ICU stories: Diabetic ketoacidosis (DKA) is another "bread-and-butter" ICU case. The typical scenario is one of a patient who presents to the ED w nausea/vomiting/weakness, receives a few liters of iv fluids & insulin drip overnight (according to a protocol), & the next day he is
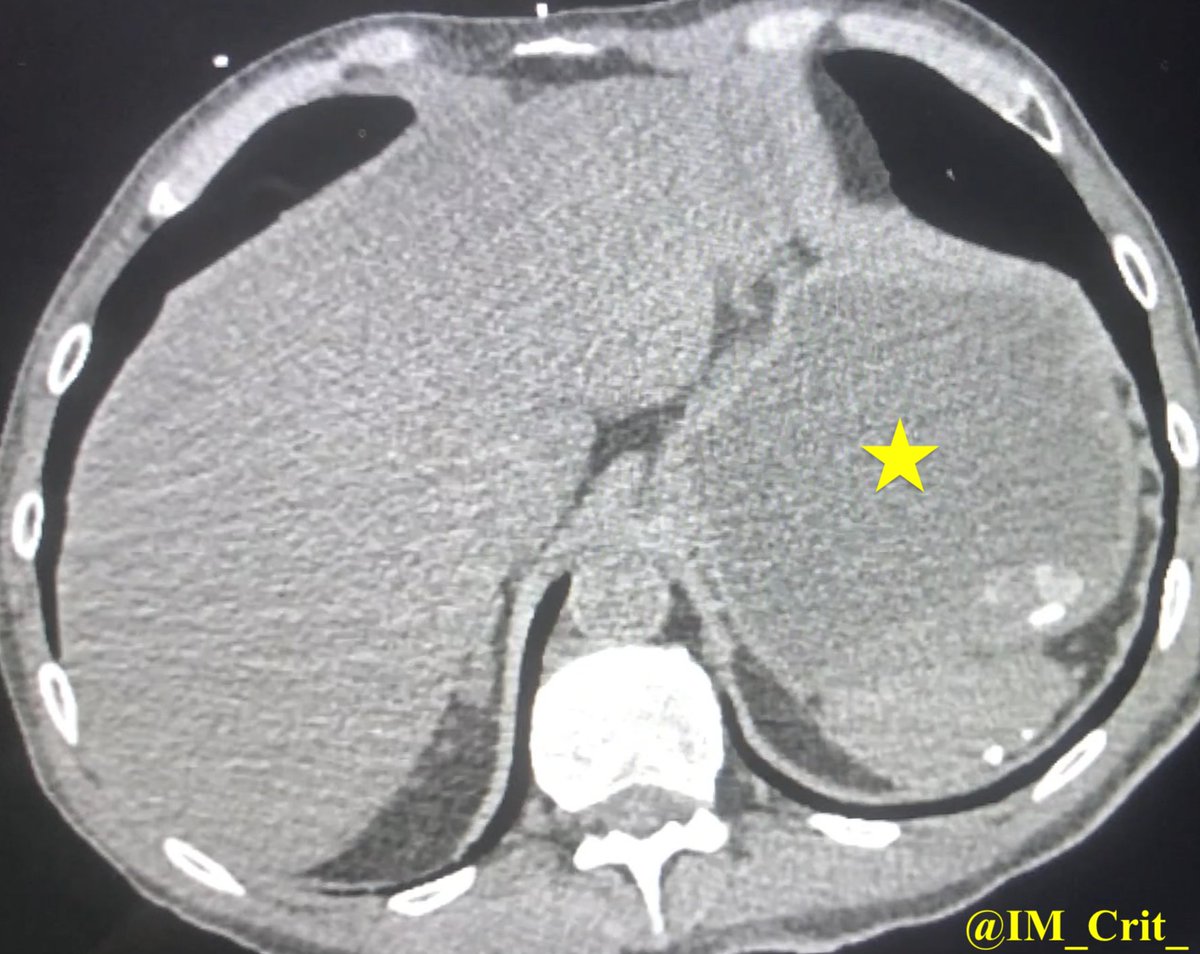
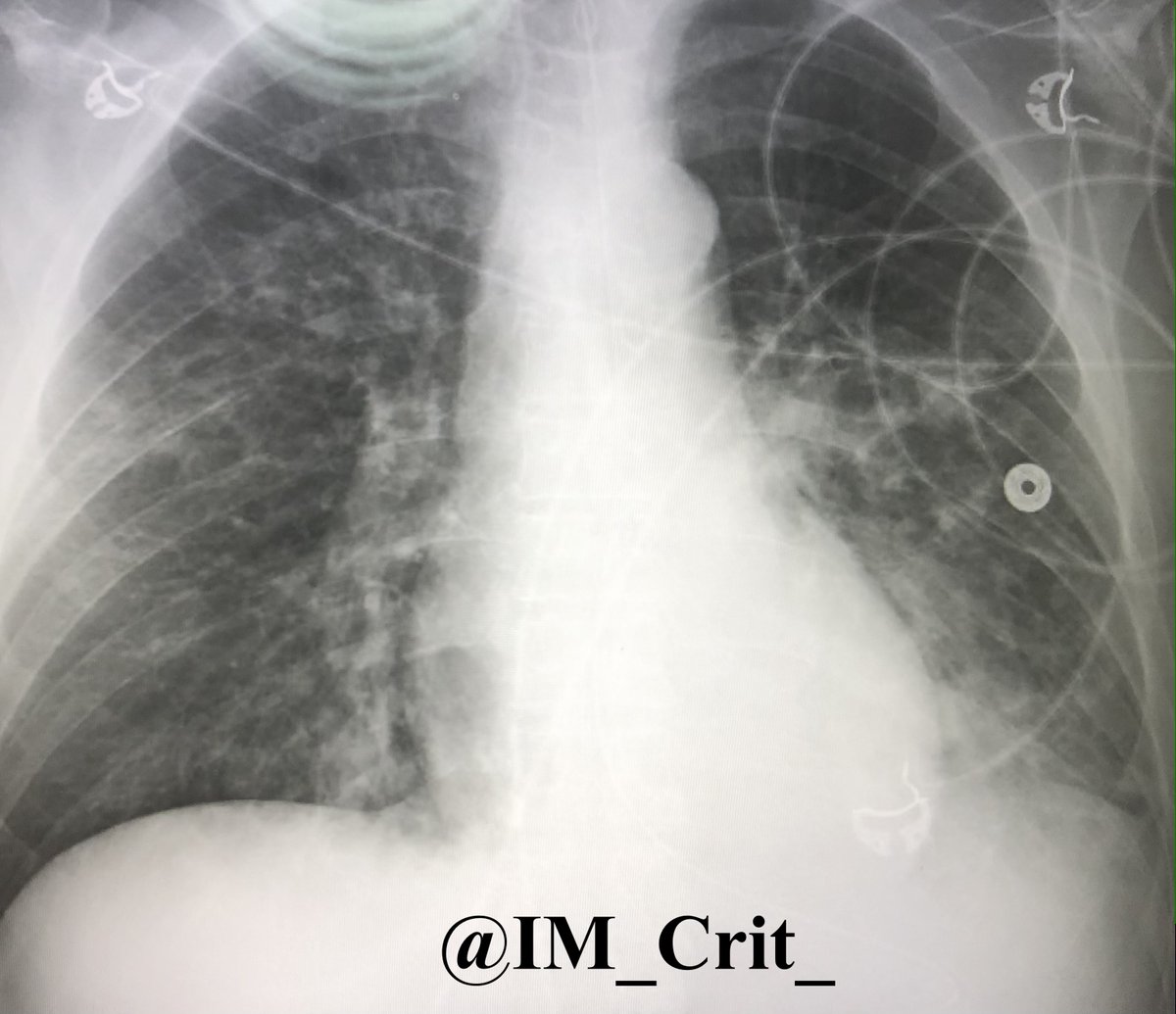
"mural thickening of multiple small & large bowel loops (nonspecific, but may be secondary to an infectious/inflammatory enterocolitis) & hepatic steatosis". Before/during the planned transfer, what would you be more concerned about?
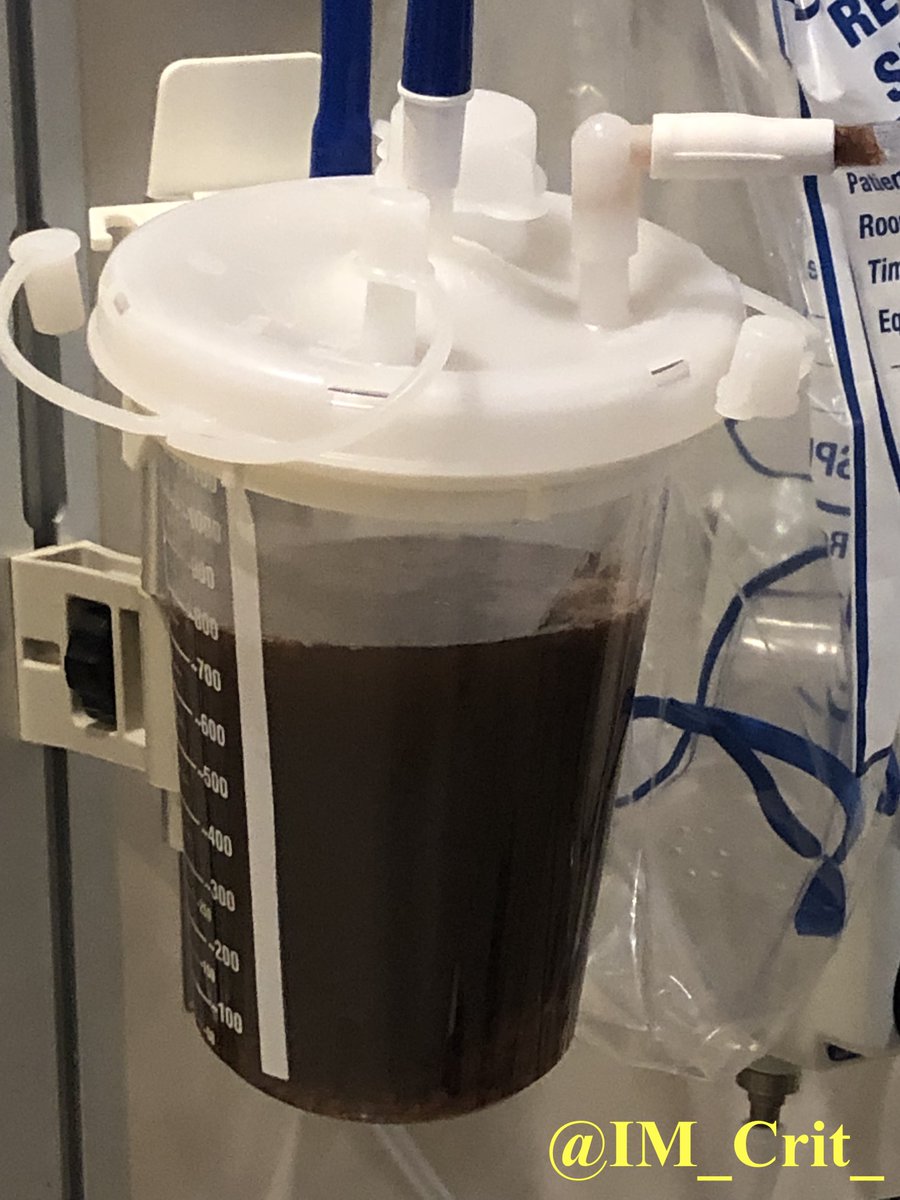
fluid-filled... I know, you are thinking: who cares about fluid in the stomach, right? I asked for NG tube placement before transfer. This was never placed. Pt was transferred by helicopter. During the 20 min flight, respiratory status deteriorated & pt was placed on NIV...
& got worse w additional aspiration. Pt stayed on the vent for 5 ds. Also developed vasodilatory shock requiring norepi/vasopressin drips for 3 ds (I am skipping POCUS findings, sorry!) as well as AKI requiring CRRT. Eventually, he improved & was extubated. RUE weakness resolved.
Renal function normalized. A few months later he was re-admitted. He had developed R vocal cord paresis likely due to intubation-related trauma. Direct microlaryngoscopy was performed w injection into the paraglottic space & medialization of the R vocal cord
Take-home messages:
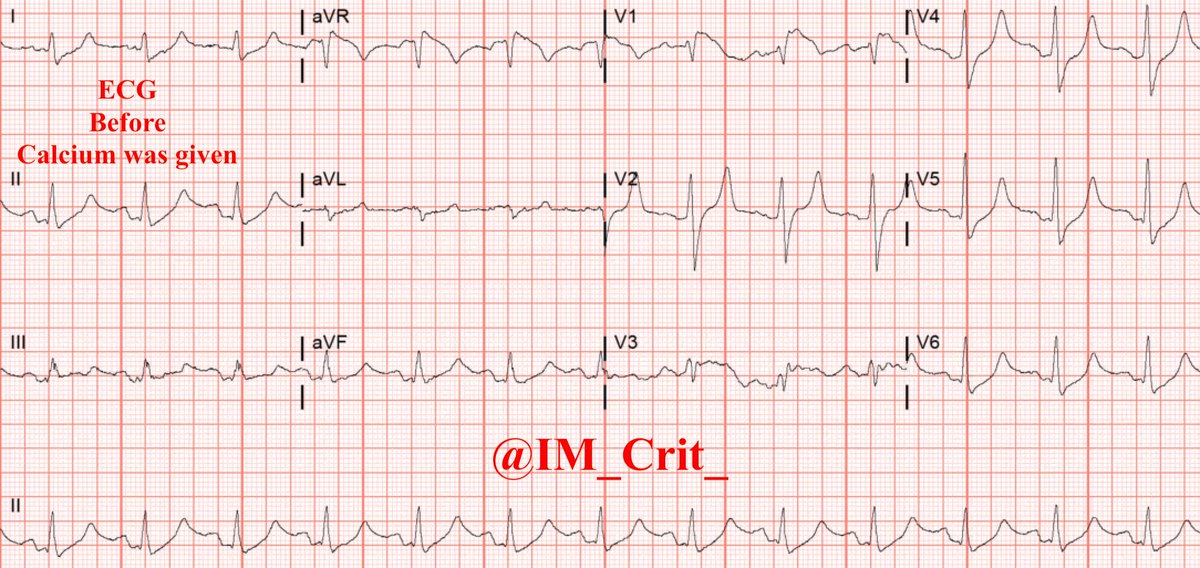
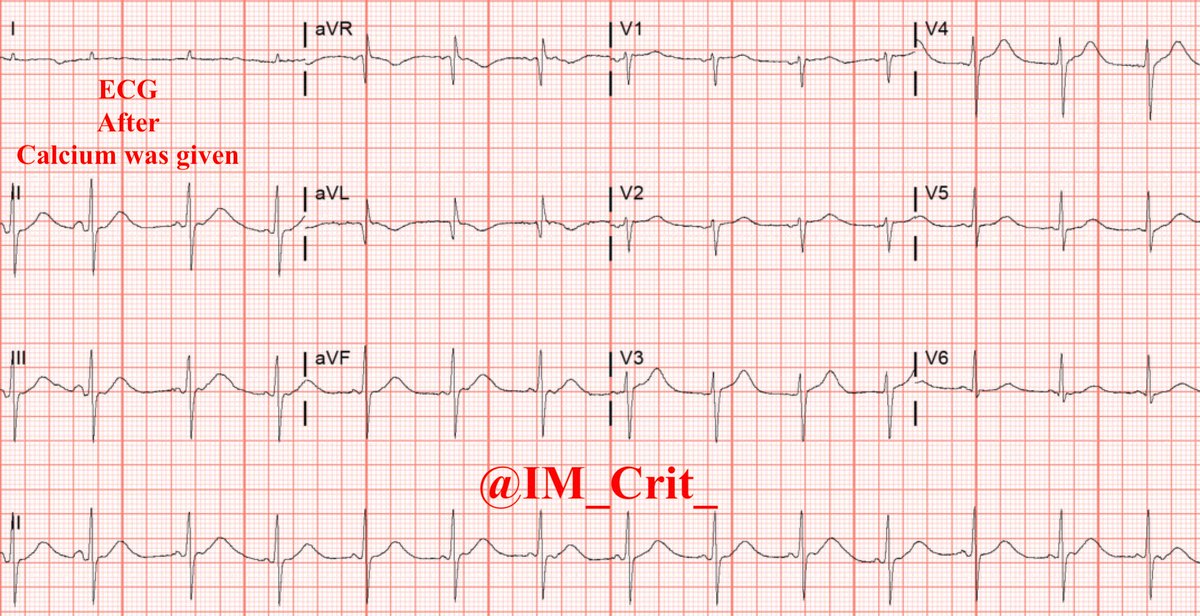
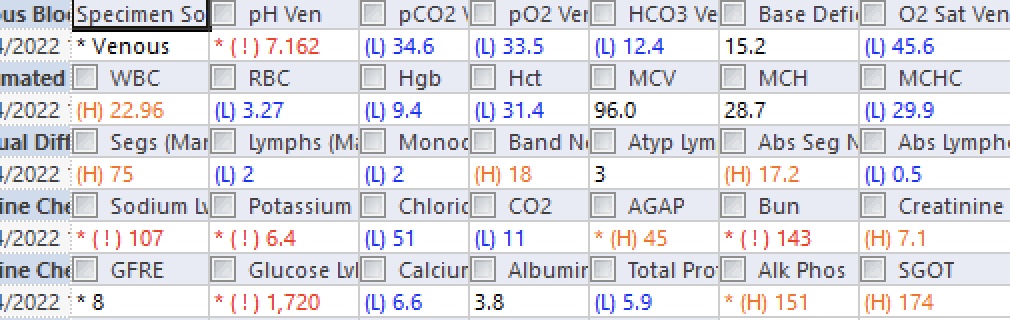
1. Not all DKAs are created equal & patients do not read books (usually...). There is still a belief that DKA has to present w Glu levels in the hundreds but it is not uncommon to find euglycemic DKA or DKA w Glu > 1000. It is also not uncommon to manage pts
1. Not all DKAs are created equal & patients do not read books (usually...). There is still a belief that DKA has to present w Glu levels in the hundreds but it is not uncommon to find euglycemic DKA or DKA w Glu > 1000. It is also not uncommon to manage pts
w hyperglycemic hyperosmolar state & high anion gap metabolic acidosis due to concomitant ketoacidosis and/or to increase in lactate levels
2. The more severe a DKA case is, the more we have to think about underlying causes. WBC>20-25,000 and/or bands>10% should be a red flag
2. The more severe a DKA case is, the more we have to think about underlying causes. WBC>20-25,000 and/or bands>10% should be a red flag
3. Hyperglycemia can present (as in this case) w stroke-like symptoms. This is why we don’t jump right away on thrombolyzing before checking glucose. Having said that, previous versions of the American Heart Association guidelines for acute stroke treatment listed Glu <50 mg/dL
& >400 mg/dL as contraindications for thrombolysis, but the most recent 2019 updated edition only kept hypoglycemia as an exclusion. On the other hand, the FDA package insert for tPA recommends “special diligence” in making the diagnosis of stroke when Glu is <50 or >400 mg/dL
4. Even though it is not emphasized in the literature, pts w severe DKA are at significant risk of aspiration. This is due to depressed mental status & worsening of diabetic gastroparesis (acute on chronic!). In these patients, the use of NIV can become problematic...
I have low-threshold of placing a NGT in a patient w severe DKA or at least doing POCUS to make sure that the stomach is not full of content waiting to relocate in the lungs…
Thanks for reading! Obviously there are other ways to approach similar cases and I am always happy to be corrected!
#FOAMed #FOAMcc #MedTwitter #MedEd #EMBound @RJonesSonoEM @TaotePOCUS @cjosephy #MedStudentTwitter
#FOAMed #FOAMcc #MedTwitter #MedEd #EMBound @RJonesSonoEM @TaotePOCUS @cjosephy #MedStudentTwitter
Loading suggestions...