1/ Hi 👋 #neurotwitter #medtwitter #neurocritcare, today we will be breaking down the following paper from @neurocritcareJ: x.com
Follow along to gleam over the most exciting and cool parts, including something you may have not heard of before!
Follow along to gleam over the most exciting and cool parts, including something you may have not heard of before!
@NeurocritCareJ 2/ ⬆ #ICP in #meningitis is something that is commonly seen and certainly a topic that I have covered multiple other times. For some examples, see below:
x.com
x.com
x.com
x.com
x.com
x.com
@NeurocritCareJ 3/ ⬆ICP in meningitis is very common & caused by:
✅ edema
✅ loss of autoregulation
✅ venous congestion
✅ hydrocephalus
✅ edema
✅ loss of autoregulation
✅ venous congestion
✅ hydrocephalus
@NeurocritCareJ 4/ Despite how common it is, why do we not place #ICPmonitors more frequently in this pt population? (Pro tip: don’t forget to read the accompanying editorial written by @provenciojavier! x.com)
@NeurocritCareJ @ProvencioJavier 5/ @ESCMID recommends 🐈scan and more research on when to use ICP monitors and the Swedish ID society recommends ICP monitoring in deteriorating or comatose patients but how often are we doing it now? That was what this paper was trying to answer!
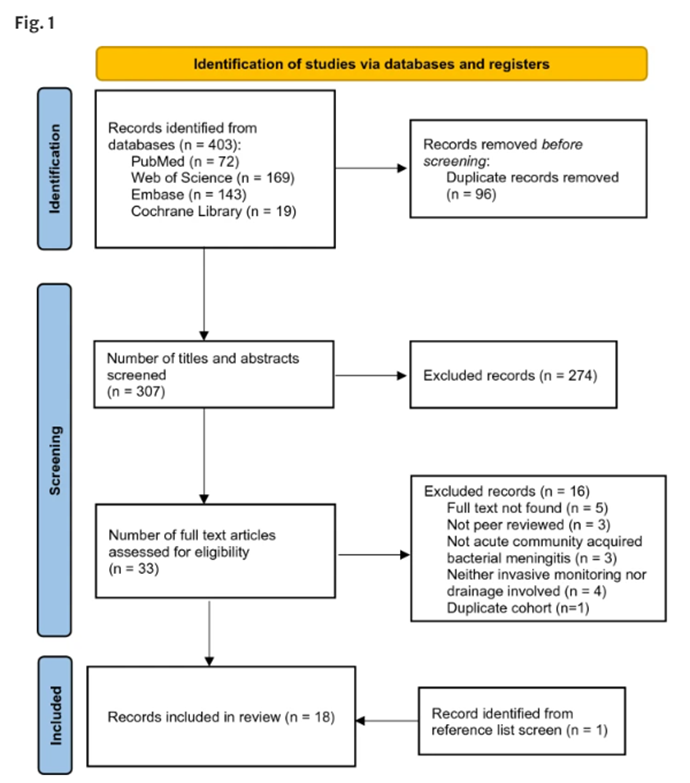
@NeurocritCareJ @ProvencioJavier @ESCMID 6/ In this meta-analysis, authors looked for papers talking about ICP monitoring and meningitis and they came up with 33 papers, of which 17 + 1 from reference list, were included:
@NeurocritCareJ @ProvencioJavier @ESCMID 7/ In summary:
🔢 Sample size: variable
🏛 Study type: mostly retrospective
🌍 Origin of study: Euro>US>India
📏 ICP measured via: EVD> Intraparenchymal monitor
✅ Main indication: deteriorating neuro status
🔢 Sample size: variable
🏛 Study type: mostly retrospective
🌍 Origin of study: Euro>US>India
📏 ICP measured via: EVD> Intraparenchymal monitor
✅ Main indication: deteriorating neuro status
@NeurocritCareJ @ProvencioJavier @ESCMID 8/ Here are some of their findings:
🐈 scans:
⛔ reliable indicators of ICP
☠ if demonstrating ICP elevation, patients had worse outcome
This makes sense to me as CT is not a sensitive marker of ICP elevation so if you are waiting for CT changes, you may be late to the game…
🐈 scans:
⛔ reliable indicators of ICP
☠ if demonstrating ICP elevation, patients had worse outcome
This makes sense to me as CT is not a sensitive marker of ICP elevation so if you are waiting for CT changes, you may be late to the game…
@NeurocritCareJ @ProvencioJavier @ESCMID 9/ ICP management:
Only 1 trial compared CPP 🎯 vs. ICP 🎯 (ie., lower ICP vs. augment MAP) and found that CPP targeted management was superior and reduced 👂loss!
Most studies lacked standardized therapeutic approaches.
1 study used #LundConcept
Only 1 trial compared CPP 🎯 vs. ICP 🎯 (ie., lower ICP vs. augment MAP) and found that CPP targeted management was superior and reduced 👂loss!
Most studies lacked standardized therapeutic approaches.
1 study used #LundConcept
@NeurocritCareJ @ProvencioJavier @ESCMID 10/ What is the #LundConcept? From University of Lund, Sweden, focuses on “volume-targeted” strategy and regulation of vol of 🧠compartments.
If transcapillary 💧 exchange is regulated by hydrostatic (-) colloid pressure, then when the #BBB is injured, 👆CPP will cause > edema.
If transcapillary 💧 exchange is regulated by hydrostatic (-) colloid pressure, then when the #BBB is injured, 👆CPP will cause > edema.
@NeurocritCareJ @ProvencioJavier @ESCMID 11/ So management focuses on:
🧮 ⬇ MAP/CPP by using beta1 and alpha2 agonist
🧮 ⬇ intracap hydrostatic pressure via vasoconstrictive properties of thiopental and dihydroergotamine
🧮 Maintain colloid osmotic press by RBC/albumin
🧮 Euvolemia to slightly negative via diuresis
🧮 ⬇ MAP/CPP by using beta1 and alpha2 agonist
🧮 ⬇ intracap hydrostatic pressure via vasoconstrictive properties of thiopental and dihydroergotamine
🧮 Maintain colloid osmotic press by RBC/albumin
🧮 Euvolemia to slightly negative via diuresis
@NeurocritCareJ @ProvencioJavier @ESCMID 12/ This concept is certainly interesting but not well validated.
Back to the paper:
☠ ranged from 0-67%
ICP monitoring, in >1 study, was associated with better outcomes!
CSF diversion, whether #EVD or #LD was superior to conventional therapy
Back to the paper:
☠ ranged from 0-67%
ICP monitoring, in >1 study, was associated with better outcomes!
CSF diversion, whether #EVD or #LD was superior to conventional therapy
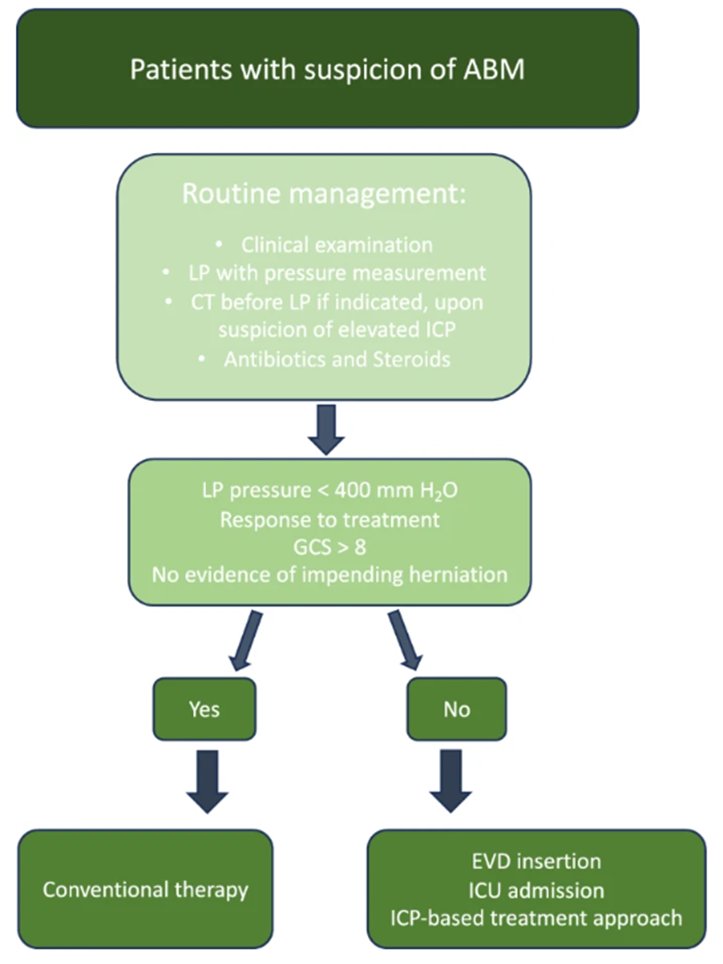
@NeurocritCareJ @ProvencioJavier @ESCMID 13/ Could this be a true signal and could monitoring help to improve outcomes and mortality? If so, could this be extended to non-invasive monitoring too? The authors did suggest a new algorithm based on their findings too:
@NeurocritCareJ @ProvencioJavier @ESCMID End/ What else did you learn from the paper? 🎩 off to the authors for their contribution to the field!
Let me know if you have any questions, corrections, suggestions, or if you have seen an article @neurocriticalcarej that you would like me to feature!
Let me know if you have any questions, corrections, suggestions, or if you have seen an article @neurocriticalcarej that you would like me to feature!
@NeurocritCareJ @ProvencioJavier @ESCMID @neurocritcareJ @aartisarwal @caseyalbin @JimmySuhMD @JimSiegler @MicieliA_MD @a_charidimou @EricLawson90 @CajalButterfly @Capt_Ammonia @DrAtulRamesh1 @RamaniBalu1 @DSandsmarkMDPhD @PennNeurology @TJUHNeuroCrit @namorrismd @ShadiYaghi2 @MDNeurocritcare @HopkinsNCCU
@NeurocritCareJ @ProvencioJavier @ESCMID @aartisarwal @caseyalbin @JimmySuhMD @JimSiegler @MicieliA_MD @a_charidimou @EricLawson90 @CajalButterfly @Capt_Ammonia @DrAtulRamesh1 @RamaniBalu1 @DSandsmarkMDPhD @PennNeurology @TJUHNeuroCrit @namorrismd @ShadiYaghi2 @MDNeurocritcare @HopkinsNCCU @neurochristiana @nirmalregency @interneurona @MicieliA_MD @oneDRwoman_ @OGdukeneurosurg @AvrahamCooperMD @LorenzoPinelli @daniel_gewolb @medinariojaMD @neurona_critica @PulmCrit @drdangayach
Loading suggestions...