3/8
Kudos to @Abhainngarbh for considering both possibilities and to @EDWINANAND3 for suggesting antibiotic-mediated AIHA 👏👏
This was in fact a case of delayed transfusion reaction.
Kudos to @Abhainngarbh for considering both possibilities and to @EDWINANAND3 for suggesting antibiotic-mediated AIHA 👏👏
This was in fact a case of delayed transfusion reaction.
4/8
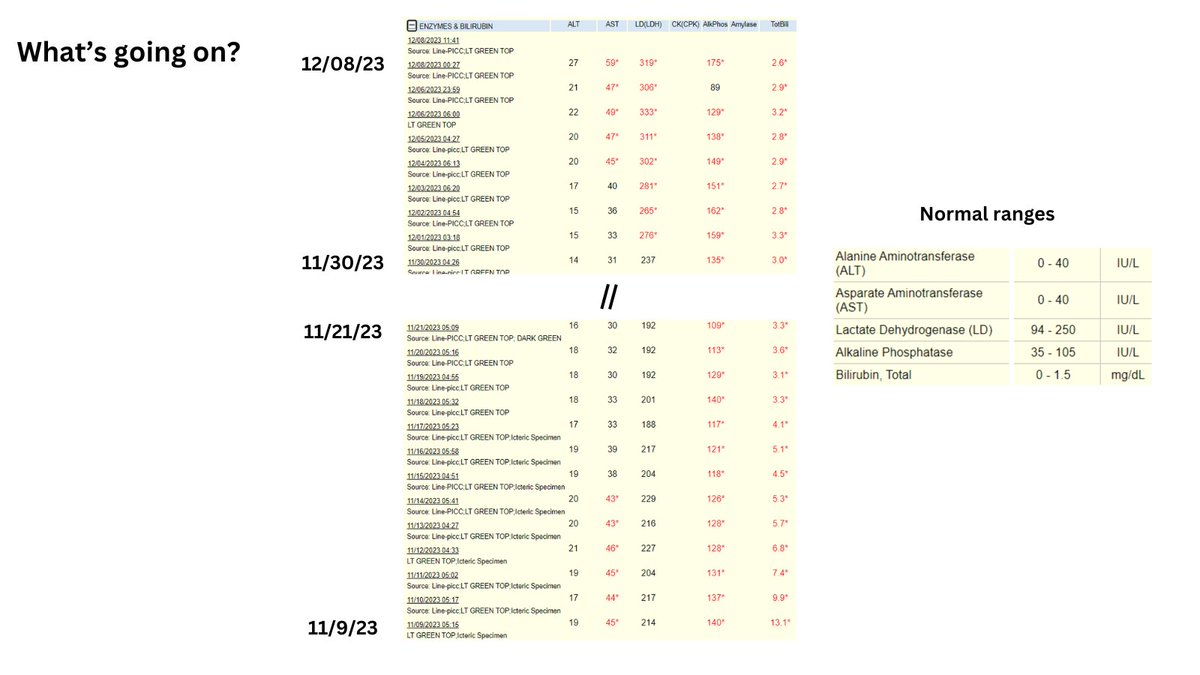
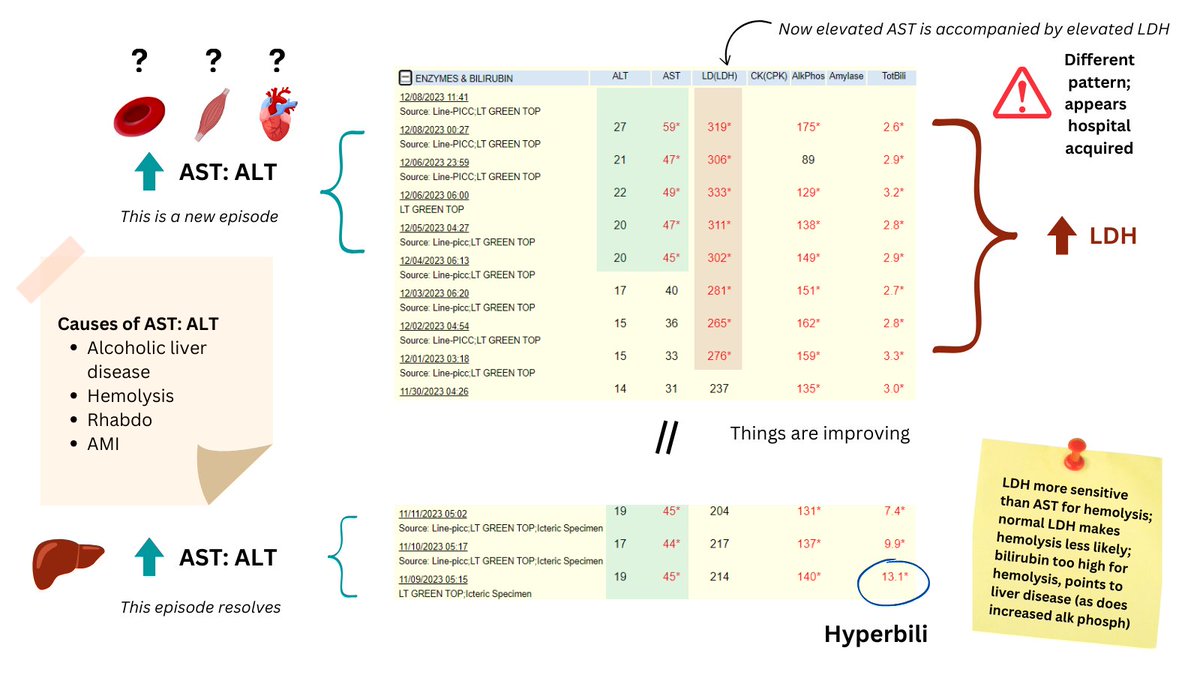
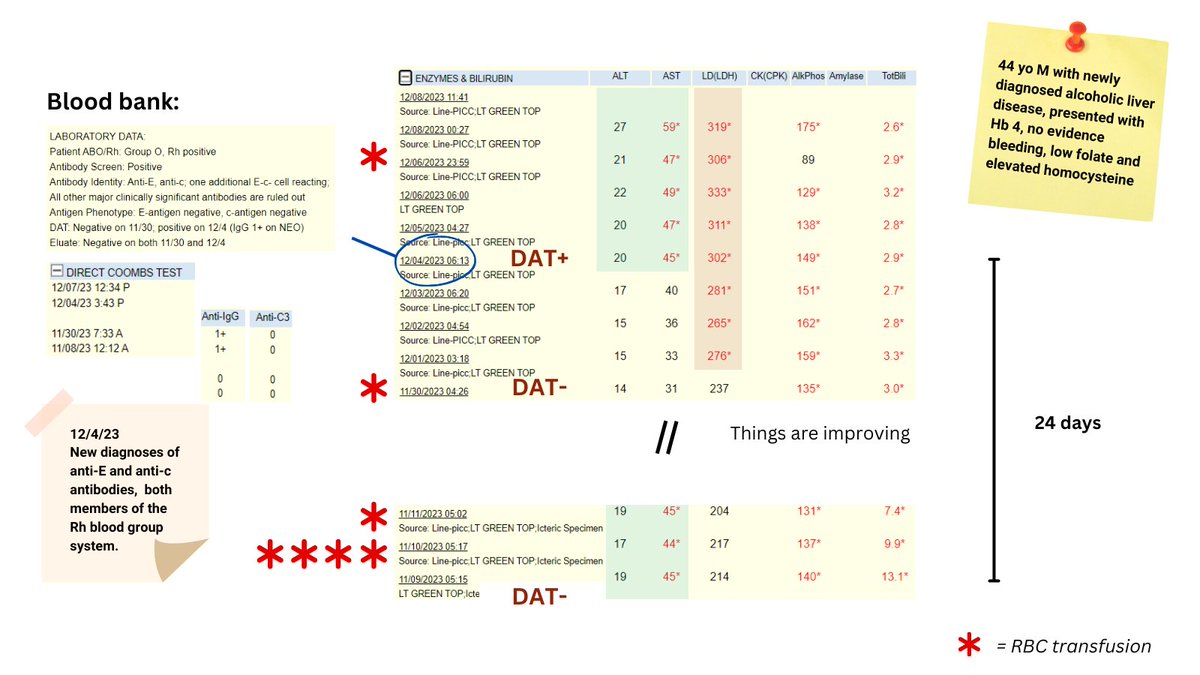
The patient was admitted with findings of alcoholic hepatitis, and was found to have Hb 4 g/dL. Work up for bleeding was negative. His folate was low, and MCV/homocysteine high. He had no hypersegmented PMNs. Initial WBC count high, PLT count normal (then fell).
The patient was admitted with findings of alcoholic hepatitis, and was found to have Hb 4 g/dL. Work up for bleeding was negative. His folate was low, and MCV/homocysteine high. He had no hypersegmented PMNs. Initial WBC count high, PLT count normal (then fell).
5/8
Treated with folate and received several units of pRBCs (see graphic).
When AST/LDH began to rise, DAT turned positive and he was found to have new anti-E and anti-c antibodies, all c/w delayed transfusion reaction (he had a past history of 7 pRBC transfusions).
Treated with folate and received several units of pRBCs (see graphic).
When AST/LDH began to rise, DAT turned positive and he was found to have new anti-E and anti-c antibodies, all c/w delayed transfusion reaction (he had a past history of 7 pRBC transfusions).
6/8
About delayed transfusion reactions (DTR):
DEFN: Positive DAT for antibodies developed between 24 h and 28 days after end of transfusion and:
1. New identification of RBC alloantibodies
2. One or more of the following:
2a. Insufficient increase in post-transfusion Hb
About delayed transfusion reactions (DTR):
DEFN: Positive DAT for antibodies developed between 24 h and 28 days after end of transfusion and:
1. New identification of RBC alloantibodies
2. One or more of the following:
2a. Insufficient increase in post-transfusion Hb
7/8
2b. Rapid decline in Hb back to pretransfusion levels
2c. Otherwise unexplained appearance of spherocytes in peripheral blood smear
EPI: DTR reported to account for 4.3% of all transfusion reactions.
2b. Rapid decline in Hb back to pretransfusion levels
2c. Otherwise unexplained appearance of spherocytes in peripheral blood smear
EPI: DTR reported to account for 4.3% of all transfusion reactions.
8/8
ETIOLOGY: Anamnestic immune response to antigens on donor in recipients who were previously alloimmunized (transfusion or pregnancy).
TIMING: Typically occurs 3-10 days after initial transfusion.
PRESENTATION: Hemolysis +/- anemia +/- fever.
TREATMENT: Supportive
ETIOLOGY: Anamnestic immune response to antigens on donor in recipients who were previously alloimmunized (transfusion or pregnancy).
TIMING: Typically occurs 3-10 days after initial transfusion.
PRESENTATION: Hemolysis +/- anemia +/- fever.
TREATMENT: Supportive
Loading suggestions...