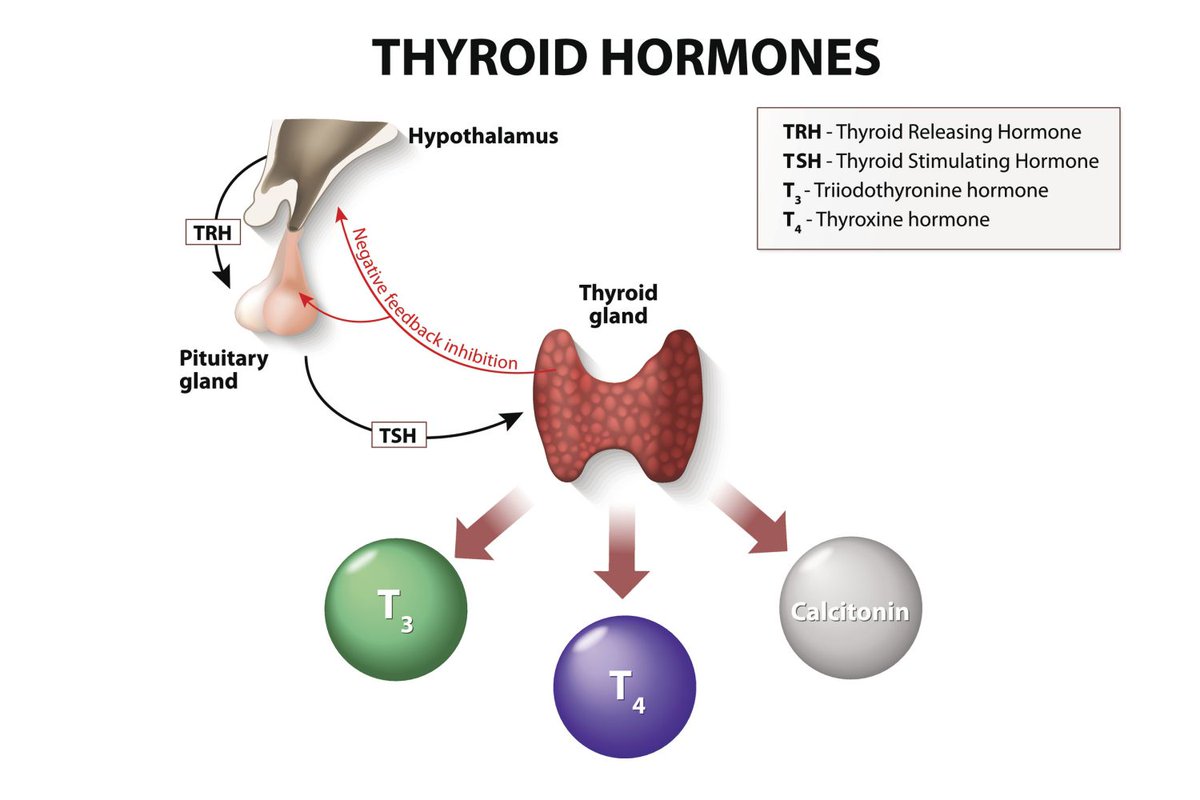
T3 is made from T4 and is the more active hormone, directly affecting the tissues.
When (inactive) T4 is released into the bloodstream, it goes to the liver and other organs to be converted into (active) T3.
This conversion is known as deiodination of T4 and is a process which
When (inactive) T4 is released into the bloodstream, it goes to the liver and other organs to be converted into (active) T3.
This conversion is known as deiodination of T4 and is a process which
When thyroid hormone levels are high, the pituitary responds by dropping TSH production.
Hypothyroidism is a disorder that occurs when the thyroid gland does not make enough thyroid hormone to meet the body’s needs.
Hypothyroidism is a disorder that occurs when the thyroid gland does not make enough thyroid hormone to meet the body’s needs.
There are 11 typical signs of suboptimal thyroid function and hence suboptimal metabolic function.
These are:
#1: Chronic fatigue
#2: Not being hungry in the morning
#3: Low body temperature and slowed heart rate
#4: Thinning hair (which is very different than
These are:
#1: Chronic fatigue
#2: Not being hungry in the morning
#3: Low body temperature and slowed heart rate
#4: Thinning hair (which is very different than
hair loss)
#5: Dry skin
#6: High LDL
#7: Insomnia
#8: Low libido
#9: Inability to put on muscle mass
#10: High prolactin
#11: Hearing problems
Now a typical thyroid panel test includes:
1)TSH (1.0 – 2.5 μIU/mL)
2)Total T4 ( 6.0 – 11.9 mcg/dL)
3)Total T3 (100 – 168 ng/dL)
#5: Dry skin
#6: High LDL
#7: Insomnia
#8: Low libido
#9: Inability to put on muscle mass
#10: High prolactin
#11: Hearing problems
Now a typical thyroid panel test includes:
1)TSH (1.0 – 2.5 μIU/mL)
2)Total T4 ( 6.0 – 11.9 mcg/dL)
3)Total T3 (100 – 168 ng/dL)
4)Reverse T3 (14.9 – 24.1 ng/dL)
5)Free T4 (1.0 – 1.5 ng/dL)
6)Free T3 (3.0 – 4.0 pg/mL)
7)Thyroid antibodies (0 – 15 IU/mL)
Now in most cases hypothyroidism can be completely controlled with the right lifestyle changes and perhaps liothyronine (cytomel and triostat).
5)Free T4 (1.0 – 1.5 ng/dL)
6)Free T3 (3.0 – 4.0 pg/mL)
7)Thyroid antibodies (0 – 15 IU/mL)
Now in most cases hypothyroidism can be completely controlled with the right lifestyle changes and perhaps liothyronine (cytomel and triostat).
So, the conversion problem is what needs to be addressed in order to help thyroid performance in a lot of people.
Which are the most common things that cause conversion problems and how can we address them?
First, not enough thyroid supportive nutrients in the diet.
Which are the most common things that cause conversion problems and how can we address them?
First, not enough thyroid supportive nutrients in the diet.
These are:
0)Sunlight.
Without daily sunlight, you can forget about having a healthy thyroid.
1)Copper which is required for the synthesis of thyroid hormones.
2)Selenium which is also required for the synthesis of thyroid hormones and a selenium deficiency usually leads to
0)Sunlight.
Without daily sunlight, you can forget about having a healthy thyroid.
1)Copper which is required for the synthesis of thyroid hormones.
2)Selenium which is also required for the synthesis of thyroid hormones and a selenium deficiency usually leads to
autoimmune thyroiditis.
Important note: some people don’t pay attention to vitamin C when it comes to thyroid but vitamin C affects the entire endocrine system and also a deficiency affects selenium metabolism which will directly affect thyroid.
Important note: some people don’t pay attention to vitamin C when it comes to thyroid but vitamin C affects the entire endocrine system and also a deficiency affects selenium metabolism which will directly affect thyroid.
3)Zinc which is required for the synthesis of thyroid hormones but also the function of T3 receptors.
Zinc is one of the primary facilitators of proper thyroid function because zinc it a) is responsible for vitamin A activity b)the synthesis of thyroid hormone and
Zinc is one of the primary facilitators of proper thyroid function because zinc it a) is responsible for vitamin A activity b)the synthesis of thyroid hormone and
c) it is involved in the pathways responsible for the recycling of vitamin C.
Which brings us to 4) Vitamin C.
Vitamin C is the first defender when it comes to the protection of many vital organs (especially the heart) including the thyroid.
Which brings us to 4) Vitamin C.
Vitamin C is the first defender when it comes to the protection of many vital organs (especially the heart) including the thyroid.
5)Vitamin A + B12 which are required both for the proper utilization of thyroid hormones.
Vitamin A regulates thyroid hormone metabolism and inhibits thyroid-stimulating hormone (TSH).
6)Iodine which is required for the synthesis of thyroid hormones.
Vitamin A regulates thyroid hormone metabolism and inhibits thyroid-stimulating hormone (TSH).
6)Iodine which is required for the synthesis of thyroid hormones.
The thyroid hormone itself is an iodine containing protein.
We recycle a lot of iodine every day and you should NOT supplement iodine.
The best sources for iodine are some seaweed every once in a while, cod and shrimp.
We recycle a lot of iodine every day and you should NOT supplement iodine.
The best sources for iodine are some seaweed every once in a while, cod and shrimp.
7)Beta carotene
Without pro-vitamin A, aka carotene the body cannot make or use thyroid hormone.
8)Calcium
In order to perform some vital daily functions, the body works to keep a steady amount of calcium in the blood and tissues.
Without pro-vitamin A, aka carotene the body cannot make or use thyroid hormone.
8)Calcium
In order to perform some vital daily functions, the body works to keep a steady amount of calcium in the blood and tissues.
If calcium levels drop too low in the blood, parathyroid hormone (PTH) will signal the bones to release calcium into the bloodstream.
At the same time, PTH signals the kidneys to release less calcium in the urine.
At the same time, PTH signals the kidneys to release less calcium in the urine.
10) Carbohydrates
Carbohydrates are the most efficient source of energy we humans have access to and some cells in the body can only run on carbohydrates.
The liver can function optimally only when there are sufficient energy stores of glycogen.
Carbohydrates are the most efficient source of energy we humans have access to and some cells in the body can only run on carbohydrates.
The liver can function optimally only when there are sufficient energy stores of glycogen.
If you go low carb for years, your thyroid will get destroyed since your liver won’t have enough glucose to convert T4 into T3 and since 70% of this conversion happens only in the liver you will experience hypothyroidism and suboptimal metabolic health.
Then we have: Gut issues
Part of deiodination happens in the small intestines, so an unhealthy gut will directly affect our thyroid.
This happens because thyroid hormone in a healthy gut reacts with acetic acid which activates it and transforms T4 into T3.
Part of deiodination happens in the small intestines, so an unhealthy gut will directly affect our thyroid.
This happens because thyroid hormone in a healthy gut reacts with acetic acid which activates it and transforms T4 into T3.
If the gut is in a state of dysbiosis and producing very little acetic acid, T3 fails to activate and thus results in functional hypothyroidism (conversion problems).
Here's a full guide on gut healing that you can check.
heliosmovement.substack.com
Here's a full guide on gut healing that you can check.
heliosmovement.substack.com
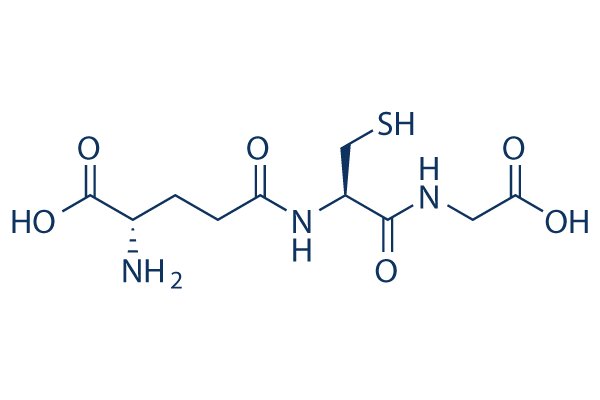
It is produced by the liver and is responsible for detoxification and thyroid hormone conversion.
Glutathione plays a role in many chemical reactions in our body, helps detoxify chemicals and protects our mitochondria against oxidative stress.
Glutathione plays a role in many chemical reactions in our body, helps detoxify chemicals and protects our mitochondria against oxidative stress.
Lower glutathione levels appear to go hand-in-hand with poor thyroid function since glutathione pathways help the conversion of T4 to T3.
Glutathione is an antioxidant dependent on selenium and produced in the cytosol of the cell.
Glutathione is an antioxidant dependent on selenium and produced in the cytosol of the cell.
How to boost glutathione production 101
1)Consume sulfur rich foods such as fish, beef, onions, garlic, shallots and broccoli once in a while after you’ve healed your gut.
2)Consume vitamin C and E rich foods.
Vitamin C maintains the body’s supply of antioxidants, including
1)Consume sulfur rich foods such as fish, beef, onions, garlic, shallots and broccoli once in a while after you’ve healed your gut.
2)Consume vitamin C and E rich foods.
Vitamin C maintains the body’s supply of antioxidants, including
glutathione and helps reprocess glutathione by converting oxidized glutathione back to its active form.
3)Consume selenium rich foods.
Selenium is a glutathione cofactor, meaning it’s a substance needed for glutathione activity and will lead to increased glutathione peroxidase
3)Consume selenium rich foods.
Selenium is a glutathione cofactor, meaning it’s a substance needed for glutathione activity and will lead to increased glutathione peroxidase
levels.
4)Start adding turmeric in your meals once in a while (not too often). Numerous animal and test-tube studies have shown that turmeric and curcumin extract have the ability to increase glutathione levels.
4)Start adding turmeric in your meals once in a while (not too often). Numerous animal and test-tube studies have shown that turmeric and curcumin extract have the ability to increase glutathione levels.
5)Other important nutrients that our body needs to make and recycle glutathione are: magnesium, zinc, B vitamins, glycine and glutamine which can all be found in animal products such as organs, oysters, free range eggs and bone marrow, brewer’s yeast and some sprouted white rice
cooked in bone broth.
If you choose to supplement NAC in order to boost glutathione just know that it will deplete copper levels and should be avoided long term.
Another thing that greatly affects our thyroid is heavy metal toxicity, here's a full thread on this
If you choose to supplement NAC in order to boost glutathione just know that it will deplete copper levels and should be avoided long term.
Another thing that greatly affects our thyroid is heavy metal toxicity, here's a full thread on this
Last but not least, ditching sodium fluoride and sort term boron supplementation might be crucial and necessary for some people.
That's it for now.
If you liked this please like or RT the first tweet.
That's it for now.
If you liked this please like or RT the first tweet.
And you know where to find more.
fitandball.gumroad.com
fitandball.gumroad.com
Loading suggestions...