1/9
Hb vs. Hct - PART 2
I recently asked a series of questions about Hb vs Hct. I addressed some earlier and now turn to the remaining ones.
QUESTION: If Hb and Hct are not interchangeable (as we saw), then what different information are you imparting by reporting both?
Hb vs. Hct - PART 2
I recently asked a series of questions about Hb vs Hct. I addressed some earlier and now turn to the remaining ones.
QUESTION: If Hb and Hct are not interchangeable (as we saw), then what different information are you imparting by reporting both?
2/9
ANSWER: Reporting both Hb and Hct provides a SINGLE piece of information that Hb or Hct alone does not, namely the MCHC (MCHC = Hb/Hct).
But who needs to calculate the MCHC when it is provided as part of the CBC?
How about a medical student you wish to put on the spot 😀?
ANSWER: Reporting both Hb and Hct provides a SINGLE piece of information that Hb or Hct alone does not, namely the MCHC (MCHC = Hb/Hct).
But who needs to calculate the MCHC when it is provided as part of the CBC?
How about a medical student you wish to put on the spot 😀?
4/9
But in day-to-day practice, where the MCHC is almost always normal, the Hb and Hct are virtually interchangeable, and the two parameters are redundant.
I suggest it is intellectually lazy to report both.
Why not choose the one that makes most sense pathophysiologically?
But in day-to-day practice, where the MCHC is almost always normal, the Hb and Hct are virtually interchangeable, and the two parameters are redundant.
I suggest it is intellectually lazy to report both.
Why not choose the one that makes most sense pathophysiologically?
6/9
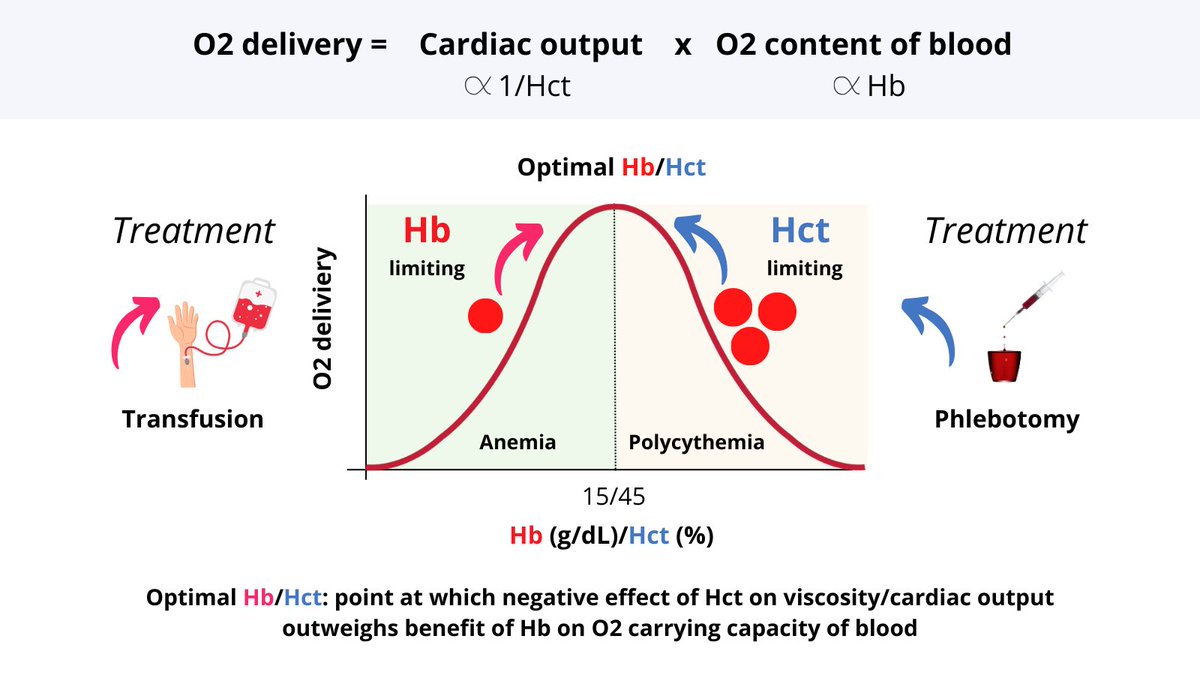
This point is called the optimal Hb/Hct and is highly conserved across mammalian species.
In patients who are anemic, the Hb (and oxygen carrying capacity) is limiting for oxygen delivery. The goal is to push them up the hill, e.g., with RBC transfusion or iron therapy.
This point is called the optimal Hb/Hct and is highly conserved across mammalian species.
In patients who are anemic, the Hb (and oxygen carrying capacity) is limiting for oxygen delivery. The goal is to push them up the hill, e.g., with RBC transfusion or iron therapy.
7/9
So it makes sense to speak of the Hb in patients with anemia.
In contrast, for those rare patients with polycythemia, the Hct is limiting, and the goal of therapy is to reduce the Hct, e.g. with phlebotomy or cytoreductive therapy. We should refer to the Hct in these folks.
So it makes sense to speak of the Hb in patients with anemia.
In contrast, for those rare patients with polycythemia, the Hct is limiting, and the goal of therapy is to reduce the Hct, e.g. with phlebotomy or cytoreductive therapy. We should refer to the Hct in these folks.
8/9
It is no accident that clinical practice guidelines use Hb thresholds for RBC transfusion and Hct thresholds for phlebotomizing patients with polycythemia!
It is no accident that clinical practice guidelines use Hb thresholds for RBC transfusion and Hct thresholds for phlebotomizing patients with polycythemia!
9/9
As for the majority of individuals who sit at the summit (those of us with a normal Hb/Hct), it's dealer's choice as to whether to refer to Hb or Hct. But I prefer Hb because I am "positive" thinker 😉.
As for the majority of individuals who sit at the summit (those of us with a normal Hb/Hct), it's dealer's choice as to whether to refer to Hb or Hct. But I prefer Hb because I am "positive" thinker 😉.
Loading suggestions...